![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Hypothalmus Hormones |
corticotropin-releasing hormone(CRH) thyrotropin-releasing hormone(TRH) gonadotropin-releasing hormone(GnRH) growth hormone-releasing hormone(GHRH) growth hormone-inhibiting hormone(somatostatin GHIH) prolactin-inhibiting hormone(PIH) melanocyte-inhibiting hormone(MIH)
GnRH: increases secretion of gonadotropins which are LH and FSH. |
|
|
|
Anterior Pituitary Hormones
|
thyroid-stimulating hormone (TSH) also known as thyrotropin adrenocorticotropic hormone (ACTH, corticotropin) luteinizing hormone (LH), also known as leydig cell-stimulating(LCSH) follicle-stimulating hormone (FSH) prolactin (PRL) growth hormone (GH) melanocyte-stimulating hormone (MSH)
TSH: stimulates synthesis n relase of thyroid hormone works on the thyorid gland. |
|
|
|
Posterior Pituitary Hormones
|
ADH Vassopressin: works on kidneys to promote water reabsorption
Oxytocin: works on uterus and mammary glands to stimulate contractions and ejection of breast milk. |
|
|
|
Thyroid hormones
|
T3 T4 Calcitonin
|
|
|
|
Adrenal Cortex Hormones
|
Glucocorticoids(cortisol): carb/protein/fat metabolism, response to stress, emotional stability, immune function, sleepwake cycle.
Mineralcorticoids(aldosterone): control bodies sodium and potassium content. |
|
|
|
Ovary Hormones
|
Estrogen
Progesterone |
|
|
|
Tested Hormones
|
Testosterone
|
|
|
|
Pancreas Hormones
|
insulin
glucagon somatostatin |
|
|
|
example of a complex control is the interaction of the hypothalamus with the anterior pit and the adrenal cortex
|
low blood levels of cortisol from the adrenal cortex stimulate the secretion of CRH in the hypothalamus n CRH then stimulates the anterior Pituitary to secrete ACTH and ACTH stimulates cortisol relase from adrenal cortex. |
|
|
|
functions of glucocorticoid hormones
|
-prevent hypoglycemia by increasing liver gluconeogenesis and inhibiting peripheral glucose use -maintain excitability and responsiveness of cardiac muscles - increase lipolysis, releasing glycerol and free fatty acids - increase protein catabolism - degrade collagen and connective tissue - increase the number of mature neutrophils released from bone marrow - exert anti-inflammatory effects that decrease the migration of inflammatory cells to sites of injury - maintain behavior and cognitive function |
|
|
|
adrenal medulla hormones
|
catecholamines: epinephrine and norepinephrine travel through blood to target cells in the body.
target cells are usually either alpha adrenergic or beta adrenergic. n NE works mainly with alphas and epi works usually with beta receptors. |
|
|
|
functions of thyorid hormones in adults
|
- control metabolic rate of all cells - promote sufficient pituitary secretion of growth hormone and gonadotropins - regulate protein, carbohydrate, and fat metabolism - exert effects on heart rate and contractility - increase red blood cell production - affect respiratory rate and drive - increase bone formation and decrease bone resorption of calcium - act as insulin antagonists |
|
|
|
PTH
|
regulates calcium and phosphorus by acting on bones kidneys and GI.
It increases bone release or calcium and phosphorus into the extracellular fluid. decreases bone formation and increases bone breakdown In the kidneys: activates vit D which increases absorption of calcium and magnesium and increases excretion of phosphorus and bicarb and sodium. In GI: enhances absorption if calcium and phosphorus from gut through vit D activation. ...all which increase serum calcium when serum levels of calcium are high PTH decreases and increases when serum calcium is low. |
|
|
|
Endocrine changes related to aging
|
<ADH production: urine is dilute...greater risk for dehydration offer fluids every 2 hrs if possible.
