![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
34 Cards in this Set
- Front
- Back
|
Seizures
|
Clinical manifestation of an abnormal & excessive excitation of a population of cortical neurons
|
|
|
Epilepsy Definition
|
- “a disorder of the brain characterised by an enduring predisposition to generate epileptic seizures”
- “occurrence of at least one unprovoked seizure” which is in contrast to an older definition which required at least two unprovoked seizures - unprovoked tendency towards recurrent seizures |
|
|
Focal Seizures
|
› Focal (partial) - Activation of neurons in a relatively small, discrete region
- Clinical manifestation reflects region of brain in which they occur - Sensory or motor - Complex partial seizures – impairment of consciousness (once diencephalon is involved loss of conciousness) - Familiarity (déjà vu) or strangeness (jamais vu), automatisms, hallucinations (auditory and visual), temporal lobe epilepsy can be a developmental focal umour tht can spread and cause generalised tonic clonic |
|
|
Generalised Seizures
|
› Generalised - Characterised by involvement of both hemispheres and
widespread neuronal activation - Tonic – extension of the extremities, rigid stretching - Atonic – sudden loss of muscle tone - Clonic (Myoclonic) – repetitive muscle twitching - Tonic-clonic (grand mal) – distinct tonic phase followed by a clonic phase (full body spasms with intermittent relaxation) - Generalised absence seizures (petit mal) –brief lapse of consciousness |
|
|
Not all antiepileptic drugs are anticonvulsants
|
-
|
|
|
Mechanisms of Anticonvulsants
|

1. Enhance Na+ channel inactivation
- reduce firing frequency of neurons 2. Inhibit excitatory amino acid release - block Ca2+ or K+ channels 3. Enhance GABA action 4. Inhibit GABA breakdown 5. Inhibit GABA uptake |
|
|
Na Channel Inactivation
|
- use dependent
- red. of sustained high-fq firing APs, specifically act on rapid firing neurons phenytoin, carbamazepine & lamotrigine |
|
|
Inhibit Excitatory amino acid release
|
- used for generalised absence seizures
- T-type Ca2+ channel blokcer Ethosuximide |
|
|
Valproate
|
Mech 1, 2 & 4
its Mech 4 action lead to newer generation anticonvulsants research |
|
|
Enhance GABA actions
|
Act at GABAa
- increase affinity for GABA - inc. Cl- conductance - prolongs open time of the channel UNWANTED sedative side effects Phenobarbitone, BZDs (BZDs bind at the interface between alpha and gamma subunits) |
|
|
Inhibit GABA breakdown
|
- vigabatrin
- synthetic structural analogue of GABA - specific inhibtor of GABA-Transaminase |
|
|
Inhibit GABA Uptake
|
Tiagabine- derivative of nipecotic acid (transportable inhibitor)
- GAT1 inhibitor |
|
|
Mechanism unknown
|
Gabapentin and pregabalin
|
|
|
Genetics of Epilepsy
|
› Since the first “gene” to cause epilepsy was discovered in 1995, more than 25 different genes have been found
› Virtually all known mutations that cause epilepsy are found in ion channel subunits |
|
|
EEG
|
Display of fluctuations in voltage which occur over the scalp generated by postsynaptic potentials in cortical neurones.
