![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
287 Cards in this Set
- Front
- Back
|
What is the primary function of the dental pulp?
|
Formation
|
|
|
Which of the following is not a stage of tooth formation?
|
Basal
|
|
|
From what cells are odontoblasts derived?
|
Undifferentiated ectomesenchymal
|
|
|
Where does deposition of unmineralized dentin matrix begin and in what direction does it proceed?
|
Begins at cups tip and progresses cervically
|
|
|
The cervical loop is the location of which of the following?
|
Where inner and outer dental epithelium meet
|
|
|
What is the first thin layer of dentin that is formed?
|
Mantle dentin
|
|
|
Epithelial cell rests of Malassez are remnants of what?
|
Epithelial root sheath
|
|
|
Why are lateral canals clinically significant?
|
They allow pulp disease to extend to periodontal tissues
|
|
|
What morphological Changes occur to the dental pulp over time?
|
Overal size of pulp chamber is reduced
|
|
|
The cementodentinal junction (CDJ) is which of the following?
|
The area where cementum contacts dentin inside the canal
|
|
|
What is the defensive function of the dental pulp?
|
Odontoblast formation of dentin in response to injury
|
|
|
Which of the following is not a major component of the odontoblast?
|
Synaptic junction
|
|
|
What cell type is primarily related to the immune system in the dental pulp?
|
Dendritic
|
|
|
What type of collagen is the most prominent found in the dental pulp?
|
Type I
|
|
|
Which of the following is not a type of pulp stone?
|
Floating
|
|
|
Lack of knowledge of pulp anatomy is the ______________ most common cause of treatment failure.
|
Second
|
|
|
Of the following, which is the best technique to determine if a root contains 2 canals?
|
Interpreting angled radiographs
|
|
|
The shape of the canal in cross-section is variable but is almost always round in the apical third.(t/f)
|
First part true, second part false
|
|
|
Multiple canals in mandibular premolars occur most often in which population?
|
African-Americans
|
|
|
Alterations in the anatomy of the pulp space occur because of which of the following a.age b.resorption c.calcifications
|
All of the above
|
|
|
Calcifications encountered in the pulp space do which of the following?
|
Represent additional dentin formation
|
|
|
Which of the following is not associated with the radicular pulp?
|
Pulp horns
|
|
|
Accessory canals are more common in the apical 3rd, and more common in posterior teeth.(t/f)
|
Entire sentence is true
|
|
|
Which of the following are true regarding the apical foramen?
|
The foramen is most commonly located 0.5mm to 1.0mm away from the anatomic root apex
|
|
|
Dens invaginatus (dens in dente) occurs most commonly in which teeth?
|
Maxillary lateral incisors
|
|
|
The lingual groove defect is (1) found most frequently in maxillary central incisors and (2) has poor prognosis for treatment.(t/f)
|
Statement 1 is false, statement 2 is true
|
|
|
A C-shaped canal is characterized by which of the following?a.Has complex internal anatomy b.Is most commonly found in the Asian population c.Usually occurs in mandibular 2nd molars d.Should be referred to an endodontist for tx
|
All of the above
|
|
|
Of the following, which tooth or root is the most likely to have 2 canals?
|
Mandibular 1st molar mesial root
|
|
|
The lingual root of the maxillary first molar often has a curvature in the apical third to which of the following?
|
Buccal
|
|
|
Diagnostic radiology is helpful in all of the following except: a.Identifying pathosis b.Determining root anatomy c. Determining pulp anatomy
|
Determining pulp responsiveness
|
|
|
What are working length radiographs?
|
Radiographs determine the distance from radiographic apex to a reference point
|
|
|
Radiographs are useful to evaluate the following qualities of an obturation except which of the following?
|
Sealer thickness
|
|
|
Radiographs are useful in evaluating success and failure at recalls because they do which of the following?
|
May show failures that often occur without adverse signs or symptoms
|
|
|
The most accurate radiographs are made by doing which of the following:
|
Using a paralleling device
|
|
|
Use of a paralleling technique may not be feasible when which of the following occurs:
|
There are maxillary tori
|
|
|
F speed film requires how much less exposure compared to E speed film?
|
20-25%
|
|
|
What does the con-image shift do?
|
It assists in identifying superimposed canals
|
|
|
What occurs as cone position moves away from parallel?
|
Lingual object moves relatively in same direction as the cone
|
|
|
Which is the disadvantage of the cone-image shift?
|
It may superimpose normal anatomic structures over the root apex
|
|
|
Which of the following is a distinguishing characteristic of a radiolucent lesion of endodontic pathosis?
