![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
Upper lip anatomy
What is the primary muscle? What is it's nerve & blood supply? |
Orbicular oris muscle
Nerve: CN VII Blood: superior labial artery (runs deep to the muscle) - branch of facial artery |
|
|
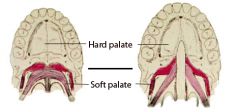
Palate anatomy
What are the structures in the primary & secondary palate? |
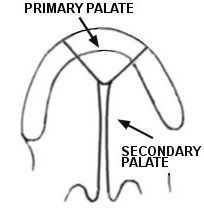
Primary palate - includes alveolar ridge & hard palate anterior to the incisive foramen
Secondary palate - includes hard palate posterior to the incisive foramen & soft palate |
|
|
Palate anatomy
What are the muscles of the palate? Name the nerves that supply each one & their actions. |
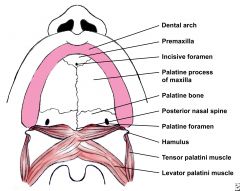
1) Tensor veli palatini (CN V3) - opens eustachian tube, tenses soft palate.
2) Levator veli palatini (pharyngeal plexus) - elevates palate 3) Uvularis (pharyngeal plexus) - moves uvula upward & forward 4) Palatopharyngeus (pharyngeal plexus) - draws palate downard |
|
|
Palate anatomy
What is the primary arterial supply to the hard & soft palates? |
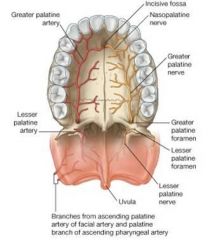
Hard palate - greater palatine artery
Soft palate - descending palatine branch of the internal maxillary artery; ascending palatine branch of the facial artery, palatine branch of the ascending pharyngeal artery, lesser palatine artery |
|
|
Embryology of the lip & palate
Critical embryologic window for facial development is the first ___ weeks of gestation. |
12
|
|
|
Embryology of the lip & palate
Critical gestational period for lip development is from __ to __ weeks How about palate development? |
Lip - 4 to 6 weeks
Palate - 8 to 12 weeks |
|
|
Embryology of the lip & palate
Does development occur in anterior to posterior fashion or posterior to anterior? |
anterior to posterior
|
|
|
The five facial prominence's appear around the __________ early in the fourth week of gestation.
What are the five facial prominence's? |
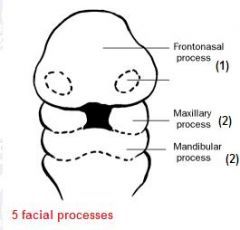
stomodeum (primordial mouth)
A) Frontonasal prominence B) Paired maxillary prominences C) Paired mandibular prominences |
|
|
The ____________ is formed by the fusion of the medial nasal prominences.
What does it develop into? |
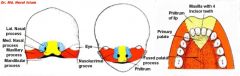
Intermaxillary segment
Develops into the nasal tip, columella, central upper lip/philtrum, and (includes central maxillary alveolar ridge, maxillary incisors, and the hard palate anterior to the incisive foramen) |
|
|
The lateral lip is formed when what two things fused?
|
maxillary prominences & the medial nasal prominences
|
|
|
How is the secondary palate formed?
|
The maxillary promiences form shelf-like processes that fuse anterior to posterior.
|
|
|
What creates a clefting of the primary palate?
|
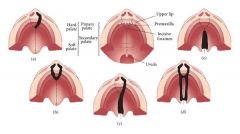
lack of fusion between the medial nasal promience and the maxillary prominence.
|
|
|
What creates a clefting of the secondary palate?
|
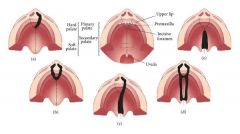
lack of fusion between the maxillary prominence to the contralateral maxillary prominence
|
|
|
List some environmental factors linking to clefting
|
1) Anticonvulsant meds
2) Retinoic acid derivatives 3) Folic acid antagonists or deficiency 4) Cigarette smoking 5) Fetal alcohol exposure 6) Pregestational maternal diabetes |
|
|
What percentage of cleft lip (with or without cleft palate) is considered nonsyndromic?
|
70%
|
|
|
What percentage of cleft palate only is considered nonsyndromic?
|
30%
|
|
|
Mutations on which gene may contribute up to 12%of the genetic etiology for cleft lip/palate?
|
IRF6 gene mutation on chromosome 1q32
|
|
|
Which syndrome Is classically associated with the triad: micrognathia, glossoptosis and U-shaped cleft palate?
|

