![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
Distinguish between a primary, secondary or tertiary endocrine disorder:
|
A primary disorder affects the target gland itself.
A secondary disorder affects the pituitary gland. A tertiary disorder affects the secretions of the hypothalamus. |
|
|
Which hormone is the only anterior pituitary hormone that is not secreted in response to hypothalamic hormone?
|
Prolactin, is under negative control by the prolactin inhibitory factor (dopamine)
|
|
|
What happens if you cut the infundibulum to all of the hormone secretions?
|
They all lower except Prolactin (since it is under negative control instead of positive control)
|
|
|
What does the anterior pituitary secrete?
What does the posterior pituitary secrete? |
FLAT PEG
ADH (supraoptic nucleus), Oxytocin (para ventricular nucleus) |
|
|
How do catecholamines and thyroid hormones behave?
What are both of these hormone types derived from |
Catecholamines behave like peptide hormones, thyroid hormones behave like steroids.
Tyrosine |
|
|
What enzyme converts testosterone into dihydrotestosterone?
|
5alphareductase
|
|
|
What are the characteristics of testicular feminization?
|
Lack of testosterone receptors means that there is no development of male genitalia.
However, because sertoli cells are still directed to secrete MIS there is also no preferential development of the mullerian duct system (paramesonephric ducts) If however, the patient only has lack of the enzyme 5alphareductase they are slightly more masculine because tesosterone does have a weak effect. |
|
|
How can congential adrenal hyperplasia affect a fetus?
|
Lack of 21 alpha hydroxylase results in excessive production of adrenal hormones and therefore virilization.
|
|
|
What is the first event of true puberty?
|
Increased secretion of FSH and LH during sleep.
|
|
|
Function of the testis:
|
Spermatogenesis
testosterone secretion |
|
|
Function of the Epididymis and vas def
|
Site of sperm maturation
|
|
|
Function of the Seminal vesicle:
|
Supplies bulk of semen volume
Supplies fructose Secrete prostaglandins for sperm motility! Supplies precursors for semen clotting |
|
|
Function of the Bulbourethral glands
|
Secretes mucus for lubrication
|
|
|
Function of the prostate
|
Secretes alkaline fluid
Secretes enzymes that trigger clotting Secretes protease PSA (prostate specific antigen |
|
|
Define infertility:
|
inability to conceive after 12 months of unprotected sexual intercourse
58% related to female factors |
|
|
What makes the Leydig cells secrete testosterone and what does testosterone inhibit?
|
LH = increased secretion of testosterone
testosterone has negative feedback for FSH and LH! |
|
|
What stimulates the Sertoli cells to secrete inhibin and abp?
|
FSH
|
|
|
What secretes inhibin and what is its function?
|
Sertoli cells secrete inhibin and they exert negative feedback on FSH!
|
|
|
Explain how an erection can occur:
|
2 ways either psychogenic or tactile but the concept is the same.
Erotic stimuli increases the parasympathetic tone, causes release of Nitric oxide which vasodilates, the sinusoidal spaces fill with blood with expands the corpora cavernosa compressing venous outflow. Spongiosum does not get hard b/c it has to remain patent for the ejaculate to be released |
|
|
How does slidenafil (viagra) work?
|
It inhibits phosphodiesterase type 5, which would normally break down cGMP (the second messenger of the NO pathway)
|
|
|
What is the purpose of abp?
|
concentrates tesosterone at the site of spermatogenesis
|
|
|
Difference of the negative feedback of Inhibin (spermatogenesis) and tesosterone?
|
Inhibin only inhibits FSH, tesosterone inhibits GnRH from the hypothalamus
|
|
|
What is the purpose of the hormone aromatase?
|
Turns testosterone or androstendione into estradiols
|
|
|
What is mediated by tesosterone versus dihydrotestosterone?
|
Testosterone-mesonephric duct structures (epid, vas, seminal vesicles); spermatogenesis; negative feedback on ant pit; 2 sexual characteristics; end of pubertal growth; libido
DHT: Penis, scrotum, prostate; male pattern hair, and baldness;acne;growht of prostate |
|
|
List 10 functions of estrogen:
|
1: development of 2nd sex chars
2: profli of ovarian /granulosa cells 3: maintainence of tubes 4: regulates tissue responsivness 5: negative feedback effects on FSH and LH 6: maintains pregnancy 7: decreases threshhold for uterine contractions 8: increases prolactin but BLOCKS action at the breast 9: decreases LDL cholesterol 10: maintains bone density |
|
|
List 4 functions for progesterone:
|
1: maintains endometrial secretion in the luteal phase
2: negative feedback control of FSH and LH 3: maintainence of pregnancy 4: increases the threshhold for contractions |
|
|
21 alpha hydroxylase deficiency casues-
|
virilization of the fetus, meaning external masculinization-clitoromegaly etc
|
|
|
Are FSH/LH levels higher or lower post menopause?
