![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back
|
A reproductive system contains what three groups of organs?
|
- Gonads
- Reproductive ducts - External genitalia |
|
|
Where are the gametes produced?
|
Paired gonads aka sex glands
|
|
|
What is the primary origin of the sex steroid hormones?
|
Paired gonads aka sex glands
|
|
|
Once produced, where do gametes pass?
|
Through series of Reproductive Ducts
|
|
|
What happens in the Reproductive Ducts?
|
- Gametes pass through here
- In the female, the ducts are a site for development of the embryo - Also provides for the events of parturition |
|
|
What organ is involved in gamete delivery and reception during coitus?
|
External Genitalia
|
|
|
What are the two components of establishing "sex"?
|
- Sex determination = genetic sex
- Sex differentiation = phenotypic sex |
|
|
What is established during sex determination? How?
|
Genetic Sex
- Established by the complement of sex chromosomes in the genome |
|
|
When is sex determination (genetic sex) established?
|
At fertilization when the male and female gamete form a zygote having either XY or XX sex chromosome content
|
|
|
What is established during sex differentiation? How?
|
Phenotypic Sex
- Influenced by genetic and epigenetic factors |
|
|
When is sex differentiation (phenotypic sex) established?
|
Occurs during and after the embryonic period
|
|
|
What influences the sex differentiation (phenotypic sex) in the male direction?
|
Presence of androgens during formation of sex organs
|
|
|
What is the monohormone theory of sexual differentiation?
|
- Presence of androgens during formation of sex organs influences sex differentiation in a male direction
- If no androgens are present, the fetus continues to develop female sex organs |
|
|
What happens to a male if castration occurs before sexual differentiation?
|
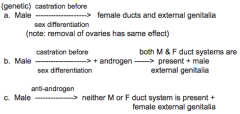
Formation of female ducts and external genitalia (female phenotype with male genotype)
|
|
|
What happens to a male if castration occurs before sexual differentiation but androgens are added?
|
Both male and female duct systems are present but with male external genitalia
|
|
|
What happen to a male if he is given anti-androgen?
|
Neither male or female duct system is present but with female external genitalia
|
|
|
Why would a castrated male given androgens develop both male and female duct systems and male external genitalia?
|
- Androgen alone is not able to promote regression of the female ducts
- Müllerian Inhibiting Substance (MIS) or Factor (MIF) or Anti-Müllerian Hormone acts on the precursors of the oviducts, uterus, and part of the vagina - Binding of MIS to its receptors causes apoptosis of the paramesonephric ducts |
|
|
What is the term for the precursors of the oviducts, uterus, and part of the vagina?
|
Paramesonephric or Müllerian Ducts
|
|
|
What is the action of Müllerian Inhibiting Substance (MIS) or Factor (MIF) or Anti-Müllerian Hormone?
|
Binding of MIS to its receptors on the paramesonephric aka Müllerian ducts causes apoptosis of the future oviducts, uterus, and part of the vagina
|
|
|
How is sexual differentiation in the brain controlled?
|
- Occurs in the brain centers controlling the pituitary
- Pulsatile release of gonadotrophin releasing hormone from hypothalamus controls male or female patterns of gonadotropin release from pituitary gland - In males, differentiation of brain is caused by a surge of T at about 6 months after birth |
|
|
When are reproductive organs morphologically indistinct with respect to sex differentiation?
|
During the Indifferent Stage (weeks 4-6), this stage is longer for the genitalia
|
|
|
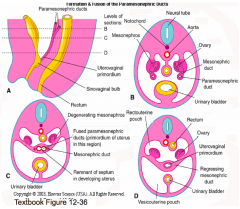
What precursor tissue forms the gonads? How does this occur?
|
- Ventromedial portion of the nephrogenic ridge as a proliferation of the overlying coelomic epithelium and the ridge mesenchyme
- Nephrogenic ridge now becomes known as the Urogenital (UG) Ridge |
|
|
What happens to the ventromedial portion of the nephrogenic ridge to form the gonads?