|
The radiolucency stays at the apex regardless of cone angulation
|
|
|
A radiolucency of endodontic origin is usually present which what type of pulpal diagnosis?
|
Necrotic pulp
|
|
|
What is the usual radiographic appearance of condensing osteitis?
|
Diffuse radiopaque appearance
|
|
|
A mesial projection cone adjustment during working length radiographs is indicated for what?
|
Maxillary molars with a ML canal
|
|
|
Digital radiography has not been proven to do which of the following?
|
Provide superior image quality
|
|
|
Which of the following is not a main portal of entry for microogranisms to enter the dental pulp?
|
Occlusal grooves
|
|
|
Why is there greater dentin permeability near the pulp?
|
Higher density of dentinal tubules
|
|
|
Exposed dentin provides an unimpeded access for bacteria to enter the pulp.(t/f)
|
False
|
|
|
What is anachoresis?
|
Microorganisms transport from blood vessels into damaged tissue
|
|
|
Root canals can become infected through anachoresis.(t/f)
|
False
|
|
|
Which of the following is not a category of intraradicular infections? A.Primary b.Secondary c.Tertiary d.Persistent
|
tertiary
|
|
|
The most common microorganisms in primary endodontic infections are
|
Gram-negative bacteria
|
|
|
Which of the following is not a source of nutrients for bacteria within the root canal system?
|
Inflamed vital pulp tissue
|
|
|
Which of the following microorganisms are commonly present in large percentages of root canal- treated teeth that present with persistent apical periodontitis, indicative of failed treatment?
|
Enterococcus faecalis
|
|
|
Gram-positive bacteria have been demonstrated to a.Have higher occurrence in post-instrumentation samples b.Are more resistant to anti-microbial treatment c.Are able to adapt to harsh environmental conditions
|
All of the above
|
|
|
A direct pulp exposure of a carious lesion is necessary to have a pulpal response and inflammation(t/f)
|
False
|
|
|
What factor is the most important in determining if pulp tissue becomes necrotic slowly or rapidly after carious pulp exposure and pulpal inflammation?
|
Lymph drainage
|
|
|
What is necessary for pulp and periradicular pathosis to develop?
|
Presence of bacteria
|
|
|
Which of following statements is true regarding mechanical irritants?
|
Operative procedures without water coolant cause more irritation than those performed under water spray
|
|
|
What nonspecific inflammatory mediators are not present when the dental pulp is irritated?
|
Epinephrine
|
|
|
What cell type associated with immune response is not present in severely inflamed dental pulp?a.T-lymphocytes b.B-lymphocytes c.Macrophages
|
Odontoclasts
|
|
|
What is the cause of pain during progression of pulpal injury?
|
Increase of venule vascular permeability
|
|
|
What is reversible pulpitis?
|
Yields a positive response to thermal pulp testing
|
|
|
What is irreversible pulpitis?
|
A severe inflammatory process
|
|
|
Which of the following is not a hard tissue change that may result from pulpal irritation or inflammation?a.Calcification of pulp tissue spaces b.Resorption of pulp tissue spaces c.Formation of pulp tissues
|
Thickening of PDL
|
|
|
What are the signs and symptoms associated with symptomatic apical periodontitis (acute apical periodontitis)?
|
Marked or excruciating pain on tapping with a mirror handle
|
|
|
What histologic feature differentiates a periapical granuloma from a periapical cyst?
|
Presence of an epithelial lined cavity
|
|
|
Which of the following is not associated with acute apical abscess? A.Moderate to severe discomfort b.Negative response to electric pulp testing c.Tenderness to percussion and palpation
|
Intense and prolonged response to thermal stimulus
|
|
|
What factors may impact and influence whether periradicular lesions heal completely or incompletely? A.Size of the lesion b.Blood supply c.Systemic disease
|
All of the above
|
|
|
What is the most important aid in distinguishing between endodontic and non-endodontic periradicular lesions
|
Pulp vitality testing
|
|
|
tooth development begins when?
|
6th week of embryonic life
|
|
|
3 stages of tooth development
|
bud cap and bell
|
|
|
most important stage of tooth development
|
bell-major tooth and crown development
|
|
|
what forms enamel
|
enamel organ
|
|
|
what forms dentin and pulp
|
enamel papilla
|
|
|
what forms the pdl (cementum, bone, and sharpeys fibers
|
dental follicle/dental sac
|
|
|
what is made of ectodermal cells
|
enamel organ
|
|
|
whats made of ectomesenchymal cells
|
dental papilla and follicle
|
|
|
what cells make:
enamel dentin cememntum bone sharpey fibers |
ameloblast
odontoblast cementoblast osteoblast fibroblast |
|
|
what forms first, dentin or enamel?