<estrogen: bone density loss, skin is thinner drier, vag is drier. do reg exercise, handle pt carefully not pulling or dragging use minimal tape on skin use moisturizer on skin,drink 2L daily urinate after intercourse, vag lubs for comfort. <glucose tolerance: weight gain, elevated Glucose levels. slow wound healing frequent yeast infections polydipsia and polyuria. excerise regularly watch for signs of diabetes. <general metabolism: cold intolerance,decreased appetite and hr and bp. dress warm. |
|
|
|
endocrine testing
|
for blood:
catecholamines must be put on ice and taken to lab immediately if drawing blood from an IV clear line thoroughly. for urine: empty bladder first and then begin collecting. dont save first one. save last one. add preservatives at the beginning of testing not at end. stimulation test: is the gland capable of normal function. suppresion test: can we suppress the elevated hormone level. HbA1c: average blood glucose over 2-3 months. |
|
|
|
Hypopituitarism
|
selective: one hormone of anterior pit.
pan: is all hormones of anterior pit which is rare. resulting in metabolic and sexual dysfunction. <GH: decrease bone density, fractures, muscle strength, n increased cholesterol. <FSH: women: amenorrhea, anovulation low estrogen breast atrophy loss of bone density loss of pubic n axillary hair decreaed libido. men: decreased facial hair ejac volume muscle mass bone density body hair libido impotence. <TSH: weight gain cold intolerance scalp alopecia hirstuism menstrual changes dec libido slow cognition lethargy <ACTH: dec cortisol levels pale malaise lethargy anorexia hypotension headache hypoglycemia hyponatremia dec axillary and pubic hair. <posterior pit hormones: <Vassopressin ADH: Diabetes insipidus interventions: replace deficient hormones, forever. |
|
|
|
hyperpituitarism
|
hyperplasia tissue overgrowth.
causes: most common is pituitary adenoma a benign tumor s/s: visual changes headache ICP all from pressure of tumor pushing on pituitary. >PRL: galactorrhea amenorrhea and infertility >GH: acromegaly: gradual over years irreversible changes in soft tissue of face hands feet and skin skeletal thickness enlargement of organs like liver and heart...bone thinning degeneration of joints hyperglycemia because GH blocks insulin n nerve impairment. treat with octreotide and pegvisomant infections weekly. >ACTH: cushings disease assess: changes in hat glove ring size fatigue or lethargy headaches or vision changes. tests: CT n MRI nonsurgical: Drugs: dopamine agonists like parlodel, dostinex, permax. all inhibit relase od GH n PRL. surgical: hypophysectomy: preop: explain it decreases hormone levels relieves headaches and may reverse secual dysfunction. nasal packing for 2-3 days so breath through mouth and a mustache dressing under nose. DO NOT brush teeth cough sneeze blow nose or bend forward after surgery. postop: monitor neuro response. changes in visual or mental status. decreased strength in extremities. monitor InO for output greater than intake signaling DI. deep breathing, dental floss or mouth rinses, monitor nasal drip for presence of halo signalling csf leak. monitor for increased swallowing which can indicate a CSF leak. |
se of brimocriptine(parlodel) are orthostaic hypotension naseau headaches cramps constipation. tske with meal or snack dont take while pregnant.
|
|
|
anterior Pituitary >PRL
|
hypogonadism
decreased gonadotropin levels galactorrhea incressed body fat increased prolactin levels |
|
|
|
>GH: Acromegaly
|
thickened lips
coarse facial features increased head size protusion of lower jaw deepened voice tufting of fingers enlarged hands ans feet kyphosis and backpain excessive sweating airway narrowing sleep apnea enlarged heart liver and lungs |
|
|
|
>ACTH: Cushings
|
elevated plasma cortisol levels
weight gain truncal obesity moon face muscle waisitng on extremities bone density loss hypertension hyperglycemia purple striae acne thin skin hyperpigmentation |
|
|
|
D.I. <ADH of post pituitary
|
large volumes of dilute urine.
polyuria, dehydration causing increased plasma osmolarity whicu stimulates thirst. signs: hypotension, tachycardia, increased BUN, dilute low specific gravity hypo-osmolor irritable decreased cognition hyperthermia lethargy ataxia treat: Desmopressin: enhances resoprtion of water. dont drink more than 3L a day watch for fluid overload like headache n confusion. Vassopressin: reducing urine output. chlorpromamide: antidiabetic agent watch for sulfa allergy always carry a form of sugar. replace fluids! |
|
|
|
SIADH >ADH
|
hyponatremia, water retention, nausea, vomiting. free water not salt is retained. lethargy headaches hostility disoriention and changes in loc. deceased deep tendon reflexes. urine osmolarity increases, plasma osmo decreases. increased urine concentration.