|
- Proliferation of the overlying coelomic epithelium and the ridge mesenchyme
- Nephrogenic ridge now becomes known as the Urogenital (UG) ridge |
|
|
What are the original gonad cell types?
|
- Germinal cells
- Supporting cells - Interstitial or steroid producing cells |
|
|
What do the primordial germ cells form from?
|
Extragonadal origin probably from cells in the epiblast (exact precursor has not been identified)
|
|
|
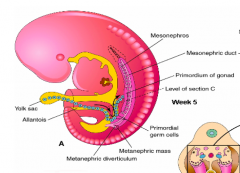
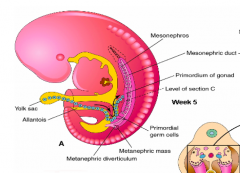
When and where are primordial germ cells first seen?
|
Yolk sac wall during week 3 as large cells with a unique staining pattern
|
|
|
What happens to the primordial germ cells first seen in the yolk sac wall during week 3?
|
During week 4-5, they migrate to the gonad within the dorsal mesentery of the hindgut
|
|
|
What happens to the primordial germ cells after they migrate to the gonad during week 4-5?
|
- During week 5-6, the germ cells proliferate as they migrate and continue to divide after they have reached the gonad
- Once they become associated with or surrounded by epithelial supporting cells derived from a proliferation of the coelomic epithelium |
|
|
What are the gonadal supporting cells in males and females? Function?
|
- Sertoli cells (M)
- Granulosa cells (F) - They play a role in organizing the gonad |
|
|
What are the gonadal interstitial cells in males and females? Function?
|
- Leydig cells (M)
- Theca cells (F) - Synthesize and secrete steroid hormones (primarily androgens) |
|
|
What kind of cells are Sertoli cells (M) and Granulosa cells (F)? Origin?
|
Supporting cells
- Originate from cord-like proliferations of the coelomic epithelium overlying the gonad primordium |
|
|
What happens to the germ cells if the supporting cells do not invest?
|
Germ cells atrophy
|
|
|
What kind of cells are Leydig cells (M) and Theca cells (F)? Origin?
|
Interstitial cells
- Originate from mesonephric mesenchyme cells |
|
|
What do the gonads attach to?
|
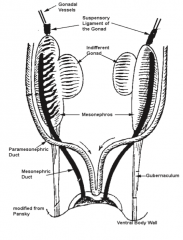
Mesenchymal tissues:
- Cranially (superiorly) - Suspensory Ligament - Caudally (inferiorly) - Gubernaculum (Genito-Inguinal Ligament) - Dorsally (posteriorly) - dorsal mesentery |
|
|
What is the function of the Suspensory Ligament?
|
- Mesenchyme that attaches to the gonad cranially (superiorly)
- Within it, develops the vascular supply to the gonad |
|
|
Where is the vascular supply to the gonad?
|
Within the Suspensory Ligament (mesenchyme that attaches to the cranial aspect of the gonad)
|
|
|
What is the function of the Gubernaculum?
|
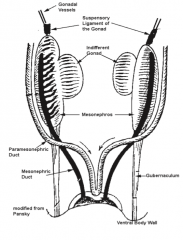
Condensation of mesenchyme that attaches the primitive gonad to the ventral body wall
|
|
|
What are the two genital duct systems that develop during the indifferent stage? When do they form?
|
- Mesonephric Ducts aka Wolffian Ducts - week 4
- Paramesonephric Ducts aka Müllerian Ducts - week 6 |
|
|
Where do the Mesonephric aka Wolffian Ducts form? When do they form?
|
Within the nephrogenic ridges as part of the mesonephros
|
|
|
What signals development of the Paramesonephric aka Müllerian Ducts?
|
Signals from the Mesonephric aka Wolffian ducts
|
|
|
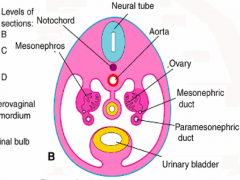
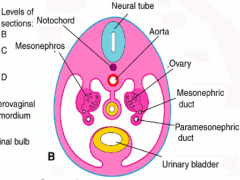
What do the Paramesonephric aka Müllerian Ducts begin as?