|
Higher, b/c there is no negative feedback-particularly on FSH by inhibins which are usually produced by the ovary.
|
|
|
What hormone characterizes the proliferative phase:
|
estrogen
|
|
|
What hormone characterizes the secretory phase?
|
progesterone
|
|
|
What causes menstruation?
|
lack of progesterone
|
|
|
What phase are oocytes arrested in of the cell cycle?
|
meiosis 1
|
|
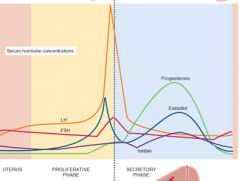
Explain hormone fluctuations during the menstrual cycle:
|
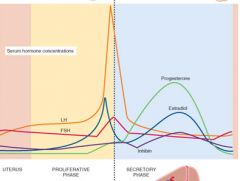
Progesterone-spike after ovulation
LH-speak before ovulation FSH spike at ovulation estrogen-double spike (combo LH and Progesterone) |
|
|
What initiates the follicular phase of the menstrual cycle:
|
Estrogen and FSH bump
|
|
|
What occurs during the follicular phase?
|
Corpus luteum dies= decreased inhibin=increased FSH
Increased FSH causes primary follicles to develop Granulosa cells secrete estrogen and inhibin under the influence of FSH Dominant follicle develops that has a high sensitivity to FSH (inhibin is decreasing the level of FSH) |
|
|
Explain the ovulatory phase of the menstrual cycle?
Hint: Ovulhation |
1: LH surge is caused by the dominant cycle signaling its maturity to the ant pit by increasing estrogen secretion, which exerts positive feedback on the ant pit
2: primary oocyte completes meitoic division to become a secondary oocyte 3: LH, progesterone, and local prostaglandins thin the lining of the ovary so the follicle can pop out |
|
|
Explain the luteal phase of the menstrual cycle?
|
1. the corpus luteum is formed under the influence of LH creating lutein cells
2. cells produce progesterone-prevents another LH surge 3. if pregnancy does not occur the ocrpus luteum degenerates, if implantation does occur the trophoblast cells secrete lh analog HcG which supports the luteum |
|
|
What causes menopause?
|
withdrawal of estrogen because of loss of follicles, FSH and LH surge b/c there is no negative feedback on GnRH
|
|
|
Average age of menopause in the USA?
|
51.5
|
|
|
How do granulosa cells make estrogen?
|
They use aromatase to turn androgens made from theca cells into estrogen.
|
|
|
Why is the first sperm to reach the egg unlikely to fertilize it?
|
The sperm need to undergo capacitation in side the female reproductive track (removes a protein coat)
|
|
|
What type of cervical mucous is best for pregnancy?
|
Stretchy, from estrogen (lets em in)
|
|
|
Explain the 6 stages of implantation:
BAPMCS |
1: BINDING: Sperm binds to the zona pellucida via specific binding proteins
2. Acrosome reaction (Cracrosome) cracks the zona pellucida with enzymes 3.Membrane PENETRATION: sperm penetrates zona pellucida to reach the oocyte membrane 4. FUSION-egg and sperm cell membranes fuse 5. CORTICAL RXN-(courts, keeps the other sperm out)- enzymes are released in the egg via exocytosis that hardens the zona pellucida-prevents polyspermy 6-SYNGAMY-male and female pronuclei fuse, chromosomal sex is determined Birthing Another Person Makes Cervixes Stretch |
|
|
What is capacitation?
|
final maturation event for sperm, occurs in the female reproductive track
|
|
|
Four stages of implantation:
|
1. Cuddle-uterine fluid absorption brings the blastocyst closer to the endometrium-pinopods drink up the fluid
2. Hatching-occurs-breakout from the zona pellucida 3. AAI-apposition, adhesion, invasion 4. Decidual reaction-changes in the endometrium to a thicker lining in concentric waves CHAD was implanted |
|
|
2 functions of the placenta:
|
1. transporting epithelium-nutrient transfer
2. endocrine gland-secretes hormones of pregnancy |
|
|
Why do immuno disorder take a while to be seen in babies?
