![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
Rates of effectiveness for current contraception methods:
|

|
|
|
Traditional tubal occlusion:
|
A surgical procedure (either by minilaparotomy or laparoscopy).
Requires a small abdominal incision and general or regional anesthesia. Occlusion techniques include tying (ligating) and blocking with mechanical devices, such as clips or rings and cauterizing. Typical failure rates are less than 1%. |
|
|
Newer method of tubal occlusion (microinsert):
|
Newer tubal occlusion: transcervical sterilization
A new nonsurgical tubal occlusion method called Essure (manufactured by Conceptus, Inc.) became available in US in 2002. Essure is a micro-insert that dynamically expands and occludes the fallopian tubes. It is placed inside the proximal section of the fallopian tube in a half-hour procedure, using a hysteroscopic technique. By 3 months, both tubes are closed in 96% of women. By 6 months, 100% of women have both tubes closed. The procedure is performed in an outpatient setting, under local anesthesia. After 2 years of follow-up, no pregnancies have been reported thus far after Essure placement. Longer f/u reveals rare chance of pregnancy, comparable to other forms of tubal sterilization. Mechanism of Action: First, the expandable outer coil is responsible for acute device anchoring; second the device provides both space filling and mechanical blockage of the tubal lumen; and finally the tissue lining the fallopian tube grows into the device, completely occluding the tube and anchoring the device. Candidates: Women who want permanent birth control and are willing to use another birth control method for the first 3 months after the procedure, and who have a medical condition that precludes general anesthesia. For women with medical conditions such as heart disease and obesity microinsert procedure may be safer, partly because of routine use of local anesthesia. Some of these women are ineligible for conventional tubal sterilization. Advantages: Because no incision is necessary, it's less invasive, women have less discomfort and recover faster, and the absence of a scar preserves their privacy. Contraindications: Is uncertain about her desire to end fertility. Is pregnant or suspects she is pregnant. Has delivered a baby, had a miscarriage, or had an abortion within 6 weeks before microinsert procudre. Has an active or current pelvic infection. Has an inaccessible, technically difficult uterus and fallopian tubes Has a know allergy to contrast medium. Has a known hypersensitivity or allergy to nickel confirmed by a skin test. Is unwilling to use another birth control method for the first 3 months. Is unwilling to return 3 months later for a procedure to check for the microinsert placement. Has a previous tubal ligation. Disadvantages: The need for backup birth control and possibility of experiencing regret are two patient disadvantages to transcervical sterilization. Counseling: Patients need to use another contraceptive method for 3 months after insertion. HSG is done at 3-month follow-up appointment. Patients need to know that they should notify any health care professionals about their microinsert prior to any intrauterine procedures. |
|
|
Name a major risk factor and a condition that risk is reduced for associated with tubal occlusion:
|
Risk factor: Ectopic pregnancy
Decreased risk: Ovarian cancer |
|
|
Copper T IUD:
|
The arms of the Copper-T IUD are wrapped with copper wire, which acts as a functional spermicide. There is clear evidence that IUDs are not abortifacients. They prevent pregnancy by preventing fertilization.
The Copper-T IUD is approved for 10 years of use; however, efficacy lasts 12 years or more. Mechanism of Action: Cooper-containing IUDs reduce the motility and viability of the sperm and the development of ova. Research shows that sperm counts found in the cervical mucus and uterine tube are much lower in women using IUDs than those in nonusers. A clinical study found that women using copper-containing IUDs had uncoordinated contractions, which suggests that the device may act by hindering sperm transport. Candidates: Women who desire long-term contraception. Women who do not want the systematic effects of hormones. Women who desire a quickly reversible method Advantages Fertility returns rapidly after removal of the copper IUD. There is no ongoing cost after insertion. The Cooper-T IUD may be associated with a decreased risk for endometrial cancer, but the exact mechanism for this association is unclear. Contraindications (WHO Criteria): Puerperal sepsis Immediate post-septic abortion Unexplained vaginal bleeding before evaluation Malignant gestational trophoblastic disease Cervical cancer awaiting treatment (when IUD initiated) Endometrial cancer Uterine fibroids with distortion of the uterine cavity Distortion of the uterine cavity Current PID (when IUD initiated) Current STI (when IUD initiated) Known pelvic TB (when IUD initiated) Disadvantages: Menstrual changes The Copper T IUD can increase the duration and amount of menstrual flow and menstrual cramping. Expulsion is rare, occurring in only 5% of users, but the most likely cause of IUC failure. Expulsion is most common within the first three months after insertion Uterine perforation is a rare complication of IUC, occurring approximately once every 770 to 1600 insertions. Perforation generally occurs at insertion, when a portion of the device becomes embedded in the uterine wall. There’s a possible increased risk of PID during early postinsertion period in women with cervical infections. Studies suggest that women with chlamydial infection or gonorrhea at the time of IUD insertion were at an increased risk of PID relative to women without infection. The absolute risk of PID was low for both groups (0-5% for those with STIs and 0-2% for those without). Counseling: Inform women that IUDs do not cause an increased risk of STIs, tubal infertility, and ectopic pregnancies. Describe how to check for the string, follow-up visits, and warning signs. |
|
|
Levonorgestrel Intrauterine System (LNG IUS):
|
LNG IUS reservoir releases 20 mcg LNG/day initially. Rate decreases to 10 mcg/day after 5 years.