|
Each duct begins as an invagination of the coelomic epithelium covering the lateral aspect of the UG ridge
|
|
|
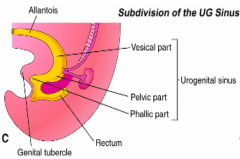
What happens to the Paramesonephric aka Müllerian Ducts initially?
|
- Initially the invagination forms a solid cord of cells that grows inferiorly toward the cloaca but lateral to the mesonephric duct
- As the ducts grow medially toward the cloaca, the ducts lie ventral and superior tot he mesonephric ducts |
|
|
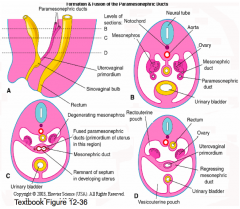
What happens after the Paramesonephric aka Müllerian Ducts grow medially toward the cloaca?
|
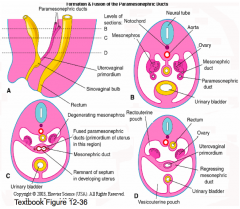
The inferior 1/3 of the paramesonephric ducts fuse together in the midline forming the Uterovaginal Primordium
|
|
|
What forms the Uterovaginal Primordium?
|
The fusion of the inferior 1/3 of the paramesonephric ducts in the midline
|
|
|
What happens after the Uterovaginal Primordium is formed from the inferior 1/3 of the paramesonephric ducts fusing?
|
- The Uterovaginal Primordium contacts the posterior aspect of the cloaca causing a swelling of the back wall in the area of the forming UG sinus (pelvic part)
- This forms the Sinus (Müllerian) Tubercle |
|
|
What do the paramesonephric ducts open into?
|
UG sinus on either side of the Sinus (Müllerian) Tubercle, a lumen forms in the ducts as they develop
|
|
|
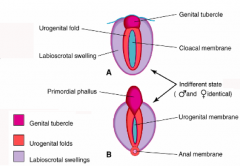
What are the primorida of the external genitalia?
|
- Genital tubercle
- Urethral folds - Labioscrotal swellings |
|
|
What is the appearance of the Genital Tubercle? Origin?
|
- Midline swelling
- Derived from mesenchyme adjacent to phallic part of UG sinus |
|
|
What is the appearance of the Urethral Folds?
|
- Paired swellings surrounding the cloacal membrane
- Initially they are called the cloacal folds |
|
|
What is the appearance of the Labiosacral Swellings?
|
- Paired swellings lateral to the urethral folds
- Little change in their appearance until the fetal period |
|
|
What does a sexually determined but sexually undifferentiated embryo develop during weeks 4-6?
|
- Pair of undifferentiated gonads
- Two sets of ducts - mesonephric and paramesonephric - A set of elevations and folds around the cloacal membrane |
|
|
What gene is responsible for testicular determination?
|
SRY Gene = Sex-determining Region Y
- Found ont he short arm of the Y chromosome - Encodes a DNA binding protein called Testicular Determining Factor |
|
|
When is the SRY gene expressed? Function?
|
During week 6 in males
- Expressed by the supporting cells of the genital ridge - Causes the supporting cells to differentiate into Sertoli cells - Begin to express Sox9 |
|
|
What do Sertoli cells begin to express after differentiating due to the action of SRY?
|
Sertoli Cells express Sox9
|
|
|
What ist he origin of the Sertoli Cells?
|
Coelomic epithelial cords that extend into the mesenchyme of the forming testis
|
|
|
What do the Sertoli Cells do once they have differentiated?
|
- Surround the primordial germ cells inhibiting their progression to meiosis
- Sertoli cells and primordial germ cells organize into Testicular Cords |
|
|
What are Testicular Cords made of? What do they form?
|
- Made of Sertoli Cells and Primordial Germ Cells
- At or before puberty the cords develop a lumen and are known as the Seminiferous Tubules |
|
|
What tissue forms the Seminiferous Tubules? When dot hey form?