Pierre Robin sequence
|
|
|
What is the distribution of:
Cleft lip with palate Cleft palate only Cleft lip only |
Cleft lip with palate - 45%
Cleft palate only - 30% Cleft lip only - 25% |
|
|
What percentage of clefts are unilateral & bilateral?
|
Unilateral - 80%
Bilateral - 20% |
|
|
Cleft lips are more common on the left or right?
Cleft lips are more common in males or females? |
2/3rd are LEFT sided
2/3rd are MALE |
|
|
Cleft palates are more common in males or females?
|
2/3rd are FEMALE
|
|
|
What are the key components of classifying clefts?
|
Detailed description of the following elements: lip, palate, unilateral, bilateral, complete, incomplete
|
|
|
Which clefts, lips +/- palates, or isolated cleft palates vary incidences across ethnicites?
|
Cleft lips +/- palates vary incidences across ethnicities
Isolated cleft palates are uniform across ethnicities |
|
|
What are the 3 main degrees of lip clefts?
|
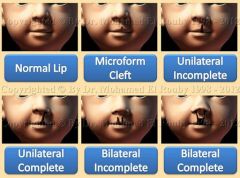
1) Microform cleft
2) Incomplete cleft 3) Complete cleft |
|
|
Which cleft lip does this describe?
Dehiscence of the orbicularis oris muscle without overt clefting of the epidermis, creating a notching at the vermilion |

Microform cleft
|
|
|
Which cleft lip does this describe?
Dehiscence of the epidermis, orbicularis oris muscle, and mucosa. Nasal floor and sill are intact. |

Incomplete cleft
|
|
|
Which cleft lip does this describe?
Dehiscence of the epidermis, orbicularis oris muscle, and mucosa extending into the nasal floor. |
Complete cleft
|
|
|
Describe submucosal clefts
|

A type of palatal clefts, where there is intact mucosa with underlying dehiscence of palatal musculature.
Classical physical findings are: - bifid uvula - Zona pellucida (hyperlucent gray line in the midline of the soft palate) - Notch in the posterior palate at midline - Risk for velopharyngeal insufficiency |
|
|
Which palatal cleft does this describe?
Dehiscence of the mucosa and palatal musculature posterior but does not fully extend through the entire secondary palate (or primary palate if there is a cleft lip) |
Incomplete cleft palate
|
|
|
Which palatal cleft does this describe?
Dehiscene of the mucosa and palatal musculature and does fully extend through the entire secondary palate (and primary palate if there is a cleft lip) |
Complete cleft
|
|
|
What are Tessier clefts?
|
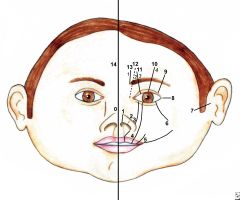
Clefts may involve the mouth, cheeks, eyes, ears and forehead and may continue into the hairline. These craniofacial clefts are often referred to as Tessier clefts.
They are numbered from 0-14 to indicate the location and extent of the cleft using the mouth, nose and eyesockets as landmarks, with the midline designated 0. These more extensive conditions may also be described anatomically, such as “oro-occular cleft” and “fronto-nasal dysplasia.” |
|
|
What are some presurgical orthopedic techniques that can be performed to narrow the cleft or reshape the nose?
|

1) Nasoalveolar molding (NAM) - very involved and requires weekly visits to the prosthodontist for remolding the appliance. (it's thought that the neonatal cartilage is "moldable" up to the first 6 weeks of life)
2) Taping: requires compliance from the family to properly apply tape across the cleft tightly. Taping will not address the nasal deformity. |
|
|
Unilateral cleft lip
What is the muscle defect? |
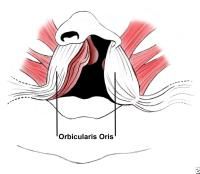
Dehiscence of the orbicularis oris with abnormal attachments to the alar base & columella
|
|
|
Unilateral cleft lip
Which way is the displacement of the nasal ala on the cleft side? |

Nasal ala on the cleft side is displaced inferiorly, laterally, and posteriorly
|
|
|
Unilateral cleft lip
What are the differences in sizes of the lateral & medial cruses, & lower lateral cartilages on the cleft & noncleft side |

