![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
98 Cards in this Set
- Front
- Back
|
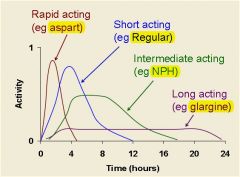
Name the rapid acting insulin preparation
|
Insulin lispro
|
|
|
Name the short acting insulin preparation
|
Regular Humulin R
|
|
|
Name the intermediate acting insulin preparations (2)
|
NPH Humulin N
NPH Novolin N |
|
|
Name the long acting insulin preparation
|
Insulin glargine
|
|
|
Name the Insulin Preparation:
Onset of action: 15 min Peak effect: 0.6-0.8hr Duration of action: 3-5 hr |
Insulin Lispro
**Given IV for Emergencies** |
|
|
Name the Insulin Preparation
Onset of action: 1.1 hr Peak effect: 5-24 hr Duration of action: 24 hr |
Insulin Glargine
**Basal level throughout the day** |
|
|
Name the Insulin Preparation:
Onset of action: 30-60 min Peak effect: 1.5-4hr Duration of action: 5-8hr |
Regular Insulin
**Covers you before meals** |
|
|
Name the Insulin Preparation:
Onset of action: 1-1.5 hr Peak effect: 6-12 hr Duration of action: 18-24 hr |
NPH Insulin
**sets a basal level** |
|
|
|
|
|
A typical type I diabetic's regimen is? (2)
|
- Take a long acting insulin (eg glargine) to cover your basal rate
- Take rapid acting insulin (eg aspart) before meals to cover the carbohydrates (aka glucose) in the meal |
|
|
What types of insulin preparations would you use for basal insulin levels?
|
Insulin NPH
Insulin Glargine |
|
|
How does Hypoglycemia cause the following effects:
-Sweating -Hunger -Paresthesias -Palpitations -Tremor -Anxiety |
Activates the SNS
|
|
|
How does Hypoglycemia cause the following effects:
-Difficulty concentrating -Confusion -Weakness -Drowsiness -Blurred vision -Loss of consciousness |
Insufficient Glucose for Brain
|
|
|
_____ is the only resource of energy for the Brain...
|
Glucose
|
|
|
How do you treat hypoglycemia from an insulin overdose?
|
Sugar --> cookies, candy, OJ
Administer Glucose Administer Glucagon |
|
|
What hormone increases gluconeogenesis and glycololysis in the liver --> raises blood glucose ?
|
Glucagon
|
|
|
____ cells release glucagon
|
alpha cells
|
|
|
What is the clinical use for glucagon?
***** |
Hypoglycemia
(SubQ injection) |
|
|
Do the following drugs treat type I or type II diabetes?
-Biguanides (Metformin) -Meglitinides -Sulfonylureas -Thiazolidinediones -Incretin mimetics -Amylin analog - a-glucosidase inhibitors |
Type II Diabetes
|
|
|
A 52-year-old male is newly diagnosed with type 2 diabetes mellitus. He begins lifestyle modifications. What will be the initial drug therapy for this patient?
|
Metformin
**1st line drug for type II DM** |
|
|
What is the 1st line drug for type II diabetes?
|
Metformin
It combats insulin resistance!! |
|
|
T/F:
Metformin is ineffective in the absence of insulin |
True
|
|
|
MOA:
**Liver** -Decrease hepatic glucose output -Probably reduces gluconeogenesis **Skeletal muscle and adipose tissue** -Enhances insulin stimulated glucose uptake -Enhances utilization of glucose -Decreases insulin resistance |
Metformin
|
|
|
What will happen to serum insulin concentrations with metformin?
|
Serum insulin will decrease since metformin works on peripheral tissues
|
|
|
What will happen to post-prandial glucose concentrations with metformin?
|
After eating, metformin decreases glucose concentration
|
|
|
What will happen to fasting blood glucose (FBG) levels with metformin?
|
FBG levels decrease when taking metformin
Metformin decreases insulin release while fasting, this decreases glucose released from the liver --> ↓FBG levels |
|
|
With type II diabetes there is an increase/decrease in both postprandial and glucagon levels
|
INCREASE
|
|
|
What is the biggest side effect we worry about with Metformin use?