Approved for 5 years Data demonstrates effective for up to 7 years Mechanism: thickens cervical mucus (inhibits sperm motility and function) High LNG levels also causes endometrial atrophy Markedly decreased menstrual flow Amenorrhea (absence of bleeding) in 20% of women at 1 year of use LNG IUS requires an office visit for insertion and an office visit for removal. Mechanism of Action: LNG IUS thickens the cervical mucus and inhibits sperm motility and function. The endometrial atrophy that is a consequence of the high endometrial levels of LNG leads to a substantial decrease in menstrual flow and absence of bleeding in some women who use this form of intrauterine contraception. It is important to some patients that the LNG IUD mechanisms of action are all before conception. It prevents fertilization rather than disrupts implantation (a common misconception). The low ectopic pregnancy rate relative to pregnancy rate suggests that an anti-implantation effect is not the primary contraceptive mechanism of action of the device. Candidates: All women of reproductive age who are seeking a long-term, highly effective contraceptive. IUD is especially appropriate for: Women who are looking for a convenient method Women with menstrual symptoms that may improve with LNG IUS, Similar to long-acting, progestin-only DMPA, use of the LNG IUS generally improves menorrhagia, dysmenorrhea, and anemia; decreases the risk of PID and ectopic pregnancy relative to non-use; and has been used as a treatment for menorrhagia. Lactating women Advantages: Use of the LNG IUS may reduce menstrual symptoms in women with uterine fibroids or adenomyosis, thereby reducing the need for hysterectomy. Data from the United Kingdom also suggest that use of the LNG IUS may reduce the occurrence of benign endometrial polyps in patients who have breast cancer and are taking tamoxifen. Can be used by lactating women. |
|
|
What are some contraindications to use of an IUD?
|
Current pelvic infection (treat, wait 3 months before insertion)
Current purulent cervicitis or GC/CT infection at time of insertion Unexplained vaginal bleeding Malignant GTD Cancer of the cervix, endometrium or breast (for LNG IUS only) Uterine distortion (makes insertion difficult, but possible to use) Known pelvic tuberculosis |
|
|
Implanon (implant):
|
Single rod implant consisting of 68mg etonorgestrel
Failure rate is 0.05% Must be removed within 3 years of insertion Bleeding, amenorrhea common Spotting (50% decreasing to 30% after 6m) Amenorrhea (20%) Frequent irregular bleeding (<10%) Unpredictable bleeding pattern over time Implanon, an etonogestrel implant, is used by more than 2 million women in European and Asian countries and is now available in the United States. One rod is 40 mm x 2 mm and its core is 40% ethylene vinyl acetate (EVA) and 60% etonogestrel. It has a rate-controlling membrane of !00% EVA Because contraceptive implants do not contain estrogen, they can be used during lactation as soon as six weeks postpartum. This feature may be especially attractive to women with young infants who want highly effective contraception that does not require daily action. The effectiveness of Implanon in overweight women has not been determine; women who weighed more than 130% of their ideal body weight were not studied. Mechanism of Action: The single-rod implant continues to rely on ovulation inhibition over the entire duration of use. To protect against pregnancy after 3 years, the health care provider must remove the rod and insert a new rod. Candidates: In addition to its high efficacy rate and long-term effectiveness (3 years), it has rapid reversibility. After the etonogestrel implant is removed, most women (94%) ovulate by 3 months, the majority within 3 weeks. Advantages: This method is a particularly good choice for women who do not want a daily or weekly action, desire a discreet method (it is nearly invisible), or want to use contraception during lactation. According to studies with lactating women, there are no negative effects on nursing or infant growth or development with etonogestrel implant. This method also can confer noncontraceptive benefits, such as improved dysmenorrhea and acne. Contraindications: Known or suspected pregnancy Current or past history of thrombosis Hepatic tumor or active liver disease Undiagnosed abnormal genital bleeding Known or suspected carcinoma of the breast or history of breast cancer Hypersensitivity to the components of the implant Disadvantages: The most common side effect of implant is bleeding irregularities, including infrequent bleeding (26.9%), amenorrhea (18.6%), prolonged bleeding (15.1%), and frequent bleeding (7.4%). But as with other progestin-only methods, it is the variability and unpredictably of the bleeding that is most characteristic of this method; for example, a bleeding pattern may change from one 2 to 3 month period to the next. Unfortunately, studies on progestin-only methods have not identified a simple approach for managing bleeding. However, one study found that ethinyl estradiol may help control bleeding during the first few months of