treat: restrict fluids. dilute feedings with saline and not water. measure InO and weight. rinse mouth but dont swallow. Drugs: Samsca abs Vaprisol they are vasopressin antagonists. samsca is.oral and vaprisol is IV. diuretics only when sodium is near normal and heart faikure is present. provide a safe environment and watch for falls. |
|
|
|
Addisons disease <ACTH and coritsol and aldosterone.
|
decreased gluconeogenesis making glucose from proteins and depleting liver glucogen lesding to hypoglycemia. decreased BUN causing anorexia and weight loss. hyperkalemia leading to acidosis with hyponatremia and hypovolemia. increased pigmentation. salt cravings, vitiligo |
|
|
|
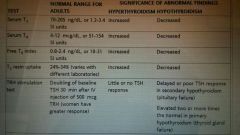
labs for adrenal assessment
|
sodium 136-145 |
|
|
|
Cushings disease >adrenal cortex hypercortisolism
|
buffalo hump. moon face. decreased muscle mass strength thin skin bone density loss. bruising, petechiae, striae, poor wound healing, hypervolemia, and edema hypernatremia. hyperglycemia. crying or lauging a lot. mood swings. shrink spleen and organs. immune response is reduced. usually caused by bilateral adrenal hyperplasia or pituitary adenoma.
test: saliva not spit. Urine test. 24 hour urine specimen seeing increased in BG Na and a decrease un Ca K and lymphs. treat: nonsurgical: patient safety for fluid overload and pulmonary edema leading to skin breakdown use a pressure reducing matress overlay. drug therapy: monutor for weight loss and increased urine output nutrition therapy:restrict fluids and sodium rapid weihht gain is best indicator for fluid overload. and monitoring. radiation therapy. surgical: hypophysectomy or adrenalectomy. preop: electrolyte balance and monitoring. hyperglycemia controlled before surgery. hugh cal hugh protien diet. glucocorticoids before surgery and for life after. postop: after adrenalectomy immediately assess pulse urine hypotension all signs of shock. vitals InO daily weight n lytes. nursinf: use tape sparingly cause fraile blood vessels. osteoporosis until coritsol returns to normal value. high cal diet increasing calcium and D. prevent infection. take meds wirh meals or snacks. increase dose before stressful events. |
|
|
|
hyperaldosteronism >in aldosterone
|
usually by a benign adenoma or high level of angiotensin 2.
hypernatermia hypokalemia metabolic acidosis. nocturia, polydipsia, polyuria, paresthesia. surgery: one or both adrenal glands removed. and spironolactone for potassium support. low sodium diet. long term hormone replacement. |
|
|
|
pheochromocytoma
|
tumor that arises in adrenal medulla. produce stoee and release epinephrine and NE. more in men than women. 40-60.
signs: intermittent episodes of hypertension or attacks ranging from mintues to hours. during this they have headaches palpitations profuse diaphoresis flushing and apprehension. causes that provoke crisis: foods high in tyramine like aged cheese and red wine and drugs like glucagon antidepressants droperidol metoclopramide. tesr: 24h urine. VMA all are elevated. surgery: both are removed and nurse promotes tissue perfusion nutrition and comfort measures. watch for hypertension after surgery. DO NOT PALPATE A PHEYCROMOCYTOMA. |
|
|
|
hyperthyroidism Graves
|
diaphoresis fine soft silky hair smooth warm skin thinning scalp blurred vision eye fatigue increaswd tears photophobia eyelid lag globe lag tremors insomnia heat intolerance fatigue restless emotiinal liability manic widened pulse rste tachycardia increased libido amenorrhea goiter weight loss exopthalmos muscle wasting.
graves is toxic goiter...an autoimmune disorder antibodies attach to TSH receptors and the gland responds by increaskng in size n number of glandular tissue. dry waxy swelling of frontal surfaces. causes: autoimmune DM Vitiligo and RA women 20-40. test: RAI 123 given by mouth and uptake of iodine by thyroid is measured. avoid iodine containing procedures 4weeksb4. n drufs with iodine 1 week b4. nonsurgical: monitor apical pulse bp and temp increase in temo could indicate storm. reduce stimulation. promote comfort by changing damp bed ljnens and ice. drugs: PTU and tapazole orevent iodine binding. but serious liver injury. propranolol for supportive therapy for symptoms of cushings. surgery: total or subtotal thyroidectomy. afger total life long thyroid replacement. suppoet neck and throat when coughing snd deep breathing. use sandbags or pillows for support of head semi fowlers humidifier the air to help resp secretiins. remain alert for damage to PT gland seeing hypocalcemia and tetany. laryngral stridor is heard in acute respiratory obstruction. laryngeal nerve damage is hoarsness and a weak voice. |
goiter clarification: |
|
|
hypothyroidism
|
myxedema edema is mucinous not by water. nonpitting eyes hands feet between shoulder blades thickens larynx and voicr is husky.
