![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
Bacterial diarrhea usually involved the _______ bowel and usually results from a __________ released by the colonizing bacteria.
|
-small bowel - secretory
-toxin |
|
|
Deaths from diarrhea usually occur in what group?
|
Children under 5
|
|
|
Normal bacteria/flora vary by ____________ and _____________.
|
-Site in the body - different nutrients, pH
-host - age, gender, culture, sexual habits |
|
|
Name 4 benefits of normal flora.
|
-protect against pathogenic bacteria (produce antimicrobial substances)
-produce vitamins and nutrients, help digest food -helps maturation of intestine -builds up innate immune system |
|
|
What is one drawback of having normal flora?
|
Can be a potential source of pathogens
|
|
|
Name the normal organisms of the: stomach, small intestine
|
-stomach - Helicobactor pylori
-small intestine - sterile |
|
|
90% of the bacteria found in the colon are ___________________.
|
anaerobes (10% facultative anaerobes)
|
|
|
Treatment with broad spectrum antibiotics can put an individual at risk of infection by what two bacteria?
|
-Clostridium difficile
-Enterococcus faecalis or VRE (vancomycin resistant enterococcus) |
|
|
How does Clostridium difficile infection occur?
|
-enterotoxin spores in the gut germinate and the drug resistant organism takes over
|
|
|
What things are important in assessing a potential bacterial infection?
|
-symptoms - vomiting, diarrhea, dysentery
-timeframe relative to consumption -history - other cases, types of foods eaten, medications, travel |
|
|
The number of bacteria required to cause diarrhea in a patient is called what?
|
Infectious dose
|
|
|
What is quorum sensing?
|
-method of communication by which bacteria sense other bacteria of the same or different species and decide which genes they need to activate/where to set up based on it
|
|
|
Entry for all bacterial, diarrhea causing enteropathogens is by what route?
|
Oral
|
|
|
Name 3 organisms with a low infectious dose (<100 organisms). Why do they all have a low infectious dose?
|
-Shigella dysenteriae
-E. Coli 0157:H7 (EHEC, STEC) -Campylobacter -they are acid tolerant |
|
|
Bacteria use __________ to move and penetrate the mucus layer covering the intestine.
|
Flagella
|
|
|
The first step in bacterial colonization is adherence, which is mediated by the ______.
|
pilus (pili)
|
|
|
Bacteria can colonize ____________ and form biofilms or _____________ in immune cells and invade the blood stream and other organs.
|
extracellularly; intracellularly
|
|
|
How do bacteria produce damage (5 mechanisms)?
|
-toxins (endotoxins and secreted exotoxins)
-invasion of the epithelium -damage from injected effectors -inducing inflammation -inducing apoptosis |
|
|
What portion of gram negative bacteria is an endotoxin?
|
The lipid A portion of LPS
|
|
|
A gram negative, rod-shaped bacterium that is motile by a single polar flagellum and lives a symbiont in algae and marine invertebrates
|
Vibrio cholera
|
|
|
What serogroups of cholera are responsible for human disease?
|
O1; O139
|
|
|
What component of the bacterium do these serogroups refer to?
|
The antigen of the LPS coat
|
|
|
How is cholera acquired?
|
-fecal contaminated water
-contaminated seafood |
|
|
What are the symptoms of cholera?
|
-secretory diarrhea - colonizes the small bowel
-rice-water stools -severe dehydration -shock and death |
|
|
V. cholerae has a ________________________ which acts as a receptor for a bacteriophage encoding the Cholera Toxin genes (encounters the phage in the environment).
|
Toxin coregulated pilus (TCP)
|
|
|
V. Cholerae also uses the TCP to colonize what area of the GI tract by bacterial aggregation and biofilm formation?
|
Small bowel
|
|
|
The major virulence factor of V. Cholerae is what? What is its structure?
|
-Cholera Toxin
-5B subunits (pentamer) and 1A subunit |
|
|
The _______ subunit binds with GM1 and creates a pore for entry into the cell, while the _____ subunit is responsible for activity once inside.
|
-5B subunit - entry
-A subunit - active component |
|
|
The A subunit acts by upregulating ___________________, promoting massive secretion of electrolytes.
|
cAMP (activates adenylyl cyclase)
|
|
|
T/F The cholera toxin initiates tissue damage to the small bowel.
|
False - no tissue damage
|
|
|
Treatment for cholera is...
|
oral or IV fluid and electrolyte replacement
|
|
|
T/F There is a vaccine for cholera.
|
True - 2 vaccines
|
|
|
Organism which causes bowel inflammation, vomiting, cramps and watery diarrhea; found in raw seafood and in coastal seawater; causes cruise ship outbreaks; common in Japan
|
Vibrio parahemolyticus
|
|
|
E. coli that are commensal are gram-_______________, lactase- _______________ bacilli. They help provide what vitamin?
|
-gram negative, lactase positive
-Vitamin K |
|
|
Good E. coli can acquire pathogenicity from what 4 methods to become pathogenic?
|
-transposons
-pathogenicity islands -plasmids -phages |
|
|
A major cause of diarrhea in children and some adults; also a cause of traveler's diarrhea; causes a cholera-like diarrhea
|
Enterotoxigenic E. Coli (ETEC)
|
|
|
ETEC produces 2 potent toxins; what are they?
