![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
87 Cards in this Set
- Front
- Back
|
How are the family Enterobacteriaceae divided?
|
28 Genera - by morphology, biochem & DNA relatedness
128 Species - bichemistry & DNA relatedness Strains serotyes - antigens biotypes - biochemisty these two relate to divergence from common ancestor Phagetypes - random division method PCR - not used as muach as could be as does not follow spp's biochem divisions |
|
|
What pathogenic genera are contained in the Enterobacteriaceae family?
|
Morganella
Serratia Citrobacter Edwardsiella Enterobacter more imp Klebsiella Shigella Proteus Esherichia Salmonella Yersinia |
|
|
Which four Enterobacteriaceae are important when considering VPH?
|
Salmonella
E. coli Yersinia Shigella |
|
|
How would you go about initially isolating & catergorising Enterobacteriaceae?
|
Grow on Fresh blood agar & MacConkey bile lactose agar plates under aerobic & anaerobic conditions.
(bile lactose differentiates lactose fermentors) |
|
|
Why grow clinical sample on both Blood agar and MacConkeys Bile lactose agar plates?
|
Blood agar non selective
MacConkeys - selective for Enterobacteriaceae, as tolerate bile and differentiates lactose fermentors. |
|

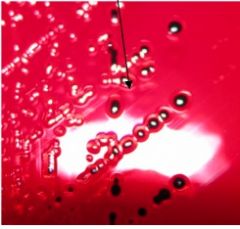
What is the significance of the colour changes on this MacConkey bile lactose agar plate?
|
Lactose fermentation = acid prod = RED
- LAC+ve, coliforms -pink E.coli, Klebsiella, Enterobacter AA decarboxylation = alkali = YELLOW - LAC -ve, non coliforms - yellow Salmonella, Shigella, Proteus, Yersinia |
|
|
List general differential features of Enterobacteriaceae family.
|
Grow in presence of bile
Non sporing Facultative anaerobes med sized (0.3-1 x 1-6uM) |
|
|
List general non differential features of Enterobacteriaceae family.
|
All Gram -ve, straight rods
some motile, some not (peritrichous flagella) med sized (0.3-1 x 1-6uM) both catalase +/-ve spp Simple nutritional needs. |
|
|
Salmonella selective media such as brilliant green agar (brown) as it is ---------- of other Enterobacteriaceae & differential.
Coliforms = ? Non coliforms = ? |
suppressive
yellow / green mostly red |
|
|
Enrichment broths use toxic agents such as -------- or ------------ which are ----- to different ---- to select one wish to grow.
|
Selenite (salmonella selctive), tetrathinate
toxic spp |
|

What colony morphology is seen in this growth on a BLA?
What is it indicative of species wise and why? |
Small butyrous like dk pink colonies
E.coli Klebsiella & Enterobacter colonies are larger, mucoid and pale pink |
|
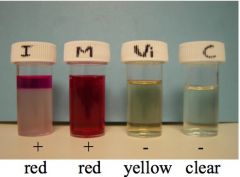
The IMViC test pattern seen above is indicative of which enteric bacteria?
|
E. coli
Klebsiella & enterbacter are -ve for I & M & +ve for Vi & C |
|
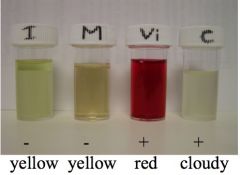
What do the initials IMViC stand for?
|
Indole
Methyl Red Voges Proskauer Citrate |
|
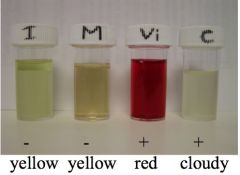
The IMViC test pattern seen above is indicative of which enteric bacteria?
|
Klebsiella & enterbacter
E. coli are +ve for I & M & -ve for Vi & C |
|
|
How must you grow your bacteria to test for motility by the hanging drop method and which genus of enteric coliform bacteria can be differentiated from one another post an IMVic test by this method?
|
Must be grown in broth
Klebsiella -ve motility Enterbacter +ve motility |
|
|
How would you proceed from genus ID to species level?
|
Lysine decarboxylase & urease tests.
|
|