|
Lactic Acidosis
|
|
|
How does Metformin result in Lactic Acidosis?
|
Metformin increases lactate production caused by tissue hypoxia
(favors ANAEROBIC metabolism) |
|
|
***Contraindications***
- Renal disease - Hepatic disease or alcohol abuse - History of lactic acidosis - Decreased tissue perfusion or hemodynamic instability: -Acute MI- -Acute left ventricular failure- -Chronic hypoxic lung disease- -Septicemia- |
METFORMIN
**Increased risk of lactic acidosis** |
|
|
Why is metformin therapy halted prior to:
-Administration of IV contrast media -Surgery |
IV contrast media → acute renal failure
Surgery → compromised circulation **These procedures predispose to lactic acidosis** |
|
|
While lactic acidosis is very rare or essentially zero without a predisposing condition, why is this such a big deal?
|
**Potentially Fatal**
Lots of people with type II diabetes have contraindications for metformin use |
|
|
Two of the biggest concerns in treating type 2 diabetes mellitus is whether or not the drug causes hypoglycemia or weight gain. What effect will metformin most likely have on these parameters?
|
**Hypoglycemia**
NO.. metformin doesn't increase insulin levels **Weight Gain** NO.. Nausea causes you to eat less.. Decreased insulin activity will actually promote weight loss |
|
|
Will metformin cause weight gain or hypoglycemia?
|
Nope
|
|
|
How does metformin protect a type II diabetes patient from Coronary artery disease and Peripheral Vascular Disease?
|
**Decrease TG, total and LDL-C**
- Decrease VLDL synthesis |
|
|
If your patient developed significant renal impairment should you continue metformin use?
|
NO...
metformin is contraindicated in patients with renal failure → LACTIC ACIDOSIS |
|
|
MOA:
Stimulate peroxisome proliferator-activated receptor-γ (PPAR-γ) |
Pioglitazone
Rosiglitazone --> never used **Thiazolidinediones** |
|
|
Name the Thiazolidinedione used for the treatment of type II diabetes to decrease insulin resistance
|
Pioglitazone
|
|
|
What 2 drugs decrease insulin resistance in type II diabetics?
|
Metformin
Pioglitazone |
|
|
What is PPAR-γ?
A.G protein-coupled plasma membrane receptor B.Tyrosine kinase plasma membrane receptor C.Intracellular receptor that increases transcription |
C.Intracellular receptor that increases transcription
|
|
|
Where is PPAR-γ located?
A.Lots in adipose tissue and some in skeletal muscle and liver B.Only in pancreatic beta cells |
A.Lots in adipose tissue and some in skeletal muscle and liver
|
|
|
PPAR-γ activation ____ GLUT 4 expression allowing you to get more glucose into the cell
|
increases
|
|
|
MOA:
- Activates the nuclear peroxisome proliferator-activated receptor-γ (PPAR-γ) - This increases transcription of genes such as the glucose transporter, GLUT4. - In adipose tissue and skeletal muscle, it increases uptake and utilization of glucose. - In liver, it inhibits gluconeogenesis. |
Pioglitazone
|
|
|
Is insulin required for the glucose lowering effect of pioglitazone?
|
YES
Insulin stimulates glucose uptake! |
|
|
Will pioglitazone tend to cause hypoglycemia?
|
No...
Insulin activity of the pancreas is not effected so you will not get hypoglycemia (i.e. insulin activity is normal) |
|
|
Does Pioglitazone cause weight gain? If so, how?
|
Pioglitazone causes weight gain
**Kidneys** ↑ Na+ reabsorption→EDEMA **PPAR-γ activation** ↓ differentiation of pre-adipocytes to mature fat cells ↓ Weight Gain |
|
|
Would you use pioglitazone in a patient with bad heart failure?
|
You would AVOID using a glitazone becuase they cause EDEMA which would make CHF worse...
Use Metformin instead = no weight gain/edema |
|
|
How could pioglitazone cause decreased bone density and increased fracture risk?