hypothyroidism signs: cool pake dry coarse haur poor wound healing depression weight gain anorexia bradycardia enlarged heart hypotension constipation impotence muscle aches and pains cold intolerance hearing loss slow speech edema hoarsness thick tongue anemia causes: little natural iodide surgery iodine def lithium tumors defects in women 30-60 than men. interventions: cardiax and resp priority measure 02 sats and respirations watch for sedating this patient. treat about hormone replacement therapy is for life levothyroxine in low dose and gradually raised take on empty stomach monitor sleep and bowels |
|
|
|
thyroiditis
|
acute: pain neck tenderness malaise fever and dysphagia
subacute: viral infextion fever chikls dysphagia resp infection joint pain. pain that radiares to the jaw. chronic: hashimotos woman more than men. 30-50. autoimmune infection thyroid tissue destruction. dysphagia and painless enlargment. needle biopsy. treat: thyorid hormone and or surgery. |
|
|
|
thyorid cancer
|
papillary younger woman slow growing.
follucular: older patients blood vessels hoarse voice medullary: older than 50 MEN1 type 2 familial. anaplastic: agressive and rapid. do radiation surgery for all others. ablative amount of RAI to destroy tissue if it doesn't work then chemo. |
|
|
|
causes of parathyorid dysfunction
|

|
|
|
|
hyperparathyroidism
|
hypercalcemia
hypophosohatemia decreased bone production and unceasing bone destruction. signs: bone fractures weight loss arthritis renal calculi osteoporosis high Ca leads to nv anorexia epigastic pain constipation and weight loss. test: cAMP n ca phos and pth levels. nonsurg: diuretic and hydration for calcium like lasix. sudden drops of calcium can cause tingling and numbness. prevent injury. handle ot carefully. drugs like oral phosphates only if ca needs to be lowered rapidly. surgery: parathyroidectomy. assess calcium after. |

|
|
|
hypoparathyroidism
|
hypocalcemia hypomagnesemia.
tetany tingling numbness. tesy: calcium phos pth levels and cAMP. nonsurgical: replace vitamins. high calcium low phos foods so avoud milk cheese yogurt. therapy is lifelong. |
|
|
|
calories per stored energy
|
fat has 9 calories of stored energy
protein and carbs have 4. |
|
|
|
FFAs
|
when there is more glucosw in thr liver cells than can be metabolized for energy or stored the insulin from pancreas causws it to be converted into free fatty acids and they are deposited as fat cells.
|
|
|
|
incretin hormones
|
secreted in response to the presence of food in stomach they increase insulin decrease glucagon slow gastric emptying all preventing postpradinal hyperglycemia.
|
|
|
|
absence of insulin
|
hyperglycemia
polyuria polydipsia polyphagia ketone bodies hemoconcentration blood concent hypovlemia decreased blood vol hyperviscosity thick blood hypoxia poor tissue oxygenation kussmaul respirations |
|
|
|
chronic complications of DM macrovascular
|
macrovascular: large blood vessels; coronary artery disease: more in woman than men. albuminuria, cigarette smoking positive family hx. hyperglycemia hypertension and hyperlipidemia...try and maintain bp below 130/80 and LDL below 100. diet changes.
cerevrovascular disease: hypertension hyperlipidemia nephropathy PVD alcohol and tobacco. irreversible brain injury and higher mortality. |
|
|
|
chronic complications of DM microvascular
|
microvascular: small blood vessels tissues and organs:
diabetic retinopathy: after 20yrs of age all pts with T1DM have this. venous bleeding slowly and causes reduced vision to point of blindness. proliferative DR, growth of new blood vessel that is weak leading to hemorrhage and vision loss..vision loss from any form of DR can be central by macular edema causing hard exudates at center of retina main cause of vision loss. hyperglycemia can cause blurred vision and hypo causes double vision neuropathy: loss of nerve function damage to sensory nerve results in pain or loss of sensation, damage to motor nerve results in muscle weakness, sorbitol collects in nerves and impaires nerve conduction. diffuse is slow and affects both sides of body like foot ulcers n deformaties. focal is a singlr nerve can lead to nerve death or ischemia n usually only affext one side of body like carple tunnel syndrome. nephropathy: ESKD 10-15yrs of diabetes. tske ACE inhibitors or ARBS. earliest manifestations is microalbuminuria. |
CAN: leads to orthostaic hypotension and syncope in older adults one of the main reason for falls.