The urease, H2S & lysine decarboxylase tests can be used to distinguish both -------- & --- -------- genus of enteric bacteria.
|
coliform & non coliform
Urease H2S Lysine decarboxylase Shigella - - - Salmonella - most + most + Proteus + most + most + Yersinia + - - |
|
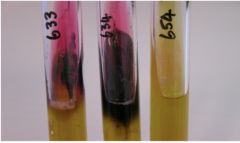
Combination media as seen above have speeded identification, they use TSI or XLD what is this?
|
Triple sugar Iron agar
Xyline, Lysine, Deoxycholate agar |
|

If you saw this on a plate what genus of non coliform enteric bacteria would you know is present?
What else would confirm this identification? |
Proteus - as it swarms across BA plate (not MacConkeys)
Smell note of caution it may obliterate other growing colonies of diff spp/ genus |
|
|
Which non coliform enteric bacteria are motile and non motile?
|
Motile Non motile
most Salmonella shigella Yersinia @22deg C Yersinia @ 37deg C change in motility may reflect dislike of conditions. Chicken salmonella spp lost motility. |
|
The image above shows a XLD agar plate what does this distinguish between?
|
Fermentation method - red if acidic
Black = H2S production lysine decarboxylase activity deoxycholate - bile sensitive so restricts to enteric |
|

What tests would be used to further speed up / identify pathogen spp?
|
Commercial biochemistry kits as shown in image
quick 4hrs growth in media post 24 hour isolation plate Immunological - ELISA /RIA but requires an idea of what expecting to see Genetic tests not commonly used , only major pathogens [DNA] limiting |
|
|
Regional reference labs will -------- enteric bacteria.
What Ag are there for E.coli and Salmonella respectively? |
serotype
O, H, K, & F O, H. |
|
|
Where are E. coli O, H, K & F Ag located?
|
O = sugar side chain of LPS (>170)
H = flagellar protein (>56) K = capsular polysaccharide (>80) F = fimbrial proteins serotype designations are V specific, >1000 i.e. O139: K82 : H2 |
|
|
Which O serotypes of salmonella are pathogenic to animals?
|
A-I
agglutination with Ab = +ve i.e. S. enteriditis O;1,9,12 H (comensal ) |
|
|
What would be a better approach / more logical to strain identification of bacterial spp then serotyping?
|
Genetic testing for toxicity genes
as specific toxin is related to dz seen & treatment. |
|
|
What is the relevance of using polyvalent O & H antiserum?
|
polyvalent O antiserum contains all animal pathogenic Ag's so +ve = pathogenic
polyvalent H antiserum contains all H Ag's agglutination = +ve for motility so know not chicken spp salmonella |
|
|
Monovalent O & H antisera +ve agglutination allows….
|
individual strain id
H antisera identifies diff flagella types some salmonella strains capable of switching type for immune avoidance. Chickens spp non motile =>> pathogenicity Enteriditis = 1 type of flagella Others 2 types of flagella. |
|
|
What system of salmonella classification is currently used?
|
Le Minor & Popoff Scheme
1 spp - S.enterica Bergey's Manual 1994 - 2 spp - S. enterica -S bongori (10 serotypes, non path & reptile) |
|
|
Name one enteric bacterial obligate pathogen that causes dysentery in humans & primates?
How is it identified |
Shigella
S. sonneri & S. flexneri most common incubation 1-7 d, usually 48hrs O serotype & toxin assays |
|
|
How is Shigella pathogenic?
|
Attaches GIT epithelium @ M cells of peyers patch
induced endocytosis from GIT epithelium invasion of lymph nodes via macrophages engulfing escape lysis by prevention of acidification of vacuole Toxin Shiga toxin - reduces protein synthesis S. dysenteriae Endo toxin -increases vascular permeability, inflammation & fever - water loss / red water reabsorption |
|
|
How is shigella spread, treated and prevented?
|
in fecal matter
carrier status can last for months in humans supportive therapy - fluid replacement antibiotics highly ?? as self limiting vaccination, reduce spread & improve hygiene |
|