|
-Heat-labile toxin (LT)
-Heat-stabile toxin (ST) |
|
|
How is ETEC acquired?
|
-fecal contaminated food or water
|
|
|
ETEC adheres to and colonizes the __________ ____________ with multiple pili types called colonization factors.
|
Small bowel
|
|
|
Treatment for ETEC is...
|
Oral rehydration therapy
|
|
|
T/F Cholera toxin B subunit antibodies can protect against LT type ETEC.
|
True
|
|
|
Which toxin associated with ETEC is similar in structure and mechanism of action to cholera toxin? What is its mechanism?
|
-LT - heat labile toxin
-5B subunits and 1A subunit - 5B binds to GM1 receptor and A subunit upregulates adenylyl cyclase, increasing cAMP |
|
|
What is the structure of the ST toxin? What is its mechanism of action?
|
-Small peptide
-upregulates guanylate cyclase, increasing gCMP |
|
|
T/F Tissue damage is not a feature of ST or LT toxin action.
|
True - no tissue damage
|
|
|
Both LT and ST toxin increase _______ and ______ secretion and inhibit ______ absorption (electrolytes).
|
-Cl- and H20 secretion
-Na+ absorption |
|
|
________________ is commensal in farm animals but only causes disease in humans.
|
E. coli O157: H7
|
|
|
How do commensal E. coli O157:H7 become Enterohemorrhagic E. coli (EHEC)?
|
They encounter a bacteriophage encoding the Shiga toxin genes (from Shigella dysenteriae)
|
|
|
EHEC affects what area of the GI tract? What symptoms does it produce?
|
-large intestine
-mild diarrhea, and in some individuals bloody diarrhea |
|
|
A sequelae of EHEC traveling in the gut to the kidney is what?
|
-Hemolytic uremic syndrome (HUS)
(usually affects very young and elderly; shiga toxin binds to Gb3 receptors in the kidney damaging blood vessels and occluding glomeruli) |
|
|
What constitutes the triad of symptoms that define HUS?
|
-acute renal failure
-thrombocytopenia -hemolytic anemia |
|
|
What is the structure of the shiga toxin?
|
-5B and 1A subunits
-B - binds to Gb3 -A - an N-glycosidase which affects protein synthesis |
|
|
T/F EHEC has a low infectious dose.
|
True
|
|
|
How does EHEC adhere to the colonic mucosa? What is the "hallmark of EHEC infection" that relates to this?
|
-Tir-intimin interaction - injection of Tir via the type 3 secretion system, binds to intimin on outer surface
-forms attaching and effacing lesions (once adheres injects effectors that form pedestals, disrupt tight junctions, increase permeability) |
|
|
EHEC can be found in what food sources?
|
-Meat (hamburger), salads and veggies (spinach), water
|
|
|
T/F Washing affected spinach will remove EHEC.
|
False - bacteria from feces of animals attach to stomata and penetrate to internal tissues of the spinach
|
|
|
T/F Antibiotics should be used to treat EHEC.
|
False - exacerbate the release of more toxin
|
|
|
A human-only pathogen that produces watery diarrhea in children below 1 year; produces microcolonies tethered by bundle-forming pili
|
EPEC - enteropathogenic E. coli
|
|
|
What part of the GI tract is affected by EPEC?
|
Small bowel
|
|
|
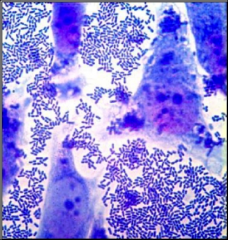
A cause of persistant diarrhea (>14 days) among HIV/AIDS patients in the US and an emerging pathogen in developing countries; causes characteristic aggregative adherence pattern on host cells
|
EAEC (enteroaggregative E. coli)
|
|
|
EAEC
|
|
|
How does EAEC adhere to colonic mucosa?
|
-AAF - aggregative adherence fimbriae
|
|
|
What toxins are associated with EAEC?
|
SHet and PET
|
|
|
Clinical features of EAEC?
|
-watery, mucoid, persistant diarrhea
(induces mucus production and feeds on it) -blood rarely present -fecal leukocytes and IL-8 - indicators of mucosal inflammation -no fever or vomiting |
|
|
Uses type 3 Secretion system to cause intestinal AE lesions, adheres via Tir-intimin interactin and bundle forming pilus, watery diarrhea in children 0-12 months of age
|
EPEC
|
|
|
Produces shiga toxins, bloody diarrhea, hemorrhagic colitis, intestinal AE lesions, and can lead to kidney failure (HUS)
|
EHEC (STEC; E. Coli O157:H7)
|
|
|
Aggregative, emerging in the US, several toxins, produces biofilms, induces mucous production and persistant mucoid diarrhea
|
EAEC
|
|
|
Produces dysentery (blood and pus in stool) similar to shigella
|
EIEC
|
|
|
Produces cholera-like disease in adults and children, profuse, watery diarrhea, due to ST and LT toxins, adheres to small bowel via several pili called colonization factors
|
ETEC
|