|
dentin
|
|
|
Explain the differentiation of IEE into forming enamel?
|
IEE differentiates into ameloblasts, which differentiates ectomesenchymal cells of papilla into odontoblasts which then stimulates secretion of dentin then in turn stimulates ameloblasts to secrete enamel
|
|
|
Hertwig's Epithelial Root Sheath (HERS) is formed from
|
IEE and OEE
|
|
|
HERS determines?
|
size and shape of roots of the teeth
|
|
|
when does cementum form?
|
when HERS fragments, exposing dentin to the dental follicle, allowing cementum to be laid down
|
|
|
what are the Epithelial Rests of Malassez?
|
remnants of HERS in the PDL
|
|
|
Epithelial Rests of Malassez are involved in forming what?
|
radicular cysts during chronic inflammation
|
|
|
before dentin is formed, breaks in HERS can form?
|
accessory and lateral canals
|
|
|
accessory and lateral canals are most common in the?
|
apical third of the root
|
|
|
accessory and lateral canals can act as passageways for?
|
bacteria and their by products to communicate btw the PDL and the tooth
|
|
|
HERS stops when
|
root formation is complete and apical foramen is closed
|
|
|
major apical foramen is located where? apex of the root or coronal to it?
|
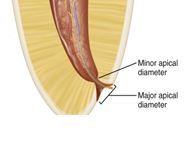
coronal
|
|
|
apical foramen is how large
|
0.3-0.6mm (funnel shaped)
|
|
|
narrowest portion of the apical foramen is the?
|
apical constriction-0.5mm from Major apical diameter
|
|
|
what are the 5 functions of the pulp?
|
induction
formation nutrition defense sensation |
|
|
what is the pulp function of induction?
|
dentin formation induces enamel formation
|
|
|
what is the pulp function of formation?
|
odontoblast forms dentin. MOST IMPORTANT FUNCTION
|
|
|
what is the pulp function of nutrition?
|
nutrients to cells through vascularity
|
|
|
what is the pulp function of defense?
|
macrophages, dendritic cells, lymphocytes, and tertiary.sclerotic dentin is formed
|
|
|
what is the pulp function of sensation?
|
pain sensation, a delta and c fibers
|
|
|
what is 70% inorganic and 20% organic?
|
dentin
|
|
|
what makes up of type 1 collagen?
|
dentin
|
|
|
which type of dentin is formed before the tooth erupts?
|
primary dentin
|
|
|
what type of dentin forms after the tooth erupts and throughout life
|
secondary dentin
|
|
|
type of dentin that forms from a pathologic process (caries and trauma)
|
tertiary dentin
|
|
|
type of dentin that protects pulp from noxious stimuli and injury
|
tertiaty dentin
|
|
|
what are the types of tertiaty dentin?
|
reactionary and reparative
|
|
|
type of tertiary dentin formed from the original odontoblasts
|
reactionary
|
|
|
type of tertiary dentin from new/replacement odontoblasts
|
reparative
|
|
|
calcified pulp chambers/canals form from
|
excessive secondary and tertiary dentin
|
|
|
3 layers of dentin are
|
mantle
circumpulpal predentin |
|
|
1st layer of dentin formed is
|
mantle
|
|
|
mantle dentin is formed from this type of dentin
|
primary
|
|
|
circumpupal dentin is formed from what types of dentin
|
primary and secondary
|
|
|
why is it easier for bacteria to infect the pulp?
|
dentinal tubules are wider and more concentrated at the pulp compared to the DEJ
|
|
|
what type of dentin is located between the tubules?
|
intertublar
|
|
|
what dentin lines the dentin tubules
|
intratubular/peritubular
|
|
|
whats more mineralized intertubular or inratubular dentin
|
intratubular
|
|
|
whats the process of blocking dentinal tubules in response to stimuli and decreasing permeability?