Proteus is a human / animal GIT commensal where else is it found and what diseases is it important in ?
|
soil & water
Otitis externa - dogs & cats, v v common UTI - dogs & Eq Diarrhoea - young most spp Surgical problems - GIT contents spillage |
|

What 2 spp of Proteus are commonly seen in vet medicine?
|
P. vulgaris & P. mirabilis
|
|

What virulence determinants are important in Proteus infections?
|
Adhesins & Endotoxin possibly not definitively known
Urease imp in bladder infections - alters pH causing epithelium damage |
|

What serotypes are used to Id proteus strains?
|
O & H
|
|

How would you treat / prevent Proteus infections?
|
Antibiotics
No vaccines Hygiene / aseptic technique |
|

Klebsiella pneumoniae is found in whiat spp and where?
|
humman & animal
GIT commensal also soil, water, hands, instruments Mucoid on plate |
|

Important Klebsiella pneumoniae dz's include….
|
Wound infection
- joint navel, foals & lambs - wounds in man Mastitis - post parturition esp on wood bedding UTI's - dogs Pneumonia - foals Genital tract infection - horse - male short term - female long term & abortion |
|

Virulence determinants in Klebsiella pneumoniae are
|
Fimbrial adhesins
Capsule Endotoxin Siderophore Steric hindrance of complement Mucoid on plate |
|

What serotypes are used to ID Klebsiella pneumoniae strains?
|
K 77-82
Mastitis - many K Ags Meritiis - 1, 5 & 7 (mares) Pneumonia - 1, 2 & 3 (humans) Mucoid on plate |
|