|
|
|
Type 1 DM
|
autoimmune disorder.
|

|
|
|
Type 2 DM
|
combo of insulin resistance and decreased insulin secretion. from obesity and physical inactivity.
|
|
|
|
prediabetes
|
impaired fasting glucose of 100 to 125
or imparied glucose intolerance of 140 to 199. |
|
|
|
indications for testing individuals for type 2 diabetes
|

|
|
|
|
normal ranges for glucose testing
|

|
|
|
|
blood glucose testing prep
|
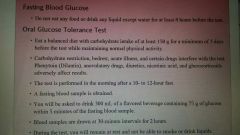
|
|
|
|
urine test of ketone bodies
|
the presence of mod to high ketones indicates a severe lack of insulin. treat with insulin.
|
|
|
|
nonsurgical mgmt of DM
|
nutrional interventions
blood glucose monitoring planned excersice program drugs to lower blood glucose: started at lowest dose and raiswd every 2weeks. drug is based on cost. Insulin secretagogues for those still able to produce insulin. sulfonylureas. meglitinide analogs designed for meal related release. |
|
|
|
secretagogues
|
glucotrol: 30min before meal.
Amaryl: single daily dose with first meal of day |
|
|
|
Meglitinide Analogs
|
Prandin: short acting used to orevent postmeal hyperglycemia take 1-30min before meal.
|
|
|
|
Biguanides
|
metformin: lowers basal and postmeal glucose. take with food. side effects are nv flatus diarrhea indigestion. dont use if have CHF which will increase risk for lactic acidosis which presents as malaise unusal muscle pain resp distress somnolence abdominal distress. swallow whole never crush.
withhold 48hrs before an iodine contrast. |
|
|
|
alpha glucosidase inhibitors
|
precose: prevent post meal hyperglycemia. tske with first bite of each meal. take missed dose at next meal but dont double. se are diarrhea and flatus.
|
|
|
|
thiazolidinediones
|
actos: improves sensitivity to insulin. watch liver. dont take while prego and monitor for fluid retentuon.
|
|
|
|
Amylin analog
|
Symlin: tyoe 1 and 2. syringe. eat or drink carbs after taking. do not mix inuslin with others.
|
|
|
|
incretin mimetics
|
Byetta: subq within 60min before morning or evening meals. watch for hypersensitivity reactio s like itching.
|
|
|
|
insulin sensitizers
|
biguanides like metformin and thiazolidinediones. they dont increase insulin production they decrease liver glucose production helping the insulin work better.
|
|
|
|
Time and activity of Insulin
|
Rapid acting: onset 30 min peak 1-3h duration 3-5.
short acting: Humulin R: onset 50min peak 2-4 duration 5-7 intermediate acting: Humulin N or NPH: onset 1h30min peak 4-12 duration 16-24 long acting: onset 2-4 no peak duration 24hrs. |
|
|
|
factors influencing insulin absorption
|
injection site: fastest in abdomen. rotating sites prevents lipohypertrophy. rotation within onr anatomic site us preferred to rotation from one area to another.
absorption rate: heat massage and excersice of inejcted area increase absorption. scarred areas feel less pain but slow absorption. injection depth: thin give at 45 degree angle to avoid IM injecting. timing: rapid insulin needs to be given 10min before meals. lag time is thr time between eating and ur premeal injection. when blood glucose is higher than normal increase lag time to give insulin timr to affext sooner before eating. if bg is low rapid should be delayed until after eatinf and regular until immediately bdfore eating. mixing: always draw up shorter acting insulin first. dont mix glargine with any other. |
|
|
|
complications of insulin therapy
|
dawn phenomenon: nighttime release of GH that causes BG elevations at about 5-6am...mgmt by providing more insulin for the overnight period like giving intermediate acting at 10pm.
