![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
|
What is the term for the occurrence of tumors involving 2 or more endocrine glands in a single patient?
|
MEN: Multiple Endocrine Neoplasia
|
|
|
What are the two major forms of Multiple Endocrine Neoplasia?
|
- MEN1
- MEN2 |
|
|
What is MEN? Characteristics?
|
Multiple Endocrine Neoplasia
- Occurrence of tumors involving 2 or more endocrine glands in a single patient |
|
|
What are the types of MEN tumors?
|
- Parathyroid Adenomas
- Pheochromocytoma - Enteropancreatic Tumors - Pituitary Adenomas - Medullary Thyroid Cancer - Marfanoid Habitus |
|
|
What type of MEN syndrome has functional, PTH-secreting benign neoplasms arising from normal parathyroid tissue? Signs/Symptoms?
|
Parathyroid Adenomas:
- High serum calcium - Low serum phosphate - Non-suppressed or elevated serum PTH |
|
|
What are the characteristics / location and signs / symptoms of Parathyroid Adenomas?
|
- Functional, PTH-secreting benign neoplasms
- Arises from normal parathyroid tissue - High serum calcium - Low serum phosphate - Non-suppressed or elevated serum PTH - 11q13 mutation (MEN1) in >90%; also associated w/ 12p14 mutation (MEN4) |
|
|
Which type of MEN syndrome is a catecholamine secreting tumor that arises from the chromaffin cells of the adrenal medulla? Signs/Symptoms?
|
Pheochromocytoma
- Hypertension - Headaches - Palpitations - Diaphoresis |
|
|
What are the characteristics / location and signs / symptoms of Pheochromocytoma? Mutations?
|
- Catecholamine secreting tumor
- Arises from the chromaffin cells of the adrenal medulla - Hypertension - Headaches - Palpitations - Diaphoresis Mutations: - MEN2A (10 cen-10q11.2) in 40-50% - MEN2B / MEN3 (10 cen-10q11.2) |
|
|
Which type of MEN syndrome is a neuroendocrine tumor of the intestine and pancreas? Types?
|
Enteropancreatic tumors:
- Gastrinoma - Insulinoma - Glucagonoma - Non-functioning pancreatic tumors |
|
|
What are the characteristics / location and signs / symptoms of Enteropancreatic tumors? Mutations?
|
- Neuroendocrine tumor of the intestine and pancreas
Types: - Gastrinoma - Insulinoma - Glucagonoma - Non-functioning pancreatic tumors Mutations: - MEN1 (11q13) in 30-70% |
|
|
Which type of MEN syndrome is a tumor of the anterior pituitary gland? What can it secrete?
|
Pituitary Adenoma, may secrete any of the following:
- Prolactin - ACTH - GH - LH/FSH - TSH |
|
|
What are the characteristics of a Pituitary Adenoma? What can it secrete? Mutation?
|
- Tumor of the anterior pituitary gland
Can secrete any of the following: - Prolactin - ACTH - GH - LH/FSH - TSH (less common) Mutations: - MEN1 (11q13) in 30-40% - MEN4 (12p14) |
|
|
Which type of MEN syndrome arises from the parafollicular (C) cells and can secrete calcitonin?
|
Medullary Thyroid Cancer
- Can secrete calcitonin |
|
|
What are the characteristics of a Medullary Thyroid Cancer? What can it secrete? How is it inherited? Mutations?
|
- Arises from the parafollicular (C) cells of the thyroid
- Can secrete calcitonin - 75% of cases are sporadic, 25% are familial Mutations: - MEN2A (10 cen-10q11.2) in >90% - MEN2B / MEN3 (10 cen-10q11.2) |
|
|
Which type of MEN syndrome decreases the upper body / lower body ratio, has abnormal posterior position of mandible, decreased cephalic index (head width/length)?
|
Marfanoid Habitus
|
|
|
What are the characteristics of Marfanoid Habitus? Mutations?
|
- Decreases the upper body / lower body ratio
- Abnormal posterior position of mandible - Decreased cephalic index (head width/length) - NO ectopic lentis (displacement or malposition of the eye's crystalline lens from its normal location) or aortic abnormalities Mutations: - MEN2B (MEN3): 10 cen-10q11.2 |
|
|
MEN1:
- Mutation - Types of tumors |
Mutation: 11q13
Types of tumors: - Parathyroid adenoma (>90%) - Pituitary adenoma (30-40%) - Enteropancreatic tumors (30-70%) |
|
|
MEN2A:
- Mutation - Types of tumors |
Mutation: 10 cen-10q11.2
Types of tumors: - Medullary thyroid cancer (>90%) - Pheochromocytoma (40-50%) - Parathyroid Hyperplasia (10-20%) |
|
|
MEN2B:
- Mutation - Types of tumors |
Mutation: 10 cen-10q11.2
Types of tumors: - Medullary thyroid cancer - Pheochromocytoma - Mucosal Neuromas - Marfanoid Habitus |
|
|
Which genetic mutation is associated w/ medullary thyroid cancer only?