How do you treat / prevent Klebsiella pneumoniae?
|
Antibiotics
No commercial vaccine Hygiene, good aseptic technique Mucoid on plate |
|
Where is Yersinia pseudotuberculosis found, spp etc?
|
soil - worldwide
GIT - wild mammals esp rodents, - birds, - domestic animals |
|
In what spp / locations are Yersinia pseudotuberculosis commonly seen?
|
Captive rodents / birds
Zoo animals Humans Domestic animals (stress related?) |
|
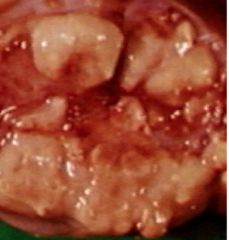
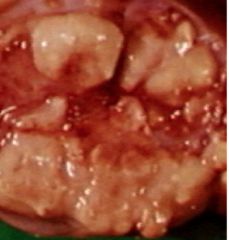
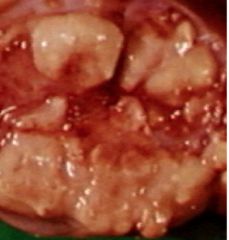
How does Yersinia pseudotuberculosis present, what serotypes are used to ID and how is it treated / prevented?
|
TB like - caseous lymph nodes,
- necrotic lesions in lung O & H serotypes Antibiotics No commercial vaccines |
|
|
Rank in order of virulence
S. flexneri S. dysenteriae S. boydii S. sonnei |
S. dysenteriae - most Shiga toxin, most severe gastroenteritis
S. boydii & S. flexneri - less toxin, less severe S. sonnei |
|
|
What is Y. enterocolitica imp in VPH and why this spp?
|
main source of food poisoning from pigs.
can proliferate at fridge temps (better then listeria) O3 & O9 serotypes most common Specifically inhabits pig tonsils !! less common also in soil & GIT of domestic & wild spp. |
|
|
What are the virulence determinants for Yersinia pseudotuberculosis & Y. enterocolitica?
|
GTPase regulator
attachment invasion superantigens - stimulate T cells - cytokine release opsinisation neutralisation Y. enterocolitica only het stable enterotoxin |
|
|
How does Y. enterocolitica cause disease?
|
As Yersinia pseudotuberculosi
Bacteria adhere to gut mucosa, destroys cells lining the gut. An enterotoxin (YST), which is stable in hot (121oC) and cold conditions, is produced but its role is unknown. Results in relatively mild infection (5-14 days), abdominal pain (pseudo-appendicitis), fever, diarrhoea; nausea and vomiting rare; but can cause septicaemia in the immuno-compromised. |
|
|
What serotype would you ID Y. enterocolitica strains by
|
O
O8 & 9 - humans O9 - also Brucella abortus |
|
|
How would you treat Y. enterocolitica infections?
|
Antibiotics
may cull due to persistence No commercial vaccine availabe |
|
|
E. coli dz's spread via ------ ----- contamination.
They are both ---------, obligate & ------------- pathogens |
Faecal oral
commensals, obligates & opportunistic |
|
|
E. coli is commonly seen in the following dz's
|
Wound infections
surgical problems UGT infections Udder infections Mastitis most common G-ve cause V common & serious |
|
|
E. coli is a non specific dz because….
|
endotoxin damages teat reducing milk yield for months.
|
|
|
Obligate pathogenic E.cloi is associated with 2 types of dz what are they and there modes of action?
|
Enteritits and / or Septicaemia
Ingestion Ingestion Diarrhoea Invasion -> shock ->Death <2d Dehydration Deposition, joints, meningies Death <3 days Death < few days |
|
|
E. coli Enteritis / septicaemia dz types are affected by…...
|
Serotype
some -> enteritis only some -> enteritis & septicaemia some -> septicaemia only Host spp Predisposing factors age / immunocompromised newly weaned (maternal Ab loss) poor hygeine |
|
|
What 6 categories of obligatory pathogenic E-coli serotypes are there?
|
ETEC - Enterotoxigenic - toxin producing
VTEC - Verotoxigenic (VHEP in humans) bloody diarrhoea AEEC - Attaching & Effacing EIEC - Enteroinvasive Unclassified Necrotoxigenic - new high mortality rate |
|
|
What serotypes are expressed by ETEC E.coli?
|
ETEC binds to Fimbrial adhesins found on GIT colonic epi cells
host spp expression variation = strains host specificity i.e F4 (K88) - piglets & horses F5 (K99) - piglets, calves, lambs |
|
|
What common dz's are caused by ETEC and in what spp?
|
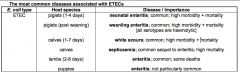
see image
|
|
|
What specific enterotoxins are associated with ETEC E. coli?
|
ST - heat stable
LT - heat labile affect Na pump = watery diarrhoea as reduces H2O reabsorption. |
|
|
What serotypes are expressed by VTEC E.coli?
|
VTEC binds to Fimbrial adhesins & pther adhesins found on GIT colonic epi cells
|
|
|
What specific enterotoxins are associated with VTEC E. coli?
|