|
dentinal scleroris
|
|
|
pulp zone next to predentin
|
odontoblast layer
|
|
|
next to odontoblast layer and contains capillary and sensory nerve fiber plexus (Plexus of Rashkow)
|
cell free zone
|
|
|
zone contains high proportions of fibroblasts and immune cells
|
cell rich zone
|
|
|
zone thats the central mass of pulp and contrains vessels and nerves. COMMON CELL TYPE IS FIBROBLASTS
|
Pulp proper
|
|
|
____are post mitotic and do NOT undergo cell division
|
odontoblasts
|
|
|
makes type 1 and 3 collagens, GAGs, and most common cell type in pulp
|
Fibroblasts
|
|
|
most common immune cell in pulp
|
dendritic cells
|
|
|
acts as APC
|
Dendritic and Macophages
|
|
|
acts as a scavenger and an APC
|
macrophages
|
|
|
pro-inflammatory mediators
|
Macrophages
|
|
|
activate macophages and b cell antibody production
|
t-lymphocytes
|
|
|
present in injured pulps only
|
mast cells
|
|
|
in a 55:45 ratio in the pulp
|
Collagen type 1 and 3
|
|
|
acts as a sieve for nutrients and provides tissue tugor
|
GAGs/Proteoglycans
|
|
|
blood vessels in the pulp
|
arterioles, cappillaries and venules
|
|
|
shunting system for pulp injury and repair
|
arteriovenous and venovenous
|
|
|
helps remove tissue fluid buildup
|
lymphatic vessels
|
|
|
younger or older people pulp are more vascular?
|
younger-more vascular, easier to repair
|
|
|
coronal vascular supply is almost ______ that of radicular region
|
twice, because more odontoblasts and fibroblasts in those locations so need more nutrients
|
|
|
venules drain POSTERIORLY into
|
maxillary vein
|
|
|
venules drain ANTERIORLY into
|
facial vein
|
|
|
what vessels decrease intersititial fluid pressure
|
lymphatics
|
|
|
regulation of pulpal blood flow is controlled by
|
Sympathetic Autonomic System-vasoconstriction
|
|
|
inflammed pulp is controlled by
|
neuronal regulation
-A, c-fibers release neuropeptides and cause vasodilation |
|
|
changes in pulp during inflammation
|
increase:
vascular permeability intersitial tissue fluid/proteins |
|
|
pulp is a _____-______ environment
|
non-compliant environment
|
|
|
because of it being non-compliant what occurs when theres inflammation of the pulp
|
strangulation of the pulp
|
|
|
Self Strangulation Theory
|
in Tissue pressure causes strangulation of vessels, generalized collapse of all venules, cessation of blood flow and subsequent ischemia and necrosis
|
|
|
Does the Self stangulation theory still hold true?
|
No-Capillaries localize blood to specific area of injury – localization of tissue fluid pressure to injured area
DOES NOT AFFECT THE WHOLE PULP |
|
|
Normal Pulpal Tissue Fluid Pressure is maintained adjacent to injured area by
|
1. increase intraluminal pressure of local capillaries-equal with outside pressure
2.increase exchange of nutrients/waste 3. anastomoses 4.lymphatic drainage ALL RESULT IN LOCALIZED INFLAMMATION |
|
|
what happens if the insult is removed and if it is not removed
|
pulp heals or becomes necrotic
|
|
|
maxillary teeth are innervated (sensory) by what?
|
V2
|
|
|
mandibular teeth are innervated (sensory) by what?
|
V3
|
|
|
the 2 sensory fibers of the pulp?
|
a-fibers (myelinated) and c-fibers (unmyleinated)
|
|
|
whats more abundant in the pulp, a or c fibers?
|
c fibers
|
|
|
two types of A fibers and which is more abundant
|
delta-more abundant
beta |
|
|
nerve bundles pass through pulp and ramify into _______ in the subodontoblastic cell free zone
|
plexus of rashkow
|
|
|
fibers located in or near the odontoblast layer
|
a fibers
|
|
|
fibers within the pulp not near the odontoblast layers or cell free layers
|
c fibers
|
|
|
fastest conducting fibers and deals with pressure and touch
|
a beta
|
|
|
fibers for pain temperature and touch
|
a delta
|
|
|
pain sensation fibers
|
c fibers
|
|
|
all sensory nerve fibers in pulp/dentin function as
|
nociceptors
|
|
|
all afferent impulses generate the sensation of ____
|
pain
|
|
|
sharp/pricking pain, low threshold for exicitation
|
a-delta
|
|
|
burning aching less bearable pain, high threshold for excitation
|
c fibers
|
|
|
explain dentinal hypersensitivty
|
Fluid in dentinal tubules moves in response to painful stimuli
Thermal, mechanical, chemical, hyperosmotic stimuli |
|
|
a-fibers act as ______receptors
|
mechanoreceptors activated by movement of fluid = Dentinal Pain (sharp)
|
|
|
causes inward flow during the Hydrodynamic Theory
|
heat
|
|
|
causes outward flow during the Hydrodynamic Theory
|
cold
air hyper-osmotic |
|
|
what causes a stronger nerve response, inward or outward flow
|
outward
|
|
|
pulp stone: surrounded by pulp tissue
|
free stones
|
|
|
pulp stone: continuous with dentin
|
attached
|
|
|
pulp stone: surrounded entirely by dentin
|
embedded
|
|
|
calcifications cause what type of pain symptoms and how big do they get when you feel the pain?