somogyi phenomenon: morning hyperglycemia from nighttime hypoglycemia ensuring adequate dietary intake at bedtime. both problems are diagnosed by blood glucose monitoring during the night. |
|
|
|
alternative methods of insulin administration
|
continuous subcutaneous infusion CSII increases insulin st mealtimes with flexibility in meal timing given by an externally worn pump with a syringe snd reservior holding rapid acting insulin and connectef to patient by infusion set. problems are skin infections, stopping infusion to fast, ketoacidosis, pump problems, obstruction
insulin given by jet injection is absorbed faster and has a shorter duration but costs alot. |
|
|
|
insulin storage
|
refrigerate insulin not in use to prevent exposure to sun and inhibits bacteria.
insulin in use can be kept at room temp for up to 28days to reduce cold injections. dont shake. dont freeze. glargine should be stored in fridge even when in use and discard after 28 days. prefilled syringes are stable up to 30days when in fridge. keeo in upright position. roll prefilled syringed between hands before using. rapid short and glargine should be clear others should be cloudy |
|
|
|
pen type injectors
|
not designed for independent use by visually impaired or those with cognitive impairment.
|
|
|
|
SMBG
|
evaluate response to therapy and assess whether glycemic targets are being reached.
finger prick. even have talking meters for those visually impaired. home tests measure whole blood and labs measure plasma glucose which is 10-15% higher. common errors: failure to obtain sufficient blood drop. poor strip storage. using expired strips. not changing code number to match strip bottle. do not share monitoring equipment. presence of maltose from dialysis can cause elevated false bg levels. alternate testing sites are not always the same as the finger. CGM: monitors glucose in interstitial fluid. transmitter attached to a sensor using radiofrequency every 1-5min. high cost. meant to supplement not replace finger sticking tests and give insulin only after confirming with finger stick. |
|
|
|
diet
|
carbs: 45-65%. with a minimum of 130g a day. carbs from fruit low fat milk whole grains.
limit sat fat to less than 7%. minimizing trans fats limiting dietary cholesterol to less than 200mg day having 2 or more servings of fish a week. protein: intake of 15-20% with normal kidney function. with crappy kidneys protein less than 10% or less. fiber: 25g a day. fruits veggies fiber rich cereals. alcohol with meals or shortly after NEVER before. 2 foe men one for women. |
|
|
|
blood glucose monitoring
|
before and 2hrs after meals determinrs weather insulin to carb ratio is correct.
|
|
|
|
exercise therapy
|
glucose stays balanced in non diabetic people working out.
type 1DM cannot make thr changes needed to maintain stable blood glucose levels during exercise. so without adequate insulin cells cannot use glucose. and in absense of insulin free fatry acids become the source of energy. so if they exercise they become more hyperglycemic and form ketone bodies. exercise can also cause hypoglycemia up to 24hrs after. start with low and work up to vigourous. warm up 5-10min before and cool down for 5-10min after. test blood glucose before exercise and after. the absence of ketones means insulin regimen is efficient. when ketones are present the patient SHOULD NOT EXERCISE. dont exercise within 1hour of insulin injection or at peak time. and unless blood glucose id at least 80 and less than 250. eat a carb beforehand. carry a simple sugar. |
screen when any of these are present:
Teach pt about the relationship between regularly scheduled exercise and blood glucose levels, blood lipid levels, and complications of diabetes Reinforce the level of exercise recommended for the patient based on his or her physical health Instruct pt to wear appropriate footwear designed for exercise Remind them to examine their feet afterward Warn the pt not to exercise within 1 hour of insulin injection or near the peak time of insulin action Teach pt how to prevent hypoglycemia during : Do not exercise unless bg is at least 80 and no greater than 250 Have a carb snack before if 1 hour has passed since last meal or if planned exercise is high intensity Carry a simple sugar to eat during exercise if symptoms of hypoglycemia occur Ensure that identification information is carried during exercises Remind pt to check blood glucose levels more frequently on days in which exercise is performed and that extra carb and less insulin may be needed during 24 hour period after extensive exercise |
|
|
blood glucose in hospital patients.
|
stress hyperglycemia. resukt from decline in basic level of glucose cause by illness.