implant use. Other side effects include weight gain (2.3%), emotional lability (2.3%), headache (1.6%), acne (1.3%), and depression (1.0%). There is no evidence of long-term effects such as decreased bone mineral density (BMD) and deep vein thrombosis, or anemia with the etonogestrel implant. On the contrary, lumbar spine BMD improved in studies. Both procedures are rapid: insertion takes 1 minute and removal takes 3 minutes. Counseling: During patient counseling, address misperceptions about implants, such as visibility of the implant, low libido, excessive hair growth, and they break off in the arm. There are no data to support or refute these misperceptions but after more than two decades of implant use worldwide, these issues have not been reported by even a small percentage of users. To decrease chances of unintended pregnancy, a quick start method can be used. With this method, the impleant can be inserted any time after a negative urine pregnancy test. Another test will need to be done in 3 weeks to make sure the woman was not pregnant when the implant was inserted. Counseling women about bleeding patterns and other side effects helps prevents early discontinuation. |
|
|
Combined oral contraceptives:
|
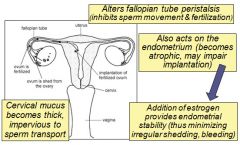
Mechanism of Action:
The progestin in COCS is the main actor in preventing pregnancy. It suppresses the secretion of gonadotropin (mainly leutinizing hormone) by the pituitary gland. The estrogen primarily inhibits follicle-stimulating hormone secretion. The estrogen also works synergistically with the progestin to affect the uterine lining and cervical mucus production. Candidates: Women with dysmenorrhea and menorrhagia Women who want to regulate menses Women who will use a daily method consistently Advantages: Contraindications: Multiple risk factors for arterial cardiovascular disease, such as smoking, diabetes, hypertension Known thrombogenic mutations Current or history of current ischemic heart disease History of stroke History of or current deep venous thrombois or pulmonary embolism Vascular disease Complicated valvular heart disease Hypertension (systolic ≥160 or diastolic ≥ 100) Smoking (>10 cigarettes/day and age 35 or older) Migraine headache with aura Major surgery with prolonged immobilization Current breast cancer Active viral hepatitis Severe cirrhosis Benign or malignant liver tumors Breastfeeding <6 weeks postpartum Disadvantages: Obesity may impair the effectiveness of COCs. Counseling: Breakthrough and /or irregular bleeding is the primary cause of discontinuation among new users. Other side effects include breast tenderness, nausea, and bloating. Many of these side effects usually disappear after the first few cycles of pill use. After breakthrough bleeding, breast tenderness and nausea are the leading causes of discontinuation. There is less likely to be side effects, such as nausea and breast tenderness, with low-dose pills. In fact, the incidence of these side effects is approximately 50 percent lower in users of 20 ug pills compared with a 35 ug pill. But the lower the dose the more likely breakthrough bleeding will occur. Even though weight gain is a primary concern of women using OCs, research shows that use of OCs does not substantially affect body weight for most women. Fear of side effects, such as weight gain and nausea, is often the reason women discontinue COC. Emphasize that side effects abate with time. Women also fear risks, such as breast cancer and venous thromboembolism. Review their risks. Breast cancer: There is confusion regarding the risk of breast cancer and OC use. Many women think that the findings of the Women’s Health Initiative regarding combination (estrogen/progestin) hormone replacement therapy apply to all hormones. Recent high-quality observational data from the Women’s Contraceptive and Reproductive Experiences (CARE) Study provide reassuring evidence that OC use does not increase breast cancer risk. The relative risk was 1.0 (95% CI = 0.8–1.0) for current OC users and 0.9 (95% CI = 0.8–1.0) for former users. These findings were not changed by duration and dosage of OC use, timing of use, age at use, or risk status based on family history. Likewise, a pooled analysis of data from WHO and New Zealand trials of DMPA found no overall increase in breast cancer risk. Weight gain: Pooled data from two, 6-cycle, multi-center, double-blind, placebo-controlled trials showed that 2.2% of 228 OC users and 2.1% of 234 placebo users reported weight gain. Likewise, a Cochrane Review of all English-language randomized controlled trials of at least 3 treatment cycles’ duration noted that 3 placebo-controlled trials found no evidence to support a causal association between combination OCs or a combination skin patch and weight gain. [Note: Redmond data were not included.] Their overall conclusion was that there was insufficient evidence to determine the effect of combination OCs on weight, but that no large effect was evident. In actual practice, however, clinicians appreciate that the effects of hormonal contraception on weight will vary from patient to patient, depending on a variety of physiological and lifestyle issues. Venous thromboembolism: Use of combination OCs increases the risk of thromboembolism. However, the annual risk is low (1.0–3.0 per 10,000 women) and approximately half that associated with pregnancy (5.9 per 10,000). Obesity and use of COCs are independent risk factors for venous thromboembolism. Another common concern is that OCs cause heart attack and stroke. This risk is related to the presence of other risk factors, especially smoking. In fact, OC use does not increase the risk of myocardial infarction or hemorrhagic stroke among healthy nonsmokers under age 35 who do not have other risk factors for these events, and is associated with only a slight increase in the risk of ischemic stroke. |