*** |
PPAR-γ activation
↓ Bone marrow stromal cells diverted to form adipocytes ↓ Decrease bone density Increase fracture risk |
|
|
Adverse Effects:
-Fluid retention Contraindicated in NYHA Class III and IV heart failure -Weight gain -Increased risk fracture Women only |
pioglitazone
|
|
|
Why is Rosiglitazone almost never used?
|
Data suggesting increased risk of carddiovascular events --> MI, stroke
|
|
|
Name the class of drugs:
-Glimepiride -Glipizide -Glyburide |
Sulfonylurea Drugs
|
|
|
Name the sulfonylurea drugs
|
-Glimepiride
-Glipizide -Glyburide ** "GL-" ** |
|
|
MOA:
- Binding of a ___ causes the K channel to close, thereby preventing K efflux. - This depolarizes the cell, opening a voltage gated Ca channel. - This increases the pulsatile secretion of insulin |
**Sulfonylurea Drugs**
-Glimepiride -Glipizide -Glyburide |
|
|
A person with type 2 diabetes took glipizide which increased insulin release from pancreatic b cells. What effect will that have on glucagon secretion from pancreatic a cells?
|
Insulin inhibits glucagon release
(Decreased glucagon) |
|
|
Why may sulfonylurea drugs fail?
|
They may cause permanent membrane depolarization!!
|
|
|
Will a sulfonylurea cause hypoglycemia and weight gain?
*** |
Yes
You are increasing insulin secretion which promtote hypoglycemia and weight gain |
|
|
Adverse Effects:
-Allergic Skin Reactions -Hyponatremia and SIADH |
Sulfonylureas
|
|
|
Name the Meglitinide Drugs
|
Repaglinide
Nateglinide |
|
|
Repaglinide
Nateglinide |
Meglitinide Drugs
|
|
|
Which 2 drug classes treat reduced insulin secretion caused by type II diabetes?
|
Sulfonylureas
Meglitinides |
|
|
These drugs:
Have a similar MOA to Sulfonylureas ↓ Inhibit the ATP-sensitive K channels |
Meglitinides
|
|
|
Clinical use of Meglitinides?
|
-Type 2 diabetes
-Take before meals to control post preandial glycemia |
|
|
What class of drugs treat reduced GLP-1 secretion in tpye 2 diabetics?
|
Incretins
|
|
|
Name the actions of GLP-1 on:
-The stomach -The brain -The pancreas |
**Stomach**
Slows Gastric Emptying **Brain** Promote a sense of satiety **Pancreas** -↑ glucose-dependent Insulin secretion -↓ Glucagon secretion |
|
|
What enzyme metabolizes GLP-1?
|
DDP-IV
|
|
|
How can you increase GLP-1 effects in the body?
|
Give GLP-1 analog
Block DPP-IV activity |
|
|
Will meglitinides cause allergic reactions, cholestatic jaundice and SIADH like sulfonylureas?
|
No..
Sulonylureas will cause these adverse effects |
|
|
name the GLP-1 agonists
|
Exenatide ***
Liraglutide ** "-tide" ** |
|
|
name the DPP-IV inhibitors
|
Sitagliptin
Saxagliptin ** "-gliptin" ** |
|
|
Which can cause a higher concentration of ‘GLP-1’ (greater GLP-1 effect)?
A. Exenatide B. Sitagliptin |
Exenatide!!
You can give the patient as much exenatide (exogenous GLP-1 promoter) as you want for a larger effect. Sitagliptin will only give you as much GLP-1 as your body can produce |
|
|
Which agent will most likely reduce appetite and food intake?
A. Exenatide B. Sitagliptin |
Exenatide!
Exenatide will give you higher concentration of GLP-1 which will affect the brain! |
|
|
Sitagliptin vs. Exenatide:
-Increases glucose stimulated β-cell secretory activity - Reduces α-cell secretory activity |
Both Exenatide and Sitagliptin will produce these low concentration GLP-1 effects on the pancreas
|
|
|
Sitagliptin vs. Exenatide:
- Delays gastric emptying - Increases satiety |
Exenatide
Will produce a high concentration of GLP-1 which will affect the brain |
|
|
What is the advantage of increasing glucose stimulated insulin release?
|
Hypoglycemia WILL NOT be an issue..