|
10 cen-10q11.2
|
|
|
MEN4:
- Mutation - Types of tumors |
Mutation: 12p14
Types of tumors: - Parathyroid Adenoma - Pituitary Adenoma - Reproductive organ tumors |
|
|
What is associated w/ mutation 11q13?
|
MEN1
- Parathyroid adenoma (>90%) - Pituitary adenoma (30-40%) - Enteropancreatic tumors (30-70%) |
|
|
What is associated w/ mutation 10 cen-10q11.2?
|
MEN2A
- Medullary thyroid cancer (>90%) - Pheochromocytoma (40-50%) - Parathyroid Hyperplasia (10-20%) MEN2B / MEN3 - Medullary thyroid cancer - Pheochromocytoma - Mucosal Neuromas - Marfanoid Habitus Medullary Thyroid Cancer only |
|
|
What is associated w/ mutation 12p14?
|
MEN4
- Parathyroid Adenoma - Pituitary Adenoma - Reproductive organ tumors |
|
|
How do you make a CLINICAL diagnosis of MEN1?
|
Patient w/ 2 or more MEN-1 associated tumors
|
|
|
How do you make a FAMILIAL diagnosis of MEN1?
|
Patient w/ 1 MEN1 associated tumor and a 1st degree relative w/ MEN1
|
|
|
How do you make a GENETIC diagnosis of MEN1?
|
Patient with an MEN1 mutation but does not have a clinical or biochemical manifestation of MEN1, mutant carrier
|
|
|
Do all patients diagnosed clinically (2 or more MEN-1 associated tumors) have a germline mutation?
|
No - not all patients with MEN1 will have a defined mutation
|
|
|
What chromosome is mutation in MEN1? Function?
|
- Chromosome 11q13
- Regulated transcription, genome stability, cell division, and proliferation |
|
|
What kind of mutations occur in MEN1?
|
- Inheritance of a germline MEN1 mutation PREDISPOSES a person to develop a tumor that arises after a somatic mutation
- Most MEN1 germline mutations are inactivating - >10% of MEN1 germline mutations arise de novo |
|
|
What tissues are affected by MEN1 tumors?
|
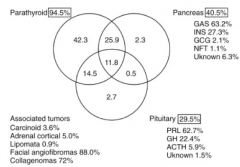
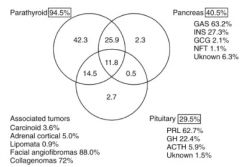
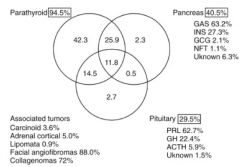
The 3 P's:
- Parathyroid gland (94.5%) - Pancreas (40.5%) - Pituitary gland (29.5%) |
|
|
Which combination of tumors is most common for MEN1 tumors?
|
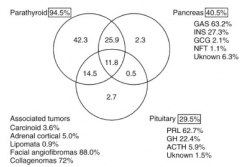
- Parathyroid alone (42%)
- Parathyroid + Pancreas (26%) - Parathyroid + Pituitary (15%) - Parathyroid + Pancreas + Pituitary (12%) - <3%: pancreas only, pituitary only, pancreas + pituitary |
|
|
What is the median age of onset for endocrine tumor expressions in MEN1 (age at 1st symptom or at 1st abnormal test result)?
|
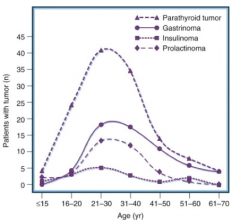
21-30
|
|
|
Who should be offered MEN1 germline mutation testing?
|
- Index patients with MEN1
- First degree relatives of patients w/ MEN1 (including asymptomatic or those w/ clinical manifestations) |
|
|
What should be done if you discover your patient has a germline MEN1 mutation?
|
- Identify family members with the germline mutation to determine appropriate testing for tumor surveillance
- Also want to identify 1st degree relatives that do not have the germline mutation to alleviate them from further testing |
|
|
What should you do for the family of an MEN1 patient that does not have an identified germline mutation?