|
tricky ricky at it again. NOT RESPONSIBLE FOR PAIN SYMPTOMS REGARDLESS OF SIZE-can block access to canals during RCT
|
|
|
what occurs when to pulp as we grow older
|
Decreased cellularity
Decreased vascularity Decreased innervation Increased number and thickness of collagen fibers |
|
|
3 types of cementum
|
Acellular afibrillar cementum:
Acellular extrinsic fiber cementum: Cellular intrinsic fiber cementum: |
|
|
Acellular afibrillar cementum:
|
Covers the teeth at and along the cemento-enamel junction (CEJ)
|
|
|
Acellular extrinsic fiber cementum
|
Confined to the coronal half of the root
|
|
|
Cellular intrinsic fiber cementum
|
is Confined to the apical half of the root
|
|
|
Cementum acts as an attachment for between the bone
|
sharpeys fibers
|
|
|
functions of the PDL
|
Supports the tooth
Absorb occlusal forces Keep tooth in socket |
|
|
connects the PDL to the tooth?
|
sharpeys fibers
|
|
|
more abundant in PULP a-delta or beta fibers?
|
delta
|
|
|
more abundant in PDL a-delta or beta fibers?
|
beta
|
|
|
a beta fibers in pdl
|
Allows patient identification of tooth with apical periodontitis-tap on it and can tell which tooth is tapped on
|
|
|
Radiopaque appearance on radiographs of alveolar bone is the
|
lamina dura
|
|
|
cause of radiographic loss of lamina dura
|
periapical inflammation
|
|
|
highest portion of the pulp-most likely for pulp exposure.
|
pulp horns
|
|
|
opening of the tooth
|
apical foramen
|
|
|
side of root to furcation area
|
lateral canal
|
|
|
bottom of pulp chamber
|
furcation canal
|
|
|
where do you stop instrumentation
|
at the apical constriction-minor apical diameter
|
|
|
Weine Classification: one single canal with one foramen
|
type 1
|
|
|
Weine Classification: two canals converging to one foramen
|
type 2
|
|
|
Weine Classification: two canals and two foramina
|
type 3
|
|
|
Weine Classification: one canal dividing into two canals with two separate foramina
|
type 4
|
|
|
Maxillary Central Incisor
|
Single root
Single canal most of the time Triangular pulp chamber outline Pulp chamber usually has 3 pulp horns (mesial, center and distal) Average age of eruption: 7-8 yrs Average age of calcification: 10 yrs |
|
|
occurs 2-3yrs after eruption
|
calcifications
|
|
|
______ prevents direct access to the root canal and deflects files labially, often resulting in a ledge or perforation
|
lingual shoulder
|
|
|
Maxillary Lateral Incisor
|
Single Root
Single canal most of the time Average age of eruption: 8-9 yrs Average age of calcification: 11yrs Usually has two pulp horns (mesial & distal) Access outline similar to max. central incisor, however slightly more compressed, due to less prominent pulp horns |
|
|
Maxillary Canine
|
Single root
Single canal most of the time No pulp horns Oval external access outline due to absence of pulp horns Pulp chamber wider buccolingually than mesiodistally Average age of eruption: 10-12 yrs Average age of calcification: 13-15 yrs |
|
|
pulp chambers
|
Wider BL than MD for Max Canine
Wider MD than BL for Mx Central and Lateral |
|
|
Mandibular Incisors
|
2 canals common – 20-40% (division occurs in coronal –middle third). into one foramen-type 2 weine
pulp chamber/root canal is wider labiolingually than mesiodistally Access outline usually oval-triangular Average age of eruption: 6-8 yrs Average age of calcification: 9-10 yrs |
|
|
where must you open the mandibular incisors
|
lingually towards cingulum as the 2nd canal is often missed
|
|
|
Mandibular Canine
|
Oval access outline form consistent with pulp chamber (wide buccolingually and narrow mesiodistally)
Similar to Max canine, however dimensions are smaller and presence of 2 roots and 2 canals is not uncommon Average age of eruption: 9-10 yrs Average age of calcification: 13 yrs |
|
|
Maxillary 1st Premolar
|
May have one, two, or three roots and canals; it most often has two roots with two canals
Buccal and lingual (palatal) pulp horns and a pulp chamber that is wider buccolingually than mesiodistally Oval external access outline form Average Age of eruption: 10-11 yrs Average age of calcification: 12-13 yrs |
|
|
because of this on Maxillary 1st premolars, if exteneded prep can cause perforation
|
mesial concavity
|
|
|
cuspal coverage Mx 1st and 2nd Premolar needed after RCT because
|
mesiodistal root and buccal cusps prone to fracture
|
|
|
Maxillary 2nd Premolar
|
About 50% of time 2 canals at the apex, and then converges.