|
|
MOA of estrogen in OC:
|
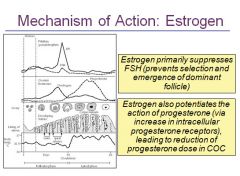
Estrogens increase globulin secretion including angiotensinogen. Note also that an increase in aldosterone secretion leads to fluid retention
|
|
|
1st, 2nd and 3rd generation progesterones:
|
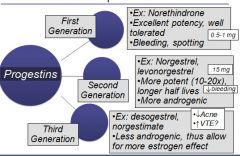
Third generation: Norgestimate FDA-approved for treatment of acne (mechanism: allows more estrogen effect leading to significant increases in SHBG which in turn increases the binding of free testosterone). On the other hand, concern was raised that increased estrogen may be associated with increased risk of venous thromboembolism
|
|
|
4th generation progesterone:
|
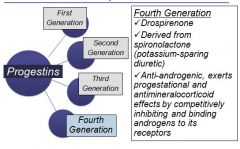
Newer formulations:
Yasmin (EE 30 mcg/drospirenone 3 mg): adolescents with acne and hirsutism may benefit from its use. Potassium levels should periodically be checked (note: patients with known hyperkalemia should not use Yasmin; patients on medications that may raise serum potassium levels [e.g., NSAIDs, heparin, potassium-sparing diuretics] should have their serum potassium checked in the first cycle of use) Yaz (EE 20mcg/drospirenone 3 mg): consists of 24 days of active pills with only 4 days of inactive pills. This shortened hormone-free interval leads to lighter periods. Yaz is effective in treating premenstrual dysphoric disorder (PMDD), the most severe form of PMS. Again, potassium levels need monitoring as above |
|
|
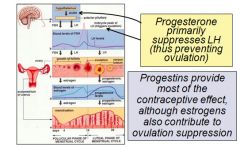
MOA of progesterone part 1:
|
|
|
|
MOA of progesterone part 2:
|
|
|
|
Transdermal patch:
|
Beige-colored patch applied once per week for 3 weeks, followed by one patch-free week
Must start using on Day1 of cycle (if not, use backup for first 7 days) Slight decrease in efficacy in women over 198 pounds Adherence Patch contains 9 days medication Issue: VTE risk, questionable possible increase First available in US in 2002. The weekly transdermal contraceptive patch (Ortho Evra) is applied once a week to the abdomen, buttock, upper outer arm, or upper torso. The patch delivers 150 g of norelgestromin/20 g of ethinyl estradiol daily to systemic circulation. Serum concentrations of norelgestromin and ethinyl estradiol within the range generally seen with oral norgestimate 250 g/ethinyl estradiol 35 g are maintained for up to 10 days, suggesting that clinical efficacy would be maintained even if a scheduled change is missed for as long as 2 full days. The contraceptive efficacy of the transdermal patch is comparable to that of combination OCs. In clinical trials, fewer than 3% of patches were replaced due to partial (2.9%) or complete (1.8%) detachment. Adhesion is not affected by heat, humidity, or exercise. Women who want an easy, nondaily method. Women with dysmenorrhea and menorrhagia Women who are concerned about interference with nausea or vomiting. Advantages: Weekly form of birth control Rapid reversibility Contraindications : Same as those for combination OCs. Disadvantages: Side effects are similar to COC’s side effects. Because the patch contains estrogen and progestin, side effects associated with its use are probably similar to OCs, although more study is needed. A 2008 publication of a Cochrane Database sytematic review determined that compared to COC users, patch users were more likely to report breast discomfort, dysmenorrhea, nausea, and vomiting, but that patch users had better compliance than OC users. These side effects usually dissipate within the first 2 months of use. Increased exposure to estrogen, which may increase the risk of side effects Application site reactions. Breast tenderness. Breast tenderness is greater in the first few cycles of use and dissipates over time. Contraceptive failures may be increased among women weighing 90 kg (198 lbs) or more. Counseling: Educate patient on application and removal of patch Avoid placing patch in areas that receive a lot of friction, such as bra straps Place on buttocks, abdomen, upper torso (excluding breasts), or upper arm Apply to clean, dry skin Once removed, fold patch closed to reduce release of hormones Do not flush in the waste system. Dispose of it in the garbage |
|
|
Nuva Ring:
|
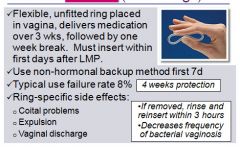
|
|
|
Nuva Ring part 2:
|
The vaginal contraceptive ring (NuvaRing) was approved by the FDA in 2001; became available in US in 2002.