complications: higher infectio rates longer hospital stays increased nerds for intensive care. greater mortality. dont give insulin to and NPO patient. |
|
|
|
patients with autonomic neuropathy or vascular disease need close monitoring to avoid hypotension or resp distress
|
those who take beta blockers for hypertension need close monitoring foe hypoglycemia because these drugs mask hypoglycemia.
patients with azotemia(increased protein or nitrogen waste products in thr blood) may have problems with fluid mgmt. hyperglycemia usually happens before fever so watch for a normal patient suddenly developing hyperglycemia and check for infection. |
|
|
|
preventing injury from peripheral neuropathy
|
follow preventive foot practices
cleanse and inspects feet daily wears properly fitting shoes avoids walking barefoot trims toenails properly reports nonhealing breaks on feet to HCP foot injury is thr most common complication of diabetes leading to hospitalization. diabetic foot ulcers: caused by peripheral neuropathy and ischemia from peripheral vascular disease. motor neuropathy: results in damage to the nerves of the intrinsic foot muscle that lesd to imbalance between flexion and extension of foot whicu leads to deformities. claw toe deformity where toes are hyperflexed and has increased pressure on ball of foot. the charcot foot is a diabetic foot including a hallux valgus a turning inward of the great toe and the foot is warm swollen and painful. and walking gives the foot a rocker bottom shape. autonomic neuropathy: dry thinning skin skin cracks and fissures increasing risk for infections. sensory: tingling and or burning and numbness and reduced sensations. ulcers on sole or ball are from standing or walking and those on thr sides and top are from shoes. test: do the 10g monofilament test and if a person cant feel the filament at any pojnt they are at rjsk. |

|
|
|
foot risk categories
|
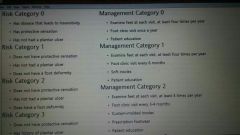
|
|
|
|
wound care for foot ulcers
|
moist environment: influenced by the dressing which reduce or prevent friction allow debridment reduce wound pain and stimulate granulation tissue keep wound moist is essential. things like iodine hydrogen peroxide and chlorhexidine all interfere with wound healing.
debridment if necrotic tissue: removes dead tissue that support bacterial growth proper debridment to reduce risk of infection and pressure. dont use mechanical debridment though. elimination of pressure(offloading): dont wear shies on affected foot while ulcer is healing. the purpose of offloading is to redistribute force awsy from ulcer site. use total contact casting half shoes removable cast walkers wheelchairs crutches. ulcer will reoccur unless redistribution of weight is life long. |
foot care instructions
|
|
|
foot care instructions
|
inspect your feet daily especially between the toes wash feet daily with luke warm water and dry thoroughly apply moisturizing cream after bathing. do NOT apply between the toes change into clean cotton socks everyday do not wear the same pari of shoes two days in a row and wear only breathable shoes check for foreign objects in shoes before putting them on. check the inside lining for cracks or tears buy shoes that have plenty of room for your toes. buy them later in the day when feet are normally larger break them in gradually wear socks to keep feet warm trim nails straight across and then smooth with an emery board see hcp for blisters, sores or infection. protect area with dry sterile dressing do not treat with home remedies do not use adhesive tape on foot do not smoke check the water of the bathtub before entering do not use extreme temperatures in water do not heat feet with water bottles, heating pads, or portable heaters do not treat ingrown toenails, bunions, blisters, calluses, or corns yourself no not go barefoot do not wear flip flops do not cross legs, or wear garters or stockings that constrict blood flow do not soak your feet
|
|
|
|
mgmt of neuropathic pain
|
gabapentin (neurotin)
pregabalin (lyrica) SNRI (cymbalta) the burning may be treated wjth capsaicin cream. |
all pts with neuropathy are risks for foot ulcers and require frequent assessment and education in foot mgmt.
|
|
|
preventing injury from reduced vision
|
blood glucose control
surgical intervention for retinal hemorrhage or new retinal blood vessel growth csn reduce vision loss. besides regular eye exams have pt with impaired vision to have an optometrist assess remaining vision and give appropriate eyewear. supplement fluoresent lighting with incandescent lighting. place dark equipment against light background snd vice versa. coding insulin with bright colors or felt tipped markers. DO NOT GIVE PREFILLED SYRINGES TO VISUALLY IMPAIRED. instead use count a dose whicj clicks for each turn. wrapping rubber band around fast acting. |
|
|
|
reducing risk for kidney disease
|
control of hypertension.