|
Testicular Cords = Sertoli Cells and Primordial Germ Cells (without a lumen)
- Once it forms a lumen it is known as the Seminiferous Tubules - Forms at or before puberty |
|
|
What do the Sertoli cells organize into in the area adjacent to he mesonephros?
|
Rete Testis
|
|
|
What do Sertoli cells begin to secrete as they differentiate?
|
MIF: Müllerian Inhibiting Factor
|
|
|
What do signals from Sertoli cells recruit at 8 weeks?
|
Recruit adjacent mesenchyme cells which differentiate into Interstitial / Leydig cells
|
|
|
What is the action of Leydig cells? How is it regulated?
|
- Secrete Testosterone, converting a 21C precursor to a 19C steroid hormone
- This is initially regulated by chorionic gonadotrophin secreted by the trophoblast |
|
|
What happens to the testis as it continues to grow?
|
- Separates from the mesonephros
- Covering coelomic epithelium becomes separated from underlying testicular cords by a condensation of mesenchyme cells that forms a thick CT layer called the Tunica Albuginea |
|
|
What causes the testis to descend into the scrotum?
|
Shortening of the gubernaculum
|
|
|
How often are the testes undescended at birth? What is this called?
|
2-3% of newborns
- Cryptorchidism |
|
|
When does organization of the ovary occur in comparison to when it occurs for a testis?
|
Ovary organization occurs later than for testis
|
|
|
What causes ovaries to develop?
|
Females have no Y chromosome, therefore they do not express the SRY gene
|
|
|
What happens to the Primordial Germ Cells developing in an ovary?
|
Primordial germ cells enter the meiotic prophase and are committed to oogenesis
|
|
|
What do the oocytes produce to stimulate the supporting cells?
|
Oocytes produce FIGα which stimulates the supporting cells to differentiate into Follicle Cells that surround the oocytes
|
|
|
What do the Oocyte and the surrounding Follicle Cells form?
|
Primordial Follicle
|
|
|
What are the components of a Primordial Follicle?
|
- Oocyte
- Follicle Cells |
|
|
What signal arrests oocyte meiosis in meiotic prophase? Source?
|
Meiosis Inhibiting Factor is produced by Follicle Cells
|
|
|
What happens to germ cells that do not have a surrounding of Follicle Cells?
|
Oocytes will atrophy
|
|
|
What prevents mesenchyme cells in females from becoming Leydig cells?
|
Wnt4 signaling
|
|
|
What is required for normal ovarian development?
|
Two X chromosomes
|
|
|
What forms beneath the coelomic epithelium covering the ovary?
|
Thin Tunica Albuginea
|
|
|
Does the ovary change position?
|
Ovaries descend into the pelvis (week 12)
|
|
|
What duct system forms in males? What structures are derived from these ducts?
|
Mesonephric Ducts, forms:
- Duct of Epididymis - Ductus Deferens - Ejaculatory Ducts - Efferent Ductules |
|
|
What structure connects the rete testis with the duct of the epididymis? What is it derived from?
|
Efferent Ductules - derived from the mesonephric duct
|
|
|
Where is T converted to DHT? How?
|
- Converted in the Mesonephric Ducts by 5α-Reductase
- Also in the prostate |
|
|
What does the prostate gland develop from?
|
- Epithelial buds of endoderm from the prostatic urethra (most of the gland tissue is formed from these buds)
- However, some glands surrounding the ejaculatory ducts (central zone) may originate from mesoderm rather than endoderm |
|
|
What do the Seminal Vesicles form from?
|
- Outgrowths of the mesonephric duct just before it enters the forming prostate gland
- Mesenchyme surrounding the glandular buds of the prostate and seminal vesicles form the CT and smooth muscle components in the wall of these glands |
|
|
What happens to the Paramesonephric Ducts in males? How?
|
These are suppressed by MIS (Müllerian Inhibiting Substance) which causes atrophy of these ducts
|
|
|
What is derived from the Paramesonephric Ducts in males?