Has one root most of the time ~85% single root Root canal morphology 75 % - 1 canal at apex Buccal and lingual (palatal) pulp horns with pulp chamber wider buccolingually than mesiodistally. Buccal pulp horn larger than lingual Oval external access outline form BL>MD Average Age of eruption: 10-12 yrs Average age of calcification: 12-14 yrs |
|
|
Mandibular 1st Premolar
|
BL>MD
Two pulp horns are present: a large, pointed buccal horn and a small, rounded lingual horn 74% one canal 2 roots – 5.5% (3 times higher incidence in African-American) Access outline: Oval Common to have 2 canals. And usually split. Weine type 4. Average age of eruption: 10-12 yrs Average age of calcification: 12-13 yrs |
|
|
Mandibular 2nd Premolar
|
Pulp chamber and access outline - Oval
Two roots – 1.5% (3 times higher incidence in African-Americans) Root canal morphology: 97.5% one canal Average age of eruption: 11-12 yrs Average age of calcification: 13-14 yrs |
|
|
need to remove lingual shoulders on these teeth
|
Maxillary and Mandibular anteriors
|
|
|
Mx 1st Molar
|
Usually has three roots that are widely spread buccolingually
Pulp chamber widest in the buccolingual dimension, and four pulp horns are present Pulp chamber and access outline triangular to rhomboid Average age of eruption: 6-7 yrs Average age of calcification: 9-10 yrs |
|
|
MB root of Mx 1st Molar
|
70-95% 2 canals. 2nd canal is ML or MB2.
Widest buccolingually |
|
|
Palatal/Lingual root of Mx 1st Molar
|
The palatal root is the longest, has the largest diameter, and generally offers the easiest access. From the orifiice, it is wide mesiodistally
|
|
|
Mx 2nd Molar
|
Morphology similar to 1st molar, however roots and pulp horns are closer to each other and lengths are slightly shorter
Two roots with two canals is not uncommon – 8% have only B & P canals Lower incidence of MB2 (ML) canal relative to 1st molar Average age of eruption: 11-13 yrs Average age of calcification: 14-16 yrs Pulp chamber and canals smaller MD when compared to first molar |
|
|
Md 1st Molar
|
Earliest permanent posterior tooth to erupt and is the tooth that most often requires root canal therapy
Usually has two roots but occasionally it can have three. 3 canals – 64% (Weine Type III ~60%)-2 mesial 1 distal Average age of eruption: 6 yrs Average age of calcification: 9-10 yrs Middle mesial-btw mesial buccal and mesial lingual and joins with either. Pulp chamber floor is roughly trapezoid |
|
|
Md 2nd Molar
|
Pulp chamber similar to 1st molar but slightly smaller and more compressed
Access outline more triangular Presence of only 2 canals (single mesial and distal) more common than in 1st molars Average age of eruption: 11-13 yrs Average age of calcification: 14-15 yrs Most frequent tooth to fracture. Bc smaller and occlusal table smaller and cant stand a lot of force. And bc of its location in the tooth Mesial root always curves out and then in Distal root curve straight. |
|
|
third molars
|
Radicular anatomy of maxillary and mandibular 3rd molars are highly unpredictable and vary greatly
Root canal morphology – Anywhere from 1-4 roots with 1-6 root canals |
|
|
common 3rd molar features
|
-Fused root system
-Short rounded crowns and conical roots -Larger chamber area and shorter canal spaces -Malalignment of the tooth may be a factor in treatment. |
|
|
c-shaped canals are most common in
|
Md 2nd molar
7-8% of time and most in asians. |
|
|
what is a c shaped canal
|

is a single, ribbon-shaped orifice with an arc of 180 degrees or more. The result is a large curved orifice.