The body won't secrete enough insulin to cause hypoglycemia if FBG levels are normal/low |
|
|
What is the advantage of decreasing glucagon release?
|
You help normalize high glucagon levels which would (normally) increase hepatic glucose production
|
|
|
Which incretin drug delays gastric emptying?
|
Exenatide
|
|
|
What is the advantage of delayed gastric emptying?
|
Decrease the rate that carbs or absorbed and eliminate post prandial glucose spike
This allows the pancreas to "catch-up" and gain control of blood glucose levels after eating |
|
|
Why do the GLP-1 agonists cause nausea and vomiting?
|
Delayed Gastric Emptying
|
|
|
Adverse Effects:
Hypoglycemia – low risk **Allergic reactions** - Rash, hives, angioedema, anaphylaxis, Stevens Johnson syndrome |
DPP-IV inhibitors
|
|
|
Adverse Effects:
Nausea, vomiting Hypoglycemia – low risk Pruritus, urticaria, rash Acute pancreatitis |
Exenatide
Liraglutide (GLP-1 Agonists) |
|
|
What effect will exenatide have on body weight?
|
Delayed gastric emptying/nausea--> weight loss
Satiety factor = weightloss (GLP-1 effects on brain) |
|
|
What effect will sitagliptin have on body weight?
|
NO EFFECT
GLP-1 levels won't be high enough to affect the brain |
|
|
What drug will treat reduced amylin secretion caused by type 2 diabetes?
|
Pramlintide
|
|
|
This hormone is secreted and works with insulin to control glucose levels
|
Amylin
|
|
|
Name the amylin mimetic drug
|
Pramlintide
|
|
|
Clinical Use:
-Type 1 and Type 2 diabetics who inject insulin at meal times -SubQ injection |
Pramlintide
(Amylin mimetic) |
|
|
MOA:
____ is co-secreted with insulin from pancreatic beta cells. **Inhibit glucagon secretion **Delay gastric emptying **Increase satiety - These actions slow and reduce the entry of glucose into circulation – works with insulin to regulate glucose levels. |
Pramlintide
(Amylin mimetic) |
|
|
Adverse effects:
Nausea, vomiting, anorexia Headache Hypoglycemia when combined with insulin |
Pramlintide
(Amylin mimetic) |
|
|
Why does pramlintide cause hypoglycemia when combined with insulin?
|
You take pramlitide and insulin before eating...
The satiety caused by pramlintide (amylin) causes you to eat less so you overshoot the amount of insulin you needed for that particular meal The excess insulin causes hypoglycemia |
|
|
What type 2 diabetes drugs reduce gastric emptying and reduce post-prandial spike in blood glucose levels? (3)
**** |
Exenatide
Pramlitide (amylin) Acarbose |
|
|
Name the α-glucosidase inhibitor
|
Acarbose
|
|
|
Acarbose is a ______ inhibitor
|
α-glucosidase inhibitor
|
|
|
MOA:
-Inhibits α-glucosidase metabolism of disaccharides to glucose ↓ -Slower absorption of glucose ↓ -Reduced post-prandial peak in blood glucose |
Acarbose
|
|
|
Will acarbose reduce fasting blood glucose levels ?
|
No...
It acts in the small intestine to reduce post-prandial glucose spikes |
|
|
Adverse Effects:
Flatulence Bloating Abdominal discomfort Diarrhea Elevation of liver enzymes |
Acarbose
(α-glucosidase inhibitor) |
|
|
Explain these adverse effects with acarbose:
Flatulence Bloating Abdominal discomfort |
Decreased breakdown of carbs in the small intestine causes colonic bacteria to breakdown the carbs and produce gas, bloating, etc...
|
|
|
Know this...
|
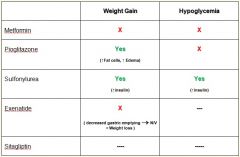
Also, Meglinitides increase weight and cause hypoglycemia by increasing insulin secretion...
|
|
|
What type of effect to meglitinides have on overnight glucose levels?
|
Little effect...
They have a quick onset of action and a short duration!! |