|
Cranial part of the prostatic utricle
|
|
|
What duct systems develop / regress in females?
|
- Mesonephric Ducts atrophy d/t absence of T
- Paramesonephric Ducts develop d/t lack of MIF (Müllerian Inhibiting Factor) |
|
|
What develops from the Paramesonephric Ducts in females?
|
- Unfused cranial 2/3 become the OVIDUCTS
- Inferior 1/3 fuses with opposite side to become the UTEROVAGINAL PRIMORDIUM (most of which forms the uterus - body and cervix) |
|
|
What does the vagina originate from?
|
- Paramesonephric ducts
- Urogenital sinus |
|
|
What does the Uterovaginal Primordium form?
|
- Most becomes the uterus (body and cervix)
- Contributes to vagina |
|
|
What does the Uterovaginal Primordium connect with inferiorly to finish the vagina?
|
- Inferior tip of the Uterovaginal Primordium contacts the posterior wall of the UG sinus (pelvic part)
- Stimulates formation of a swelling or thickening, the Mullerian or Sinus Tubercle |
|
|
What extends from the Mullerian or Sinus Tubercle (swelling / thickening formed from Uterovaginal Primordium and UG sinus contact)? Effect?
|
Paired, solid outgrowths, Sinovaginal Bulbs, extend dorsally from the Sinus Tubercle pushing the Paramesonephric Ducts superiorly
|
|
|
What happens to the Sinovaginal Bulbs (paired, solid outgrowths of the Sinus Tubercle)?
|
Sinovaginal Bulbs fuse to form a Vaginal Plate that becomes canalized
|
|
|
What is the epithelial lining of the vagina derived from?
|
- Upper part of the vagina is derived from the inferior part of the uterovaginal primordium
- Lower part is formed from the sinovaginal bulbs |
|
|
What forms the remaining tissue of the vaginal wall?
|
Surrounding mesenchyme
|
|
|
What separates the vagina from the UG sinus?
|
A membrane - the Hymen
|
|
|
How common is a complete septum across the vagina? What is this called?
|
3% of the population has a hymen that forms a complete septum across the vagina, known as the Imperforate Hymen
|
|
|
When is an Imperforat Hymen discovered?
|
When the child begins to menstruate during puberty
|
|
|
What are some anomalies of the uterus and vagina?
|
- Absence of uterus and vagina
- Duplication of uterus and vagina - Vaginal Atresia (10% isolated) or with Uterine Aplasia/Atresia (90%) - Complete or incomplete septa may subdivide the uterine lumen |
|
|
What could cause duplication of the uterus or vagina?
|
Incomplete merging of the paramesonephric ducts (which merged to form the unpaired uterovaginal primoridum)
|
|
|
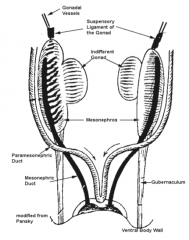
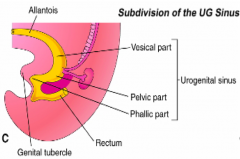
What are the parts of the UG sinus?
|
- Vesicle (superior)
- Pelvic (intermediate) - Phallic (inferior) |
|
|
What does the Pelvic Part of the UG sinus form in males and females?
|
Males:
- Epithelial lining of the distal part of the prostatic urethra and membranous urethra Females: - Epithelial lining of the inferior parts of the vagina |
|
|
What does the Phallic Part of the UG sinus form in males and females?
|
Males:
- Epithelial lining of the penile urethra Females: - Epithelial lining of the vestibule |
|
|
What does the penis form from?
|
- Genital Tubercle elongates during the indifferent stages to become the Phallus
- Urethral Plate (extension of endoderm in the roof of the phallic part of the UG sinus) |
|
|
What happens as the phallus elongates in the male?
|

- Pulls the urethral folds forward causing them to fuse on the ventral surface
- Pulls the UG sinus anteriorly - Deepens the urethral groove on inferior side of the phallus |
|
|
Where do the urethral folds fuse?