- normal EEG doesnt exclude epilepsy - if normal repeat after sleep dep. |
|
|
Aetiology
|
Infancy & childhood
–Birth injury –Inborn error metabolism –Congenital malformn. Childhood & adolescence –Idiopathic/genetic syndrome (idopathic not caused by anything and so by inference genetic) –CNS infection Adolescence & young adult –Head trauma Older adult –Stroke –Brain tumor 1. cortical dysplasia (classical trauma @ frontal eye fields) |
|
|
Childhood absence epilepsy
|
peak onset 6-7 years, girls > boys
–family history of epilepsy –Absences very frequent EEG, 3Hz spike and wave complexes, »clinical seizures produced by hyperventilation remission in approx. 80% by adolescence –generalised tonic clonic seizures, 20-40% –ethosuximide, valproate, lamotrogine |
|
|
Juvenile myoclonic epilepsy
|
–age of onset, 12-16 years
»myoclonic seizures, early morning occurrence »generalized (clonic-)tonic-clonic seizures, 90-95% »absence seizures occur in 10-33% of cases VALPORATE drug of choice |
|
|
Genetic Contribution to epilepsy
|
Risks are greater for generalised than focal epilepsies
–Generalised epilepsies: risk to sibs ~ 10% –Focal epilepsies: risk to sibs < 5% –Febrile seizures: risk to sibs ~ 8% |
|
|
Twin Studies
|
»“idiopathic” epilepsy syndromes (genetic);
eg. Childhood Absence Epilepsy »monozygotic 70.2%, dizygotic 7.5% »Structural focal epilepsy (acquired); eg. Head injury, encephalitis, tumour »monozygotic 10.8%, dizygotic 5.6% |
|
|
Channelopathies
- simple inheritance (only account for a small proportion of epilepsy syndromes) |
VG Channelopathies
Ligand Gated Channelopathies Non-Channel genes |
|
|
Laceration to lateral margin of tongue specific to what seizure?
|
Tonic clonic
|
|
|
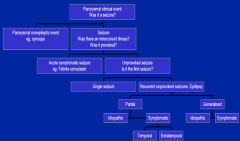
Questions for a first seizure?
|
Seizure or not?
Seizure type? –focal onset, postictal deficits Evidence of CNS dysfunction? –school, work, hemiparesis, PMH Any precipitating factors? What investigations to order? Do we start an AED? What precautions to advise? |
|
|
Seizure Precipitants
|
Low (less often, high) blood glucose
Low sodium, calcium, magnesium Stimulant/other proconvulsant intoxication Sedative withdrawal Severe sleep deprivation |
|
|
Evaluation of a first seizure
|
History, physical
Blood tests: FBC, electrolytes, glucose, Ca, Mg, hepatic and renal function Lumbar puncture only if meningitis or encephalitis suspected (CT scan) Urine drug screen Electroencephalogram CT or MR brain scan |
|
|
Relapse Rate after 1st seizure
|
wide range from studies, pooled data 51%
most recurrences in 1st year, usually 3-6mo Predictive factors –idiopathic (32%) vs remote symptomatic (57%) »abnormal exam, structural lesion on CT/MRI –abnormal EEG, epileptiform (58%) –partial seizures, especially remote symptomatic Relapse rate is reduced by AED treatment |
|
|
AIMS of AED Tx
|
Choose appropriate medication
–valproate for generalised seizures Use a single drug, monotherapy –simplifies treatment, reduces adverse effects Make the patient seizure free –without dose related side effects if seizures recur, increase dose –maximal tolerated dose –need to observe for 2-3x usual seizure interval |
|
|
Prognosis
|
70% have a good prognosis for control of seizures and remission
–better for idiopathic than symptomatic –better for generalised than partial 20% need regular medication and may have breakthrough seizures 5-10% poorly controlled |
|
|
Convulsive Syncopy
|
is common and often miss Dx as epilepsy
|
|
|
Syncopy DDx Seizure
|
Precipitating factors
Light-headed, tinnitus limp fall, convulsive movements brief rapid recovery no incontinence or tongue bite Normal EEG |
|
|
Seizure DDx Syncopy
|
Supine, sleep
Aura, CPS tonic clonic evolution duration minutes postictal confusion (often wake up in hosiptial bed not knowing how they got there) muscle soreness, injury, lateral margin tongue bite Abnormal EEG |
|
|
DDx Seizures
|
Seizure
Syncope Migraine Cerebral ischaemia Movement disorder Sleep disorder Metabolic disturbance Psychiatric disturbance |
|
|
Refractory seizure disorder
|
Review the diagnosis
–are the seizures epileptic? Review the medical therapy –compliance with medication? –adequate trials of AEDs? Consider alternatives to medical therapy –epilepsy surgery in partial seizure disorders |
|
|
Epilepsy surgery
|
Failure of antiepileptic medication
–Trials of different drugs, >2 often predicts refractory seizures –Identify epileptic focus; »Video EEG, MRI, PET, SPECT –show it could be removed safely Temporal lobectomy Focal cortical resection of frontal, parietal or occipital lobes |