Ring is flexible, transparent, and colorless to nearly colorless. Ring comes in one size that fits most women; no fitting is required. One ring is inserted into the vagina per cycle and is to remain in place continuously for 3 weeks, followed by a ring-free week. When inserted, the ring delivers ~ 120 g of etonorgestrel and 15 g of ethinyl estradiol/day to the systemic circulation over a 3-week period. After insertion, maximum serum concentrations of etonorgestrel and ethinyl estradiol are achieved in approximately 1 week and show a gradual linear decline thereafter. Women not previously using hormonal contraception should insert the ring on or before day 5 of the cycle, counting the first day of menstruation as day 1. Back-up contraception is recommended for the first 7 days of ring use. Women switching from a combination OC may insert the ring any time within 7 days after the last combined estrogen/progestin OC and no later than the day that a new cycle of pills would have been started. No back-up method is needed. Consider “Quick Start” method with the ring. Candidates: The vaginal ring is an appropriate method for women who desire the convenience of a 3-week regimen, as well as those who have difficulty using a method that requires daily attention. Women who want to regulate their periods. The hormonal benefits of the vaginal ring are similar to those of the contraceptive skin patch and pill. Clinical trials with the vaginal ring were not designed to assess specifically the impact of heavier body weight on contraceptive efficacy. Therefore, no data are available regarding the efficacy of the vaginal contraceptive ring in women of heavier body weight. Ring improves vaginal flora, leading to reduced frequency of bacterial vaginosis. A multicenter trial showed a low incidence of gastrointestinal problems, such as nausea and vomiting. Advantages: Convenient, once a month use Privacy Cycle control, few women experience untimely spotting or bleeding Contraindications: Same as those for combination OCs (except those related to intestinal absorption problems0 Significant pelvic relaxation Vaginal obstruction Unable to touch genitalia Disadvantages: Possibility of leukorrhea and vaginitis Hormone-related side effects associated with use of the vaginal ring, such as headache and nausea, are similar to those seen with OCs, although more study is needed. Local adverse effects associated with use of the vaginal ring include leukorrhea, vaginitis, and a slight risk (1%) of device expulsion. The ring is rarely felt during intercourse. Because the vaginal ring contains estrogen and progestin, contraindications for its use are similar to those for OCs. Counseling: The ring is easy to insert; there is no wrong way to insert it. The ring can be placed anywhere in the vagina, but the deeper it’s placed, the less likely it will be felt. After 3 weeks, remove the ring for one week and then insert a new ring. Patients need to be cautioned that the ring can be inadvertently expelled from the vagina while removing a tampon or during bowel and bladder emptying, especially with straining or constipation. Often women are not aware that the device has been expelled. If the ring falls out, it should be rinsed with warm water and reinserted within 3 hours. |
|
|
Combined Oral Contraceptive benefits:
|
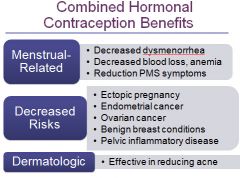
Most users of COCs have reduced menstrual flow and dysmenorrhea.
