![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
What are the hormones of the posterior pituitary?
|
ADH (vasopressin) and oxytocin
|
|
|
Pituitary adenoma:
- Most common cause of hyperpituitarism. - Classified based on the hormones that are produced. - PRL, GH, and ACTH are the most common. - Microadenomas are found in 25% of autopsies. |
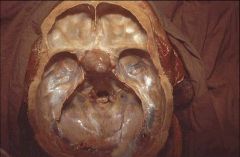
What is this mass?
|
|
|
What are the three most common mutations seen in pituitary adenomas?
|
- G protein mutations: commonly secrete somatostatin and cortisol, but infrequently anything else.
- Mutation on chromesome 11q3 causes multiple endocrine neoplasia (MEN-1), but only causes 3% of adenomas. - RAS and MYC are seen in the most aggressive tumors. |
|
|
Adenomas that are this large infrequently have a hormone secretion.
|
What hormone does this pituitary adenoma secrete?
|
|
|
What are the major clinical characterisitics of a prolactinoma?
|
- 30% of functioning pituitary adenomas (the most common type).
- More common in women. - Presents with a classic triad: amenorrhea, galactorrhea, and infertility. - 25% of women with amenorrhea present with prolactinoma. - Diagnosis: PRL levels of less than 20 ng/Dl will exclude. - Treatment: Bromocriptine a dopamine recetor agonist. |
|
|
What are the major clinical charactersistics of a somatotroph cell adenoma?
|
- Second most common functioning pituitary adenoma.
- Tumors can be basophilic or chromatophobic. - Symptoms: If before full growth, giagantism, if after, acromegaly. - Diagnosis: Elevated GH and IGF-1, GH release not supprsed by the glucose load, and imaging studies. Treatment: Surgery. |
|
|
What are the major clinical characterisitics of a corticotroph cell adenoma?
|
- Tumors are often basophilic, but sometimes chromophobic.
- Exccess ACTH production leads to hypercortisolism (Cushing disease). - Nelson syndrome is a large adenoma that occurs after an adrenalectomy. |
|
|
What are the major clinical characterisitics of a gonadotroph?
|
- Difficult to diagnose because it secretes variably and without clinical effect.
- Middle aged patients may experience headaches and visual disturbances. |
|
|
What is the most rare pituitary adenoma?
|
Thyrotrophs only make up 1% of the pituitary adenomas.
|
|
|
How much of the pituitary must be lost before symptoms emerge?
|
75%
|
|
|
What are the common causes of hypopituitarism?
|
- Mass lesions
- Surgery in the area - Pituitary apoplexy (hemorrhage into an adenoma) - Ischemic necrosis of pituitary - Sheehan syndrome: Post-partum necrosis of the pituitary - Empty sella syndrome - Genetic defects: Rare - Lesions of the hypothalamus |
|
|
What are the subtypes of diabetes insipidus?
|
- Too little ADH is secreted, or the ADH that is secreted is ineffectual.
- Neurogenic: Too little is secreted. - Nephrogenic: The kidney fails to respond. - Primary polydipsia: Abnormal thirst causes too much water intake. - Gestational: Increased metablism of vasopressin causes deficiency. - Symptoms: Polyuria, polydipsia, hypernatrimia, enuresis. |
|
|
What are the causes of diabetes insupidus?
|
Familal mutations, tumors, pituitary surgery.
|
|
|
What are two causes of the syndrome of inappropriate ADH syndrome?
|
- Abnormal regulation of ADH secretion with high levels of ADH.
- Ectopic secretion of ADH by a malignant tumor (small cell carcinoma most commonly). |
|
|
What are the major clinical characteristics of syndrome of inappropriate ADH?
|
- Weakness and general deteriation.
- Confusion and seizures. - Nausea and vomiting. - Hyponatremia is the only abnormal lab value. |
|
|
What are the characterisitics of a carniopharyngioma?
|
- Derived from the remnants of Rathke's pouch.