|

Urethral folds fuse as the phallus elongates along the ventral surface of the phallus
|
|
|
Where does the penile urethra form?
|

Within the urethral groove (mechanism unclear) and urethral plate contributes to formation too
|
|
|
The development of the male external genitalia and its maintenance is supported by what hormone(s)?
|
Androgen (Dihydrotestosterone)
|
|
|
How does the scrotum form?
|

- Under androgen influence, the perineal area of the male embryo elongates
- Labiosacral swellings fuse ventrally forming the scrotum - Inferior or caudal end of the gubernaculum is attached to the labioscrotal swellings - Testis enters the scrotum via the inguinal canal prior to birth |
|
|
What is the gubernaculum attached to?
|
Labioscrotal swellings (that forms the scrotum)
|
|
|
How do the testis enter the scrotum?
|
Via the inguinal canal prior to birth
|
|
|
What are the penile anomalies? Which is more common?
|
- Hypospadias: urethra opens ventrally
- Epispadias: urethra opens dorsally, 5x more common |
|
|
What is the term for a urethra opening on the ventral surface of the penis? Why does this occur? Other features?
|
Hypospadias
- Occurs because of incomplete fusion of the urethral folds - There may also be a ventral bend in the penis |
|
|
What is the term for a urethra opening on the dorsal surface of the penis? Why does this occur? Other features?
|
Epispadias
- Five times more common than epispadias - Usually associated with bladder exstrophy and rarely occurs as an isolated condition |
|
|
Does the perineal area elongate in males or females? Why?
|
- Males: elongates in presence of androgen
- Females: does not elongate d/t no androgen |
|
|
What happens to the phallus in the female?
|
Bends inferiorly to form the Clitoris
|
|
|
What forms the epithelial lining of the vestibule of the vagina?
|
Phallic portion of the UG sinus
|
|
|
How does the fate of the urethral folds differ in males and females?
|
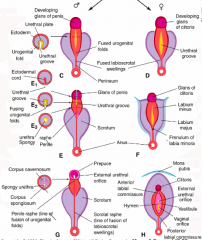
- Males: fuse during elongation of the phallus on the ventral surface
- Females: remain unfused and form the Labia Minora |
|
|
What forms the Labia Minora? Labia Majora?
|

- Labia Minora: unfused urethral folds
- Labia Majora: unfused labioscrotal swellings |
|
|
How does the fate of the labioscrotal swellings differ in males and females?
|
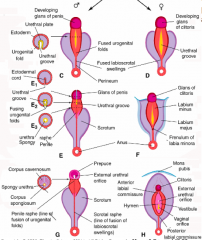
- Males: fuses ventrally to form the scrotum
- Females: remains unfused to form the Labia Majora except for minimal fusion at the anterior end which forms the Mons Pubis |
|
|
What does the Mons Pubis form from?
|
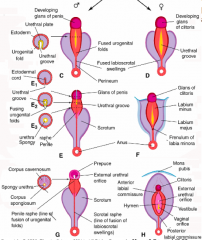
Anterior fusion of the Labioscrotal Swelling
|
|
|
What stimulates development of the female external genitalia?
|
Estrogens
|
|
|
When does sex determination occur?
|
Fertilization
|
|
|
When does sex differentiation occur?
|
During embryonic and fetal periods
|
|
|
What happens during the indifferent stage?
|
Undifferentiated gonads, ducts, and external genitalia form initially
|
|
|
What directs undifferentiated gonads to form testes?
|
SRY gene
|
|
|
What ducts form in males? How?
|
- Mesonephric ducts is supported by androgens from testes and forms the male duct system (except urethra)
- MIS inhibits development of the Pramesonephric ducts |
|
|
What directs undifferentiated gonads to form ovaries?
|
Absence of SRY gene expression
|
|
|
What ducts form in females? How?
|
- Absence of androgens allows Mesonephric Duct to atrophy and allows external genitalia primordia to develop in the female direction (supported by estrogen)
- Absence of MIS allows Paramesonephric Ducts to develop and form the female duct system (except caudal vagina) |