COCs reduce the risk of ovarian cancer by 40-80% after ~ one year of use and decrease the risk from 10-12% annually thereafter. (Burkman) Even after discontinuing COC use, protection continues for 15-20 years. COCs reduce the risk of endometrial cancer by 40-50%, and like ovarian cancer, protection increases with duration of use. Studies demonstrate 90 percent protection from ectopic pregnancy with current OC use. A reduced incidence of benign breast disease--including fibrocystic changes and fibroademomas has been consistently shown. Three multicenter, randomized, placebo-controlled trial have demonstrated COC’s effectiveness in reducing acne. |
|
|
Combined oral contraceptive risks and side effects:
|
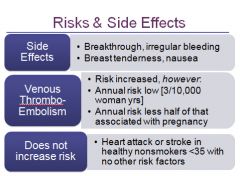
|
|
|
Risk of Cervical and Breast cancer with COC usage:
|
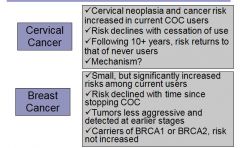
|
|
|
Contraindications for COC use:
|
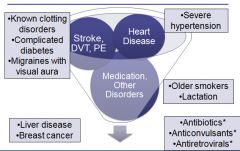
Known clotting disorders: Factor V Leiden, Prothrombin G20210A Variant, Protein C, Protein S,
Complicated diabetes: nephropathy, neuropathy, retinopathy. If without vascular complications, may use (benefits/risks) Antibiotics: Controversial. Several studies fail to confirm association (pencillins, tetracycline, doxycline, ciproflxacin, ofloacin). Anticonvulsants: reduced efficacy,, affects phenytoin, phenobarbital, primidone, carbamazepine |
|
|
Progesterone only OC:
|
Called the “mini-pill”
Two formulations: norethindrone and norgestrel Mechanism: suppresses ovulation, thickening of cervical mucus Consistent use critical: miss dose by >3 hours, use back-up contraception for 48hrs Similar benefits to COC, fewer risks, only contraindication is breast cancer Good for women who cannot use estrogen Often called “mini-pills,” progestin-only pills are a good contraceptive choice for women who can’t use estrogen. There are currently two formulations--norethindrone (Micronor, each pill contains .35 mg of norethindrone) and norgestrel (Ovrette), each pill contains .075 mg of norgestrel). Efficacy of progestin-only pills requires consistent use. So women should take the pill at the same time every day. Mechanism of Action: Progestin-only pills prevent contraception through multiple mechanisms including suppressing ovulation and midcycle gonadotropin peaks and altering the cervical mucus, the endometrium, and fallopian tubes. Candidates: Progestin-only pills are useful for women who want immediately reversible hormonal contraception but for whom estrogen is contraindicated because of breastfeeding, cardiovascular disease, and migraine, for example. Advantages: Progestin-only pills (COCs also are used) can be used to correct dysfunctional uterine bleeding. This bleeding usually results from anovulation and occurs at the extremes of life. Progestin-only pills do not have the estrogen-related side effects that COCs have, such as nausea, headache, and bloating, but they do cause irregular vaginal bleeding. These pills protect against cancer of the uterus and ovaries, benign breast disease, and pelvic inflammatory disease. Contraindication: The only contraindication to taking progestin-only pills is current breast cancer. Disadvantages: Efficacy of progestin-only pills requires consistent use. So women should take the pill at the same time every day. Progestin-only users should be prepared to use a back-up method in case they don’t take the pill as required. The primary side effect is irregular menstrual bleeding, including spotting or breakthrough bleeding, amenorrhea, or shorted cycles. Irregular bleeding decreases in many users by cycle 12. But menstrual side effects are the most frequently cited reasons for discontinuing progestin-only pills. Less common side effects are headache, breast tenderness, and dizziness. Counseling: The pill must be taken at the same time each day. If a pill is more than 3 hours late, a backup method of contraception should be used for at least the next 48 hours. Inform women about emergency contraception. Explain that the range of bleeding disturbances that may occur, including frequent bleeding, prolonged bleeding, irregular bleeding, or, in some cases, amenorrhea. In many women, this irregular bleeding improves within a few months. If bleeding is heavy or particularly bothersome, women should contact their health care provider. |
|
|
Depo-provera:
|