C-shaped-orifcaces shaped and arced in 180 degrees to apical foramen. Harder to treat and tissue in btw that’s harder to clean. A lot of anastomoses and communicated with other orifices. Greater failure rate. |
|
|
The floor of the pulp chamber is always located in the center of the tooth at the level of the CEJ
|
Law of Centrality
|
|
|
The walls of the pulp chamber are always concentric to the external surface of the tooth at the level of the CEJ, that is, the external root surface anatomy reflects the internal pulp chamber anatomy
|
Law of Concentricity
|
|
|
Except for the maxillary molars, canal orifices are equidistant from a line drawn in a mesiodistal direction through the center of the pulp chamber floor
|
First law of Symmetry
|
|
|
Except for the maxillary molars, canal orifices lie on a line perpendicular to a line drawn in a mesiodistal direction across the center of the pulp chamber floor
|
Second Law of Symmetry
|
|
|
The pulp chamber floor is always darker in color than the walls
white walls, yellow pulp tissue |
law of color change
|
|
|
The orifices of the root canals are always located at the junction of the walls and the floor
|
Law of orifice location:
|
|
|
3 uses/importance for Radiographs
|
diagnosis
treatment recall |
|
|
identifying pathosis
determining root and pulpal anatomy characterizing normal structures |
diagnosis
|
|
|
determining working lengths
locating canals obturation |
treatment
|
|
|
healing of the pathosis
determining other treatment options |
recall
|
|
|
primary radiograph used in endodontics is the
|
Periapical Radiograph or PA.
|
|
|
Periapical Radiograph or PA.
|
-At least 2mm of bone should be visible beyond the apex of the tooth.
-Entire periapical lesion should be visible |
|
|
Limitations of Radiographs
|
-Two dimensional representation of a three dimensional object
-Superimposition of anatomic structures -Lesion appears in the radiograph only after certain amount of destruction of bone |
|
|
How is a panoramic radiography used for diagnosis?
|
its not. CANT BE USED FOR DIAGNOSIS of endodontic
|
|
|
Buccal object rule
SLOB Clarks Rule Cone Shift Technique |
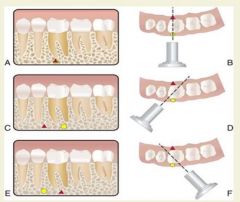
A lingual object will move in the same M/D direction as the x-ray cone head, whereas a buccal object will move in the opposite M/D direction (Same Lingual Opposite Buccal)
|
|
|
ideal SLOB shift is
|

20 degrees
|
|
|
SLOB allows for:
|
-Location of additional canals and/or roots
-Distinction between superimposition of structure -Determination of buccal or lingual position of anatomical features or iatrogenic mishaps |
|
|
PAs distort easily so take BWs as well because:
|
in order to minimize elongation or foreshortening.
|
|
|
BW’s more accurately depict the
|
-depth of caries
-extent of restorations -morphology of pulp chambers -presence of open margins -size, position and depth of posts |
|
|
Most accurate periapical radiograph is achieved using the ________ ___________
|
paralleling technique
|
|
|
paralleling technique
|
The film is placed parallel to the long axis of the tooth and the central beam is directed at right angles to the film.
Most accurate representation of the tooth |
|
|
The ________ ________ ________ is used during anatomic configurations (i.e., shallow palate)
|
bisecting angle technique
|
|
|
bisecting angle technique
|
The central beam is directed at an imaginary line that bisects the angle between the tooth and film.
|
|
|
Tissue destruction and Radiographs
|
-Tissue destruction is usually more extensive than it appears radiographically.
-12.5% of cortical plate and/or 7.4 % of mineralized bone has to be destroyed before it appears on the radiograph. |
|
|
Differential Diagnosis
|
1. Conduct vitality tests, the presence or absence of symptoms and possible etiology.
2. Take multiple radiographs from different angles and use the SLOB rule to evaluate the situation 3. In the case of anatomical radiolucencies, the healthy tooth in question should also exhibit an intact lamina dura and PDL space. 4. Finally, knowing your anatomy will prevent a misdiagnosis! |
|
|
Goldman 1974 Study
|
These 6 examiners agreed on less than 50% of the cases. Six to eight months later, 3 of the original examiners again viewed the same radiographs. They agreed with their own previous responses 75% to 83% of the time!
|
|
|
2011 Tewary Hartwell Study
|
digital radiographs.
