![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
47-year-old female presents at her family practice physician complaining of fatigue and chronic constipation. She states that she is always cold and has gained 10 lbs in the last 4 months, even though she has not had much of an appetite. Physical exam revealed dry skin, nonpitting edema in her lower extremities, a somewhat puffy face, and a slightly enlarged thyroid. A test was positive for thyroid peroxidase antibodies. What would you most likely see on her lab test?
|
↓T3, ↓T4
This is Hashimoto's (anti-TPO) **HYPOthyroidism** |
|
|
Hashimotos and Radiation cause ____thyroidism
|
hypothyroidism
|
|
|
What are possible treatment options for primary hypothyroidism (eg. from Hashimoto’s thyroiditis)?
|
Give T3, T4
|
|
|
What is primary hypothyroidism?
|
There is a failure of the thyroid to produce sufficient thyroid hormone
|
|
|
What is secondary/tertiary hypothyroidism?
|
Diminished stimulation of thyroid by TSH d/t:
hypothalmic disease (tertiary) pituitary disease (secondary) |
|
|
What are possible treatment options for secondary hypothyroidism (eg from pituitary dysfunction)?
|
Give T3, T4
|
|
|
What are the synthetic thyroid hormone preparations?
|
Levothyroxine (T4)
Liothyronine (T3) |
|
|
Which synthetic Thyroid Hormone drug is mainly used?
|
Levothyroxine (T4)
|
|
|
Clinical Use:
- Hypothyroidism -TSH suppression therapy in patients with thyroid cancer - Occasionally those with nontoxic goiter |
Mainly Levothyroxine (T4)
|
|
|
Why would you use levothyroxine in a euthyroid patient with a nontoxic goiter?
|
There is a decreased release of TSH from pituitary
Decrease the growth and size of the goiter |
|
|
MOA: Levothyroxine in treating a nontoxic goiter
|
Blocks TSH from pituitary
Reduces size and growth of tumor reduces TH released |
|
|
What might you expect to see when treating a nontoxic goiter with levothyroxine?
|
Hyperthyroidism
(you are giving synthetic TH while the patient is still producing human TH) |
|
|
Why is levothyroxine (T4) preferred over liothyronine (T3) for hormone replacement therapy?
|
T4 is converted to T3
T4 has the longest half-life |
|
|
When might you want
to use liothyronine (T3) ? |
An emergency such as MYXEDEMA COMA.
T3 would work much faster to reverse hypothyroidism |
|
|
A 37-year-old female presents to your clinic for unintentional weight loss. Over the past 3 months, she
has lost approximately 15 lb without changing her diet or activity level. Otherwise, she feels great. She has an excellent appetite, no gastrointestinal complaints except for occasional loose stools, a good energy level, and no complaints of fatigue. She denies heat or cold intolerance. Her heart rate is 108 bpm, blood pressure 142/82 mm Hg, and she is afebrile. When she looks at you, she seems to stare, and her eyes are somewhat protuberant. You note a large, smooth, nontender thyroid gland, and her skin is warm and dry. There is a fine resting tremor. She most likely has: A. Diffuse (simple) goiter B. Graves’ disease C.Hashimoto’s thyroiditis D.Myxedema E. Toxic multinodular goiter |
Graves’ disease
(Auto-antibodies to TSH receptor) |
|
|
A 37-year-old female presents to your clinic for unintentional weight loss. Over the past 3 months, she
has lost approximately 15 lb without changing her diet or activity level. Otherwise, she feels great. She has an excellent appetite, no gastrointestinal complaints except for occasional loose stools, a good energy level, and no complaints of fatigue. She denies heat or cold intolerance. Her heart rate is 108 bpm, blood pressure 142/82 mm Hg, and she is afebrile. When she looks at you, she seems to stare, and her eyes are somewhat protuberant. You note a large, smooth, nontender thyroid gland, and her skin is warm and dry. There is a fine resting tremor. You determine she has Grave's Disease Propanolol would be useful in treating which of her symptoms? |
**Tremor**
blocks β2 on muscle **Tacchycardia** blocks β1 on heart **HTN** |
|
|
How could you treat a patient's hyperthyroidism who is diagnosed with Grave's Dz?
A. Inhibit thyroid hormone synthesis B. Inhibit thyroidhormone release C. Inhibit the thyroid hormone receptor D. Destroy thyroid tissue |
A. Inhibit thyroid hormone synthesis
B. Inhibit thyroidhormone release D. Destroy thyroid tissue |
|
|
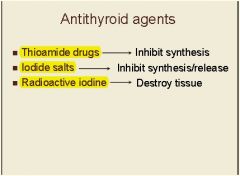
**Antithyroid Agents**
______ → inhibit synthesis ______ → inhibit synthesis/release ______ → Destroy Tissue |
|
|
|
Name the Drug Class:
Methimazole Propylthiouracil |
Thioamides
(Inhibit TH synthesis) |
|
|
MOA: Thioamides for hyperthyroidism
|
Inhibit thyroid peroxidase (TPO) from forming T3, T4
|
|
|
What enzyme catalyzes the reaction between iodide, H2O2 and TG to form MIT and DIT, and the coupling reaction between MIT and DIT to form T3 and T4?