Depot Medroxyprogesterone Acetate (DMPA)
Subcutaneous injection given every 3m (up to 14w) Convenience, high efficacy popular with teens Side effects: Irregular bleeding very common; at least 50% amenorrheic by one year Weight gain Bone mineral density: FDA black box warning. Evidence, however, suggests loss of BMD is small, reversible, not ass’d with osteoporotic fractures Return to fertility prolonged Mechanism of Action: As with other progestins it not only prevents ovulation, it also reduces ovarian production of estradiol. Candidates: DMPA is a good choice for women who want reversible, nondaily contraception DMPA does not require daily use. The convenience and high efficacy rate of DMPA has made this contraceptive method an increasingly popular with teens--the percentage of teens who had used DMPA increased from 10% in 1995 to 21% in 2002. Clinical situations in which estrogen is contraindicated include complicated migraine headaches, diabetes, smokers aged >age 35, and postpartum women. DMPA can be initiated immediately postpartum because it does not contain estrogen--it does not affect breastfeeding. The amenorrhea the majority of DMPA users experience may improve conditions such as menorrhagia, dysmenorrhia, and iron deficiency anemia. At least one-half of users develop amenorrhea within 12 months. Amenorrhea may be a desired lifestyle change. DMPA also can decrease the risk of dysfunctional menstrual bleeding in women who are overweight. But it is only appropriate for women who do not wish to conceive immediately after discontinuing it. The median time to conception for those who do conceive is 10 months following the last injection. Advantages: Reduces the risk of endometrial cancer by up to 80%, with continuing protection after discontinuation. Reduces risk of PID and uterine leiomyomata Can decrease the number and severity of crises in patients with sickle cell anemia. Contraindication: Known or suspected malignancy of the breast (WHO Medical Eligibility Criteria for Contraceptive Use, 3rd edition 2004). Disadvantages: Weight gain: The data suggests that weight gain with DMPA is varies from person to person. Some gain weight while others lose or maintain body weight. Menstrual irregularities: Most women have an altered menstrual cycle with DMPA, including irregular bleeding and spotting, and rarely heavy bleeding, for at least the first 3 months of use. Then, these menstrual changes decrease over time. By one year, up to 70% of women have amenorrhea. Bone mineral density: In 2004, the FDA issued a black box warning that DMPA use may lead to significant BMD loss, increasing the risk of future osteoporotic fractures. Since that time, the best available evidence supports the notion that DMPA use decreases BMD, but that this decrease is small, reversible and has not been associated with osteoporotic fractures. Recent consensus statements do not include recommendations to monitor BMD or to suggest use of calcium or vitamin D supplements based solely on a woman’s use of Depo-Provera Return to fertility: The median time to conception for those who do conceive is 10 months following the last injection. |
|
|
Which 3 birth control methods are considered "moderately effective"?
|
Condoms
Diaphragm Sponge |
|
|
What 3 birth control methods are considered "effective"?
|
Fertility Awareness
Cervical Cap Spermicides |
|
|
Emergency contraception part 1:
|
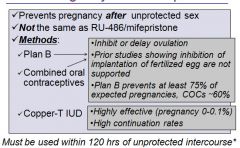
|
|
|
Emergency contraception part 2:
|
Emergency contraception is recommended for all women at risk for unintended pregnancy. It’s used to prevent pregnancy after sex.
There are 3 methods available in the U.S. for EC: Plan B-high-dose progestin-only pills (approved specifically for EC); come as 2-dose regimen (.75 mg levonorgestrel, to be taken 12-24 hours apart) or single dose (1.5 mg levonorgestrel) Certain daily oral contraceptive pills that contain a combination of estrogen and progesterone when prescribed in higher-than-normal doses. Insertion of the copper-T IUD. The progestin-releasing intrauterine system (LNG IUD) is not currently recommended for emergency contraception. Regimen: Plan B: Take 1 tablet (if using single dose regimen) or 2 tablets 12-24 hours apart (for 2-dose regimen) within 120 hours after unprotected sex Oral contraceptives used for EC: Regimen varies by product Copper-T IUD: Insertion within 5 days after unprotected intercourse Contraindications/Indications: There are no medical conditions that preclude the use of emergency contraception pills. The copper IUD is an option for women who want immediate, long-term contraception; are breastfeeding; have a personal history of thromboembolic disease, stroke, or heart attack |