Verotoxins - shiga like
VT1, VT2 & VT2e VT2e - face and neck swelling prevent protein production in host cell of membrane bound proteins => red H2O reabsorption. |
|
|
What common dz's are caused by VTEC E.coli in what spp?
|
post weaning piglets -
weanling enteritis; as for ETEC but less common oedema disease; quite common; acute and chronic forms; high mortality; N.B. no enteritis Calves 1-7d - white scours; as for ETEC Rabbits - enteritis; common; high mortality |
|
|
What common dz's are caused by AEEC E.coli in what spp?
|
enteritis - rare; some deaths
|
|
|
What common dz's are caused by EIEC E.coli in what spp?
|
Calves - septicaemia; high mortality
Lambs (1-3d) - septicaemia (watery mouth); hi mortality foals - septicaemia; common, hi mortality, 25% all deaths |
|
|
What common dz's are caused by unclassified E.coli?
|
Mushy chick dz - egg infected in ovaries or post laying
total body inflammation = fatal Chicken septicaemia - inhalation of faecal matter - invasion from lung to blood - acute form high mortality - chronic granulomatous dz intestines / mesentery Hjarre's dz's |
|
|
What virulence factors are used by AEEC E. coli?
|
Fimbrial attachment
Intimin & Initimin receptor toxins ??? not yet identified |
|
|
What virulence factors are used by EIEC E. coli?
|
Adhesins
Surface proteins - parasite induced endocytosis / uptake Enzymes - escape endosome Capsule / outer membrane proteins limit phagocytosis & opsinisation Siderophores Endotoxin over activate Complement Toxic shock Death of young |
|
|
Obligate pathogenic E. coli infections are ID'd by….
|
Fimbrial Ag & toxins
Fluorescent Ab tests & PCR |
|
|
Obligate pathogenic E. coli infections are treated by …...
|
Antibiotics where not resistant
Palliative - fluid / electrolyte therapy |
|
|
Obligate pathogenic E. coli infections are prevented by….
|
Good husbandry
susceptible to UV, drying & disinfectants Vaccines ( fimbrial proteins /toxins) Neonate; passive or active immunisation |
|
|
Salmonella reservoirs incude….
|
GIT humans, mammals, birds, reptiles
|
|
|
Salmonella serotypes are ---- adapted & --- ---- adapted.
Adaptation is --- ------ |
host, non host
i.e. host adapted - S. Dublin, S. Pullorum non adapted - S. Typhimurium not absolute almost all serotypes can affect humans excpet poultry adapted, S.pullorum |
|
|
Salmonellosis can be either --------- or -----------
|
Enteritis or septicaemia
|
|
|
Enteritis salmonellosis manifests via…..
|
Motility leads to contact
Fimbrial mediated adherence Parasite induced endocytosis, inflammation Endosome survival - catalase activity Endotoxin & cell damage Adenylate cyclase activation & inflammation cellular infiltrate large |
|
|
Septicaemic salmonellosis manifests via…..
|
Fimbrial mediated adherence
Parasite induced endocytosis, inflammation Endosome survival - catalase activity Deeper invasion - blood stream Endotoxic shock, +/- deposition Joints -arthritis / osteomyelitis Placenta / foetus - abortion Brain - meningitis Lungs - pneumonia edotosaemia induced ischaemia in claves hind limbs/ tail/ ears = terminal dry gangree in calves |
|
|
The type of dz seen in salmonella infections depends on ….
|
Virulence determinants
Innate & adaptive host defences Interaction of these factors Primary infection subclinical | clinical | chronic recover | local invasive | enteritis septicaemia sub clinical clinical | shedders |
|
|
What sources of Salmonella infection in animals are ther?
|
Environmental
Milk from carriers Infected hosts / convalescent hosts / carriers Vertical transmission from infected breeding stock |
|
|
How do Salmonella outbreaks occur?
|
not common
an individual infected animal joins susceptible herd / flock Contaminated feed / water shedding from rodents protein supplements - most common source |
|
|
How does Salmonella spread in reptiles & birds differ?
|
Fecal - oral spread
vertical transmission - via eggs Salmonella diverged from E.coli @ dinosaur point in evolution. |
|
|
Human Salmonella infections in humans are usually ...
|
Food borne
infected source animal / bird infected food handler / utensils S. Typhimurium - in all spp S. Enteritidis - in poultry Beware imported eggs & poultry not vaccinated. |
|
|
Salmanellosis is diagnosed by what types of testing?
|
Biochemical
Serotypes Biotypes Phage types Flourescent Ab staining of faecal matter / PM tissues |
|
|
In Salmonellosis fecal samples are often -----------
|
polymorphic
|
|
|
To carry out serological testing ideally you need to do ----- / ----------- tests and carry these out against ------ sera from both ----- & ------------ stages or the dz. Ideally you would test the ---- not ---------.
The problem with single sera testing is….. |
ELISA / agglutination
paired acute & convalescent herd / flock not individuals Gives many false +ve |
|
|
How would you control Salmonellosis in animals?
|
Good husbandry
Vaccines - inactivated & live Competitive exclusion - feed pooh from herds / flocks free of dz causing |
|
|
How would you control Salmonellosis in humans?
|
Break chain of infection
clean water food hygiene sewage disposal |
|
|
What similarities & differences are there in treating enteritic & septicaemic Salmonellosis?
|
Similarities
good nursing Fluid / Electrolyte replacement Differences Enteritis - antibiotics probably contra indicated in enteritis as selects for inc resistant & inc virulence salmonella strains & kills comensals Speticaemia Antibiotics indicated, parenteral admin |