Lower lateral cartilages - same on both sides
Medial crus - on the cleft side it is shorter Lateral crus - on the cleft side it is longer |
|
|
Unilateral cleft lip
Why is the columella and caudal septum displaced to the noncleft side? |
Caused by the pull of the abnormally inserted orbicularis muscle.
|
|
|
In complete cleft lips, what happens to the nasal floor?
|
it is absent
|
|
|
What is the timing of surgical repairs of unilateral cleft lips? (rule of 10's..)
|
>10 weeks
>10 Hgb >10 lbs |
|
|
Describe the surgical repair technique for unilateral cleft lip
|
1) Release of the orbicular oris from its abnormal attachments and recreation of the sphincter.
2) Lengthening the cleft lip to equal the length of the upper lip on the noncleft side 3) Symmetric alignment of the alar base (this can be dificult secondary to deficiency of the skeletal structure on the cleft side) 4) Closure of the nasal floor and sill 5) Meticulous realignment of the vermilion-cutaneous border at the cleft repair site and restablishing the "white roll" 6) Camouflage of the incisional scars 7) Primary rhinoplasty may be utilized to address the nasal deformity. |
|
|
List the three most widely used techniques for unilateral cleft lip repair.
|
1) Millard rotation-advancement repair (46%)
2) Modified rotation advancement (38%) 3) Triangular flap technique (9%) |
|
|
Bilateral cleft lip
What happens to the muscle fibers and vermilion in the prolabial segment? |
they are both absent
|
|
|
Are bilateral cleft lip repairs typically performed as a single stage procedure?
|
Typically yes, but it can be staged at least 3 months apart with repairing the widest cleft first.
|
|
|
Cleft palate
What is the defect in the velopharyngeal sling? |
The levator veli palatini muscle abnormally attach to the posterior margin of the hard palate, instead of interdigitating at midline.
|
|
|
Early aggressive palatal surgery may impact _________, however, delayed palatal surgery may result in significant _________
|
midface growth
speech disorders |
|
|
What is the most common site of fistula formation post-palatoplasty?
|
junction of the hard palate-soft palate
|
|
|
What are the three main types of cleft palate repair techniques?
|
1) Straight-line closure
2) Double opposing Z-plasty 3) Schweckendiek two-stage palatoplasty repair |
|
|
What are the three types of straight-line closure techniques for cleft palate?
|
1) Two-flap palatoplasty (Bardach)
2) Bipedicled-flap palatoplasty (von Langenbeck). 3) V-Y pushback palatoplasty (Veau-Wardill-Kilner). |
|
|
Describe the two-flap palatoplasty (Bardach) straight-line closure procedure
|

Two posteriorly based mucoperiosteal flaps based off of the greater palatine arteries.
Shortens palatal length Easy visualization of the arterial pedicles Used for wide clefts Single staged |
|
|
Describe the bipedicled-flap palatoplasty (von Langenbeck) straight-line closure procedure
|
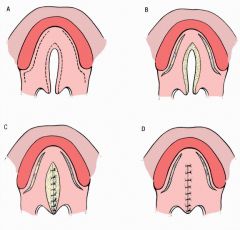
Attached anteriorly & posteriorly
Blood supply from both anterior & posterior attachments Blinded dissection around the greater palatine artery pedicles. Shortens palatal length Used for more narrow clefts Single staged |
|
|
Describe the V-Y pushback palatoplasty (Veau-Wardill-Kilner) straight-line closure procedure
|
Lengthens the palate
Used for wide clefts Single staged |
|
|
Describe the doule opposing Z-plasty palatoplasty (Furlow)
|

Most commonly used for submucosal and soft palate clefts
For complete palatal clefts, the Furlow technique may be used to close soft palate and combined with straight-line hard palate closure technique. Best technique for reestablishing the levator veli palatini into its normal horizontal sling orientation Significantly lengthens palate When velopharyngeal insufficiency persists after a straight-line closure palatoplasty, a revision Furlow palatoplasty may improve speech prior to pharyngeal surgery. Single staged |
|
|
Describe the Schweckendiek two-stage palatoplasty repair
|
Closes the soft palate cleft and leaves the hard palate repair until the maxilla or palate is more developed.
A prosthetic obturator is used to obstruct the oronasal communication until time of hard palate repair. Poor compliance with the children wearing the obturator leads to poor speech development. Not a frequently used technique Two-stage repair. |
|
|
What are some otologic associations with cleft patients?
|
- 95% of cleft pt's have chronic otitis media with effusion
- Poorly fnct tensor veli palatini (due to its defective attachment) contributes to poor pressure equalization - Increased nasopharyngeal reflux from the cleft may exacerbate middle ear dz - Ventilation tubes are often placed at the time of lip repair. - Ear dz typically improves with age and after palatal repair |
|
|
What are some swalling associations with cleft patients?
|
- Not able to create suction or create a seal around nipple
- Use modified nipples that ease the flow and create less need for suction - Popular cleft nipple or bottles include: Pigeon, Haberman, and Mead-Johnson bottles - Cleft babies need to be burped more frequently |
|
|
What & of cleft pt's have speech difficulties?
|
25%
|
|
|
What is the initial treatment for VPI?
|
Intensive speech therapy for at least 6 months.
Failure to improve with 6-12 months of speech therapy may indicate need for surgical intervation. |
|
|
If a pt with VPI has had intensive speech therapy but is not a good candidate for surgical intervantion, what can you do to improve VPI?
|
dental obturator
|
|
|
Children with this syndrome often have persistent VPI even after surgical intervention.
|
Velo-cardio-facial syndrome
|
|
|
Good anterior-posterior wall motion with poor lateral wall closure classically is repaired via ___________________
|
Orticochea spincteroplasty (aka sphincter pharyngoplasty)
|
|
|
Good lateral wall motion with poor anterior-posterior wall motion is classically is repaired via ___________________
|
posterior pharyngeal flap
|