|
|
Medical abortion medication regimens:
|
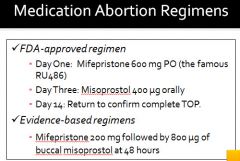
|
|
|
MOA of Mifepristone
|
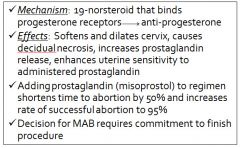
|
|
|
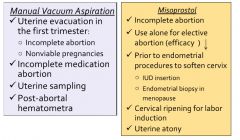
MOA of Misoprostol:
|
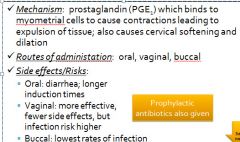
Rates of serious infection dropped significantly after the joint change to buccal misoprostol from vaginal misoprostol and to either testing for STI or routine provision of antibiotics as part of the medical abortion regimen. The rate declined 73% with a change to buccal misoprostol. With addition of routine antibiotics, the rate further declined 93%
|
|
|
Method of manual vacuum aspiration:
|
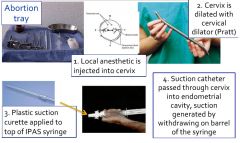
|
|
|
Comparison of medical abortion to MVA:
|
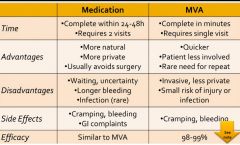
|
|
|
Antibiotic requirement for abortion:
|
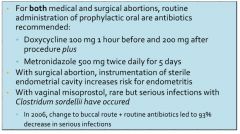
|
|
|
Other clinical indications for abortion:
|
|
|
|
Abortion medication review:
|

|
|
|
Review of the effects of estrogen in the body:
|
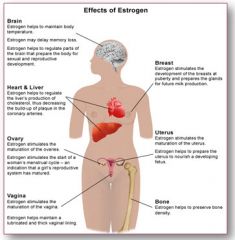
|
|
|
Usage of oral estrogen therapy for menopause:
|
- Conjugated estrogens (also known as CEE)
Orally avail…used alone if hysterectomy Used with medroxyprogesterone (MPA) IF INTACT UTERUS to prevent the effects of unopposed estrogen on the uterus. - 17B-estradiol orally or other routes - Ethinyl estradiol –oral pill Lower dose than used for birth control Used with a progestin |
|
|
Steps in the activation of estrogen receptors ERa and ERb:
|

|
|
|
Alternative methods for administering HRT:
|
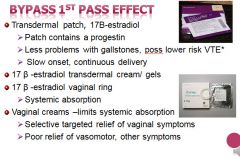
|
|
|
Adverse effects of HRT:
|
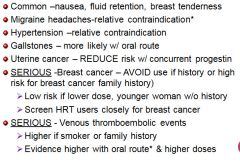
Increase in fluid retention and blood pressure due to estrogen induced increase in renin level.
|
|
|
Adverse effects of the progesterone component of HRT:
|
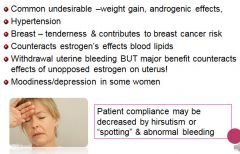
|
|
|
Contraindications for HRT:
|
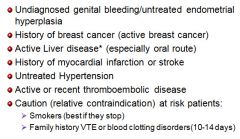
|
|
|
HRT alternatives for hot flash relief:
|
- Progestin-only therapy may relieve vasomotor symptoms in some woman who can’t tolerate estrogen:
Migraine headache suffers Endometrial hyperplasia (common in perimenopausal) - Antidepressant venlafaxine –SNRI (serotonin norepinephrine reuptake inhibitor antidepressant shown good at efficacy at reducing depression & vasomotor hot flashes) Vasomotor symptom relief Improves depression & mood swings - Clonidine – alpha2 adrenergic agonist -symptom relief but side effects may limit use - Gabapentin – GABA analogue anticonvulsant- |
|
|
Androgenic progesterones can have what effect on HDL and LDL levels?
|
They can counteract the positive effect of estrogen; leading to increased LDL and decreased HDL
|
|
|
Clomiphene Citrate (Infertility):
|
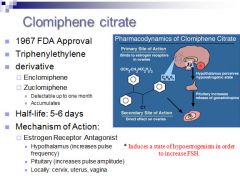
|
|
|
Aromatase Inhibitor (infertility):
|
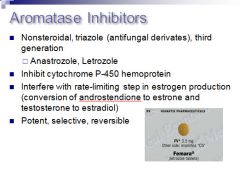
- Has a shorter half life; and less side effects.
- Mechanism of action Centrally: decrease peripheral estrogen production resulting in a decrease in estrogen negative feedback Peripherally: Accumulation of intraovarian androgens and increases follicular sensitivity to FSH - Suppression of peripheral estrogen upregulates estrogen receptors in the endometrium |
|
|
Use of gonadotropins to treat infertility:
|
- Mechanism of Action:
FSH binds granulosa cells CAMP-mediated second messenger system induces aromatase increases granulosa cell number, LH receptors - Contraindications: ovarian failure untreated hyperprlactinemia untreated thyroid, adrenals or pituitary disease lack of appropriate monitoring capability, patient cooperation, or trained personnel ovarian cysts/abnormal vaginal bleeding |
|
|
Method of triggering ovulation:
|
- Usually done with HCG which has a 95% similarity to LH.
- 10,000 IU of urinary HCG or 250 mcg of recombinant HCG - Utilized effectively in those with difficulty accurately predicting an LH surge, luteinized unruptured follicle syndrome |
|
|
At which "cell stage" is embryo transfer most sucessful?
|
Blastocyst stage
|