- Slow growing - Occurs in the hypothalamic region and cause growth defect, visual disturbance, and diabetes insipidus. - Bimodal age distrubance. |
|
|
What is the most common cause of hypopituitarism in children?
|
Craniopharyngoma
|
|
|
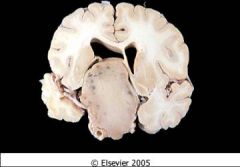
Craniopharyngoma:
- Remanants of Rathke's pouch - Characterisitic cyst formation with epithelial cells present - Difficult to eradicate, but good prognosis. |
What is this pathology?
|
|
|
What locations are common for ectopic thyroid tissue and which area is the most common?
|
Ectopic tissue can be found anywhere along the thyroglossal duct, but is most usually found in the lingual region.
|
|
|
What is the most common congenital throid anomaly?
|
Thyroid cysts:
- Remnant of the thyroglossal duct. - Does not cause any pathology. |
|
|
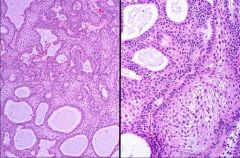
These are thyroid cysts and they are not associated with any pathology.
|

What are the complications from the pathology viewed here?
|
|
|
What is a diffuse (simple/colloid) nontoxic goiter?
|
A form of goiter that involves the entire thyroid gland and cuases it to become non-functional.
|
|
|
What is a multinodular goiter?
|
Recurrent episodes of hyperplasia because of a diffuse goiter results in formation of a multinodular goiter. This is also due to varying sensitivity of the follicular epithelium.
|
|
|
What is a toxic goiter?
|
Describes a goiter that produces thyroid hormone.
|
|
|
What is thyroiditis?
|
Inflammation of the thyroid gland caused by many issues.
|
|
|
This is a nodular goiter:
- Common worldwide because of iodine defciencies in developing nations - Uneven enlargement of the thyroid gland - Possible that nodules are hot |

What is this pathology?
|
|
|
What is thyrotoxicosis?
|
The clinical finding of an increasing metabolic state because of incrasing circulating levels of T3 and T4.
|
|
|
What is hyperthyroidism?
|
Similar to thyrotoxicosis, but causes thyroid dysfunction secondary to a primary thyroid disorder.
|
|
|
What is subclinical hyperthyroidism?
|
Low TSH associated with normal levels of T3 and T4.
|
|
|
What is thyroid ophthalmopathy (exopthalmos)?
|
This is an accumulation of loose connective tissue in the posterior orbit causing the prominent protuberence of the eyes in Grave's disease.
|
|
|
What is a thyroid storm?
|
Abrubt onset of severe thyrotoxicosis.
|
|
|
What are the major clinical characterisitics of thyrotoxicosis?
|
- Increased BMR.
- Cardiac symptoms (tachycardia) - Weight loss - Heat intolerance - Nervousnous - Ten times more common in women. - Goiter more likely in younger patients. |
|
|
What are four basic causes of sustained thyrotoxicosis?
|
- Primary: Overactivity of the thyroid, by far the most common.
- Secondary: Excessive thyroid stimulating hormone. - Tertiary: Caused by hypothalamic disorders. - Exogenous: Caused by taking thyroid hormones. |
|
|
What are the causes of transient thyrotoxicosis?
|
(1.) Subacute granulomatous thyroidosis
(2.) Subacute lymphocytic thyroiditis (3.) Hashimoto thyroiditis |
|
|
What are causes of primary hyperthyroidism?
|
(1.) Graves disease
(2.) Toxic multinodular goiter (3.) Toxic adenoma (4.) Drug-induced goiter (5.) Amiodarone: Antiarrythmic agent that has hyperthyroidism as a side effect. (6.) Iodides: Used in prescription drugs. (7.) Lithium induced hypothyroidism onccurs in depression patients. |
|
|
What are the causes of secondary hyperthyroidism?
|
- Autonomous TSH secerting pituitary hormone.
- Ectopic TSH production is associated with small cell carcinoma. - Agonist effect of HCG, a complication of molar pregnancy. - Mutation of pituitary hormone beta receptor: resistance of thyroid hormone to shut down TSH secretion. |
|
|
What are the causes tertiary hyperthyroidism?
|
- Hypothalamic induced TSH via TRH (rare).
|
|
|
What are two causes of exogenous hyperthyroidism?
|
- Iatrogenic: Excessive administration of thyroxine by physicians.
- Factitious thyrotoxicosis: result of patient self administering excessive doses of thyrotoxicosis. |