|
1st degree family members will need to be identified by abnormal chemistries and imaging tests (eg, serum Ca2+ and PTH, gastrin, fasting glucose and insulin, prolactin and IGF-1), and pancreas imaging)
|
|
|
What is the benefit to family members of identifying a germline mutation in your MEN1 patient?
|
It makes it easier to screen first degree family members (check if they have the mutation, if not they are fine); if there is no germline mutation identified in your patient then you must do chemistries and imaging to assess family members
|
|
|
What should you do before offering MEN1 mutation testing?
|
Provide these patients with genetic counseling first
|
|
|
How are MEN1 and MEN2 inherited?
|
Autosomal dominant
|
|
|
What tumors are associated with MEN2?
|
- Medullary Thyroid Carcinoma (MTC)
- Pheochromocytoma - Primary Hyperparathyroidism |
|
|
What mutations are associated with MEN2?
|
Germline mutations in the RET proto-oncogene
- RET = REarranged during Transfection |
|
|
What are the subtypes of MEN2?
|
- MEN2A
- MEN2B - Familial MTC (medullary thyroid carcinoma) |
|

What is this facial appearance indicative of?
|

MEN 2B
|
|

What is this tongue appearance indicative of?
|

Mucosal neuromas on the tongues - MEN2
|
|
|
What is important for determining the appropriate management of a patient with MEN2?
|
- Genotype helps predict phenotype and guides management
- Helps the clinician better understand the risks that the index patient will have for associated diseases such as pheochromocytoma, and will allow for a greater understanding of the management of affected family members such as timing of prophylactic thyroidectomy |
|
Case 1: 48 yo woman being evaluated for hypercalcemia. Hx of kidney stones. Only takes a multivitamin. No weight loss, nausea, pain, or confusion. Her sister's 30yo son has high calcium. Father had hx of severe GERD and died of pancreatic cancer. Paternal uncle had neck surgery twice (maybe for thyroid) and brain surgery. Brother died of MI.
Labs shown above. Why does your patient have hypercalcemia? |
Primary Hyperparathyroidism
|
|
Case 1: 48 yo woman being evaluated for hypercalcemia. Hx of kidney stones. Only takes a multivitamin. No weight loss, nausea, pain, or confusion. Her sister's 30yo son has high calcium. Father had hx of severe GERD and died of pancreatic cancer. Paternal uncle had neck surgery twice (maybe for thyroid) and brain surgery. Brother died of MI.
Labs shown above. Your intern recalls learning about multiple endocrine neoplasia and questions if this patient may have this genetic disease. At present, can you determine if this patient has Multiple Endocrine Neoplasia type 1 (MEN1)? |
Undefined: the patient does not have 2 or more endocrine glands clinically involved and we have not confirmed if her father had MEN1
|
|
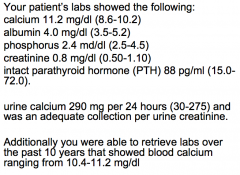
Case 1: 48 yo woman being evaluated for hypercalcemia. Hx of kidney stones. Only takes a multivitamin. No weight loss, nausea, pain, or confusion. Her sister's 30yo son has high calcium. Father had hx of severe GERD and died of pancreatic cancer. Paternal uncle had neck surgery twice (maybe for thyroid) and brain surgery. Brother died of MI.
Labs shown above. The patient, her children, and the patient’s sister and nieces and nephews are concerned about their future risk. What evaluation would your recommend? |
Refer to a genetic counselor prior to testing for MEN1 germline mutation. If patient has a germline mutation, then initially test her children and sister.
|
|
|
Case 2: 25yo man recently diagnosed w/ Medullary Thyroid Cancer. He has 2 children (4 and 6 years). He is positive for germline RET proto-oncogene mutation
1. He questions what should be done at this point in time. Which of the following is NOT a reasonable recommendation? a) Refer to a genetic counselor to review associated risks with germline mutation and testing of his children. b) Order plasma metanephrines to test for pheochomocytoma and serum calcium and intact parathyroid hormone on the patient. c) Recommend that his children have prophylactic thyroidectomy. d) Take a thorough family history so that primary relatives can be tested. |
Children do not need a prophylactic thyroidectomy at this time
|
|
|
What should you consider for a young patient presenting w/ primary parathyroidism?
|
- MEN1 (most will not have MEN1)
- Other endocrinopathies should be considered in the patient (also obtain a detailed family history) |
|
|
What are you obligated to do if you identify a genetic disease in a patient that is likely to affect other family members?
|
Obligated to inform / encourage your patient of the importance of testing other family members
|
|
|
What testing should be done in patients with Medullary Thyroid Cancer?
|
RET proto-oncogene testing
|