Conclusion: The interpretation of radiographs is subjective and most important factors are years of experience of examiner and their familiarity with digital systems. |
|
|
Tools for Diagnosis
|
-Chief Complaint
-History of signs and symptoms -Clinical examination -Radiographs (Should be ordered after the clinical examination) |
|
|
The goals of endodontic treatment are to
|
-Prevent the development of and treat apical periodontitis
-Create adequate conditions for periradicular tissue healing |
|
|
An inflammatory disease of microbial origin caused primarily by infection of the root canal system
|
Apical Periodontitis
|
|
|
two types of apical periodontitis
|
symptomatic and asymptomatic
|
|
|
prevalence
|
As people age and grow.-preavalence is 1/3rd but then almost doubles as you get to over 60yrs old
|
|
|
Etiology of apical periodontitis
|
Infection of the pulp tissue caused by caries or other pathways is the primary cause of apical periodontitis*
caries from coronal area into pupal space. |
|
|
Other etiologies
|
-Physical insults(overinstrumentation, overfilling)
-Chemical insults (irrigants, intracanal medication, root canal filling materials) -Traumatic injury to the periapical tissues -Foreign bodies |
|
|
the periapical tissue reaction to irritants emerging from the root canal system that manifests as vasodilation, increased vascular permeability and exudation
|
Apical inflammation
|
|
|
physical presence of pathogenic microorganisms in the periapical tissues that subsequently produce tissue damage
|
Apical infection
|
|
|
Routes of Root Canal Infection
|
-Caries, fractures, exposed dentinal tubules
-Coronal leakage -Via periodontium -Anachoresis |
|
|
Caries, fractures, exposed dentinal tubules
|
Non motile-travel by reproducing themselves. And travel through dentinal tubules. Or hydrostatic prassures and fluid pushes them through tubules into the pulp. –fight with inflammation.
|
|
|
main bacteria
|
lactobacillus and step mutans
|
|
|
microbial ingress to the root canal system after obturation
|
coronal leakage
|
|
|
via periodontium
|
Microbial access to the dental tubules by periodontal disease
|
|
|
localization of blood-borne bacteria during bacteremia to a site of inflammation
|
anachoresis
|
|
|
degree of pathogenicity or disease producing ability of a microorganism
|
virulence
|
|
|
Characteristics of a microorganism that enable it to induce disease
|
virulence factors
|
|
|
radiographic examination
|
-Widening of the periodontal ligament space
-Development of apical osteolytic lesions due to bone resorption -The loss of bone is mainly caused by activated osteoclasts. |
|
|
The inflammation-induced bone resorption in the periapical tissues is accompanied by
|
recruitment of immune cells which essentially build a defensive line against the spread of microbial invasion from the root canal (immune response)
|
|
|
thick peptidoglycan
|
Gram +
|
|
|
thinner wall and outer membrane. also has LPS-pathogenic factor
|
Gram -
|
|
|
sessile multicellular microbial community characterized by cells that are firmly attached to a surface and enmeshed in a self-produced matrix of extracellular polymeric substance (EPS), usually polysaccharide
|
biofilm
|
|
|
Microorganisms entering the pulp and periapical tissues must be able to :
|
-Colonize
-Evade host defense mechanisms -Initiate tissue destruction -Deal with variable conditions within the root canal system |
|
|
two types of endo infections
|
intraradicular and extraradicular
|
|
|
Intraradicular Infection: Primary Infection
|
Caused by microorganisms that initially invade and colonize necrotic pulp tissue (initial or “virgin” infection)
|
|
|
Intraradicular Infection: Secondary Infection
|
Caused by microorganisms not present in the primary infection but introduced in the root canal at some time after professional intervention (i.e., secondary to intervention)
usually with failed RCT |
|
|
Intraradicular Infection: persistent infection
|
Caused by microorganisms that were members of a primary or secondary infection and in some way resisted intracanal antimicrobial procedures and were able to endure periods of nutrient deprivation in treated canals
|
|
|
obligate anaerobes are found in the
|
apical area-slow growing
|
|
|
facultative anaerobes are found in the
|
coronal part of the canal-rapidly growing
|
|
|
most common fungal infection
|
candida albicans
|
|
|
maybe associated with irreversible pulpitis and apical periodntitis
|
Epstein barr virus
|
|
|
present in dental pulp but not required for development of acute apical abscess or cellulitis of endodontic origin
|
Herpes Virus
|
|
|
Predominantly Gram negative anaerobic rods
|
Primary endodontic infections
|
|
|
Gram positive facultative anaerobes
|
Previously treated canals
|
|
|
Detected in failed treatment 3x more than primary Tx
|
Enterococcus faecalis
|
|
|
characterized by microbial invasion of the inflamed periradicular tissues and is a sequel to the intraradicular infection
|
Extraradicular infection
|
|
|
It can be dependent on or independent of the intraradicular infection
|
Extraradicular infection
|
|
|
dependent on the intraradicular infection
|
take care of intraradicular infection, then extra goes away
|
|
|
independent of the intraradicular infection
|
live by itself no matter of the intraradicular infection
Independent extraradicular infections would be those that are no longer fostered by the intraradicular infection and can persist even after successful eradication |
|
|
If bacteria from the infected root canal gain entry into the periradicular tissues and the immune system is unable to suppress the invasion, an otherwise healthy patient eventually shows signs and symptoms of an acute apical abscess, which can in turn evolve to cellulitis
|
fascial space infections
|