test GFR and serum creatinine annually. annual test for microalbuminuria for type 1 who have had it more than 5yrs=30-299perday. when albumin rises over 300 its termed albuminuria. once it develops we focus on controlling bp and blood glucose restricting dietary protien avoiding nephrotoxic agents promtly treating UTIs and preventing dehydration. smoking cessation. drugs: ACE and ARBS. monitor for hyperkalemia. restrict dietary protein. avoid dehydration and if all else fails do dialysis. |
|
|
|
preventing hypoglycemia
|
Whipples triad: manifestations consisten with low blood glucose a low plasma concentration and reslotuion of symptoms after plasma glucose concentration is raised.
once glucose falls below 70 signs are irritability tremulousness sweating anxiety tachycardia hunger all serve as a warning before central neuro symptoms occur which is paralysis seizure and coma. the brain cannot make glucose and storws onky a few minute supply and the supply isnt maintained when blood glucose falls. the first defense for a non diabetic is decreased insulin secretion and decreased glucose use and increased glucose production. glucagon and epinephrine are counterregulatory hormones. they both raise bloog glucose levels. in type 1 they dont know their glucose is dropping because they have lost that effext since their insulin comes from a shot and not their body so they dont have that feedback. treat: glucagon subq or IM and D5W. thn give a smaller sugsr and snack or meal. for mild: glucose tablets, half cup fruit juice or nondiet sofa, cup skim milk, 6 hsrd candies, 4 sugar cubes, 4tbs sugar, 6 saltines, 3 graham crackers, 1tbs honey or syrup. then retest blood in 15min. and repeat if not resolved then est a small snack or carb and protein if not a next meal. for moderate: 15-30g of rapidly absorbed carb. and take additional food like low fat milk or cheese after 10min for severe: administer 1mg of glucagon n second dose in another 10 minutes. notify HCP. If still unconscious transport to ED. give small meal when awakens. |
|
|
|
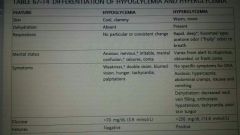
differences in hyper and hypoglycemia
|
|
|
|
|
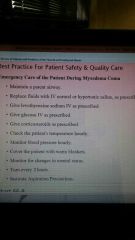
preventing DKA
|
in type 1DM
most common is infection. polyuria polydipsia wt loss vomiting abdominal pain dehydration altered mental status. kussmaul respirations very deep and rapid csuse resp alkalosis in an attempt to correct metabolic acidosis. after treatment starts potassium levels drop quickly. treat: assess airway thrn level of consciousness hydration status electrolytes and blood glucose level n vitals every 15min. assess for jugular vein pressure. hypotonic fluids NS at 4-14mL/kg/hr. after initial fluid bolus. when blood glucose reaches 250 give D5W in .45%NS. this solution prevents hypoglycemia needs fluids to replace those lost which is up to 6-10L. n give insulin through IV. do bolus and then infusr of 0.1unit/hr. potassium replacement. before giving IV potassium pt must be outputting at least 30mL/hr. |
signs of hypokalemia are fatigue malaise confusion muscle weakness shallow respirations abdominal distention paralytic ileus hypotension n weak pulse.
|
|
|
differences in DKA n HHNS
|

|
|
|
|
preventing HHNS
|
no ketones snd blood glucose is much higher from kidney impairment. usually in older adults with type 2. seizures jerking reversible paralysis and neuro impairment. cant drink enough water...extreme diuresis.
treat: replace fluids. in shock give NS otherwise usually give half normal saline. infuse at 1L/hr. then reduce to 100-200mL hr. replace half the water deficite in first 24hrs. assess hourly for signs of cerebral edema like abrupt mental changes abnormal neuro signs and coma. n administer IV insulin after fluid is replaced. monitor closely thrn for hypokalemia. |
|
|
|
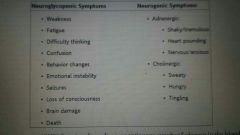
symptoms of hypoglycemia |
neuroglycopenic symptoms: weakness, fatigue, difficulty thinking, confusion, behavior changes, emotional instability, seizures, loss of consciousness, brain damage, death,
neurogenic symptoms: adrenergic: shakey/tremulous, heart pounding, nervous/anxious cholinergic: sweaty, hungry, tingling |
|