|
Thyroid Peroxidase
|
|
|
What enzyme is involved in the
conversion of T4 to T3 in peripheral tissue? |
Thyroid Hormone Deiodinase
|
|
|
Which thioamide partially inhibits the peripheral deiodination of T4 to T3?
|
Propylthiouracil
|
|
|
MOA:
Inhibits thyroid peroxidase (TPO)-catalyzed reactions thereby blocking iodine organification (production of MIT, DIT) and iodotyrosine coupling (production of T3, T4). - This decreases thyroid hormone synthesis |
Methimazole
Propylthiouracil (Thioamides) |
|
|
Clinical Use:
- Control hyperthyroidism while waiting for spontaneous remission from Grave's Disease - Control hyperthyroidism before radioactive iodine or surgical treatment |
Methimazole
Propylthiouracil (Thioamides) |
|
|
How quickly will methimazole cause a patient with Graves’hyperthyroidism to become euthyroid?
|
A few weeks
You have stored TH and it will take a few weeks to get rid of the stored stuff |
|
|
Which theoamide agent causes a more rapid achievement of euthyroidism?
|
Methimazole
|
|
|
Which thioamide is teratogenic, ESPECIALLY during the first trimester during organogenesis?
|
Methimazole
|
|
|
Which thioamide causes hepatotoxicity and liver failure?
|
Prophylthiouracil
|
|
|
Which agent is first line for the treatment of hyperthyroidism?
|
Methimazole
(No hepatotoxicity side effects) |
|
|
Which agent would you use for hyperthyroidism during pregnancy?
A. Methimazole throughout B. Propylthiouracil throughout C. 1st – Methimazole 2nd, 3rd – Propylthiouracil D. 1st – Propylthiouracil 2nd, 3rd – Methimazole |
D. 1st – Propylthiouracil
2nd, 3rd – Methimazole (Remember, Methimazole is teratogenic during the first trimester) |
|
|
Lugol’s solution = ________
|
Iodide Salts (potassium idodide [SSKI])
|
|
|
What is 131^I- ?
|
Radioactive iodine
|
|
|
What is the difference in using
high levels of iodide salts and radioactive iodine to treat hyperthyroidism? *** |
**Iodide salts**
the effect is REVERSIBLE and transient. Improvement is seen within 2-7 days but limited to several weeks. **Radioactive Iodine** the effect is PERMANENT. Usually takes several weeks to restore thyroid hormone levels to ‘normal’. |
|
|
Clinical Use:
Destroy some of the thyroid tissue |
Radioactive iodine
|
|
|
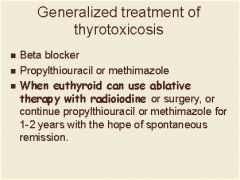
Treatment algorithm for hyperthyroidism
|
|
|
|
Adverse Effects:
Skin rash Pruritus Arthralgias Fever Nausea Agranulocytosis - rare |
Thioamides
|
|
|
What is the biggest
side effect of radioactive iodine? |
Hypothyroidism if you destroy too much tissue
|
|
|
What are the absolute contraindications to Radioactive Iodine?
|
- Pregnancy, lactation
- Inability to comply with radiation safety regulations |
|
|
You are giving a patient methimazole for graves disease and want to add a drug for preoperative treatment. What should you give them?
|
**Iodide Salts**
- Decrease vascularity, size and fragility of the hyperplastic thyroid - Lower serum thyroid hormone concentrations in patients that are not euthyroid |
|
|
Should iodide salts be used before and/or after radioactive iodine?
|
ONLY AFTER
Giving large doses of iodine before radiation would cause competition at the symporter and neither would get in the colloid space |
|
|
Which anti-thyroid drugs treat thyroid storm? Which are the quickest?
|
Iodide salts (rapid: 2-7 days)
Thioamides |
|
|
An acute, life-threatening, hypermetabolic state induced by excessive release of thyroid hormones (THs) in individuals with thyrotoxicosis.
The clinical presentation includes fever, tachycardia, hypertension, and neurological and GI abnormalities. Hypertension may be followed by congestive heart failure that is associated with hypotension and shock |
Thyroid Storm
|
|
|
What could you use to treat a
thyroid storm? A. Levothyroxine B. Methimazole C. Iodide salts D. Propranolol E. Propylthiouracil F. Radioactive iodine |
B. Methimazole
C. Iodide salts D. Propranolol E. Propylthiouracil |
|
|
Why are iodide salts given at least an hour after a thioamide in a patient with a
thyroid storm? A. Iodine will block the uptake of thioamides into the thyroid gland B. The thioamide will prevent the iodine from being used as a substrate for new thyroid hormone synthesis |
The thioamide will prevent the iodine from being used as a substrate for new thyroid hormone synthesis
|
|
|
What may be an advantage of using propylthiouracil vs methimazole in a patient with a thyroid storm?
|
Blocks the conversion of T4 to T3 peripherally
More rapid reduction in serum T3 levels |