|
fetal immune system consists of maternal IgG until about 6 months of age.
|
|
|
What is the most important peptide made by the placenta?
|
HCG!!!! rescues the corpus luteum =continued progesterone secretion
after 8-9 weeks the placenta takes over progesterone production |
|
|
What is hCS (hPL)? Human placental lactogen
|
hPL-spares glucose, high during pregnancy, reduces maternal insulin responsiveness!!!!
|
|
|
What substances does the fetal endocrine system need from the maternal system?
|
LDL cholesterol for steroid synthesis
|
|
|
Does the fetus produce progesterone or estrogens?
|
NO! fetus is an androgen sink, it then converts these things to DHEAS to estriol e3 which increases uteroplacental blood flow
|
|
|
How does the fetus create estrogens?
|
It uses DHEA-s to DHEA- 16-OH DHEA from the fetal adrenal gland to make e3!!!-increases blood flow
|
|
|
The non pregnant uterus is what kind of smooth muscle? The pregnant uterus is what kind of smooth muscle?
|
Non pregnant=multiunit smooth muscle
pregnant=single unit smooth muscle |
|
|
Explain the stages of pregnancy:
|

QASI!! quit acting so infantile!
Plase 0-quiesance-uterus is quiet under *progesterone*. Relaxin is secreted by the corpus luteum and maintains the relaxed state. Phase 1-(estrogen!!!s)activation-week before parturition there are low frequency myometrial contractions (braxton hicks), and increased oxytocin and prostaglandin receptors as well as new *gap junctions* to promote unified muscle contraction. Phase 2-stimulation-oxytocin and prostaglandins induce uterine contractions and dilation of the cervix Phase 3- involution-uterus returns to its normal size with the assistance of sustained contraction, assists in blood clotting (oxytocin) |
|
|
What hormones keep the uterus relaxed?
|
progesterone and relaxin (from the corpus luteum)
|
|
|
Timing of labor
|
latent phase-8 hrs
active phase 8-14 hrs slope of cervical dilation happens in this time (to 10 cm) -everything before this is stage 1 Stage 2 delivery occurs from hours 14-16 stage 3 birth until delivery of the placenta |
|
|
What initiates labor?
|
A change in the progesterone/estrogen ratio towards estrogen (decrease in progesterone expression).
Progesterones PGF2alpha causes uterine contraction Oxytocin maintains labor. Prostaglandin release and oxytocin to maintain it (Ferguson reflex) Uterotonin theory (above) means that aspirin can prevent premature labor |
|
|
What are the four shunts of fetal circulation?
|
placenta
ductus venosus foramen ovale ductus arteriorsus |
|
|
What systems are still immature at birth of a fetus?
|
GI system
Erythropoesis immune liver-jaundice is common as hbf is broken down renal system-weight loss |
|
|
What are the roles of oxytocin and prolactin in lactation?
|
prolactin is required for milk production
oxytocin stimulates milk ejection |
|
|
What prevents maternal milk production from occuring before childbirth?
|
high estrogen levels and progesterone
delivery of the placenta reduces these hormone and allows lactation to proceed. |
|
|
What regulates prolactin?
|
lack of negative control by dopamine
|
|
|
What is the most important stimulus for prolactin secretion?
|
the Suckling reflex which inhibits dopamine release, it also stimulates oxytocin release which causes contraction of myoepithelial cells which cause milk ejection.
|
|
|
Why do women not immediately get their period after pregnancy?
|
B/c suckling inhibits the GnRH pulse generator, which supresses FSH and LH
cam result in absence of menses for up to 2 years. |
|
|
Why is it adviseable to breastfeed to prevent vaginal prolapse?
|
Oxytocin release helps stimulate involution so the uterus returns to normal size
|
|
|
What hormone is primarily responsible for the development of the breast?
|
brEstrogen
|
|
|
When does final differentiation of the breast occur?
|
only in preganncy
|
|
|
What is colostrum?
|
Colostrum is secreted initially until milk production gets going, concentrated form of nutrients with a mild laxative effect that helps clear fetal biliruben
|

