![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
128 Cards in this Set
- Front
- Back
|
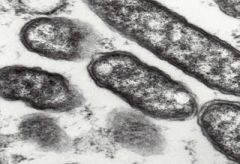
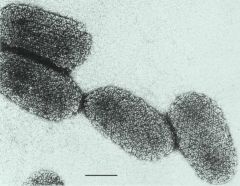
Pathogenesis:
contracted by eating any kind of undercooked food Enetric Fever- -bacteria bury themselves into the lining of the gut and travel on into the lymph, infecting the liver, gallbladder, spleen, kidney, and bone marrow. The bacteria expand in great numbers within all these organs and then pour back into the blood, triggering a raging fever. Gastroentertic- -bacteria stays in the gut causing vomiting, fever, stomach cramps, and diarrhea. Metastatic- -bacteria travel throughout the body, and then set up shop in various locations. these infections can cause damage to heart tissue, joints, and implanted medical devices; they can also leave the person with a form of arthritis. carrier- person shows no symptoms, but instead harbors the bacteria and deposits them daily in his or her stools. Symptoms: -fever (enteric)- infection of liver, gall bladder, kidneys, and bone marrow. stomach cramps, guys deterioration (gastroenteritis)- dehydration, vomiting, diarrhea |
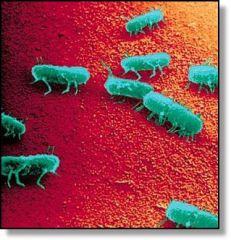
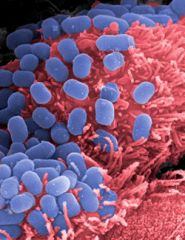
Salmonella enterica
|
|
|
Pathogenesis:
-contaminated food or water -lives in the gut and passed on in their feces Symptoms: -falling temperature and blood pressure -stomach cramps -leg cramps -vomiting, rapid dehydration -organ failure -severe dehydration |

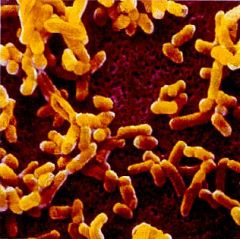
Vibrio Cholerae
|
|
|
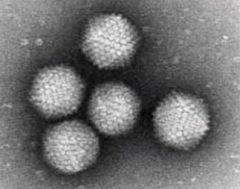
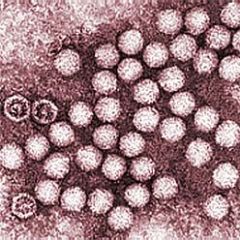
Pathogenesis:
-contaminated food or water -virus absorbed in the gut, and multiplies in lymph nodes in the abdomen -from the lymph nodes, virus migrates in the bloodstream to the central nervous system Symptoms: -Stiff neck, sore throat -Headache, fever -Nausea -Back Pain -Possible muscle paralysis |
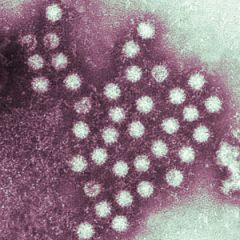
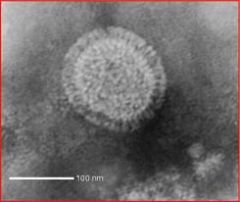
Poliovirus
|
|
|
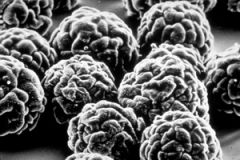
Pathogenesis:
-once the body absorbs the misshapen protein molecule, an unknown process sets about multiplying it Symptoms: -Depression, memory loss, headache -Coordination problem -Mood swings, brain damage -Pains in the limbs -Pins and needles in the arms and legs |
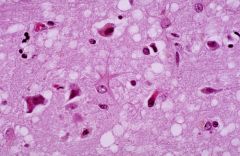
Transmissible Spongiform Encephalopathies
(Proteinaceous infectious particle, prion) |
|
|
Pathogenesis:
-fecal-oral transmission -mostly from contaminated water Symptoms: -fever, exhaustion -yellow eyes -vomiting -nausea -stomach ache, loss of appetite -dark urine |
Hepatitis A virus
|
|
|
Pathogenesis:
-obligate anaerobe -spores get into the food mix before the container is sealed for storage -bacteria releases toxins Symptoms: -dry mouth, difficulty swallowing, vomiting, slurred speech -blurred or double vision -weak neck and arms -diarrhea or constipation -paralysis |

Clostridium botulinum
|
|
|
Pathogenesis:
-often introduced to a person in poorly-cooked ground beef -can also occur after drinking unpasteurized milk or contaminated water Symptoms: -possible fever -kidney failure -damage to gut lining, abdominal cramps -severe diarrhea -red-colored stools |
E. coli 0157:H7
|
|
|
Pathogenesis:
-contaminated water -protozoa disrupts the way in which fats are absorbed in the gut, and it also generates a lot of gas -diarrhea and inability to absorb fat may cause a person to lose weight and become dehydrated, and the symptoms can last for six weeks or longer Symptoms: -Dehydration -Stomach cramps -Diarrhea, greasy stools -Weight loss |

Giardia lamblia
|
|
|
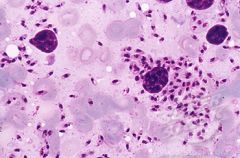
Pathogenesis:
-Infections in pregnant women are rare before about 20 weeks of pregnancy -the only people susceptible are those whose immune system is not working well Symptoms: -Mild chills, fever -Possible headache -Possible eye infection -Possible sore throat -Back pain -Possible diarrhea -Possible miscarriage, premature delivery, or stillbirth |

Listeria monocytogenes
|
|
|
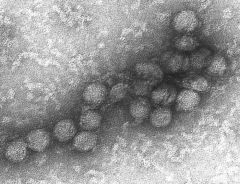
Pathogenesis:
-Passed on in the stools, poor hygiene, or consuming contaminated shellfish -Historic outbreaks found in cruise lines Symptoms: -Vomiting -Nausea -Stomach cramps -Diarrhea |
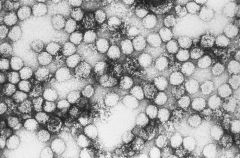
Norwalk Virus
|
|
|
Pathogenesis:
-bacterium carried by fleas -sputum of an infected person is also packed with bacteria Symptoms: -Vomiting blood-pink sputum -Fever headache -Swellings in the neck, armpits, and groin -Nausea |
Yersinia pestis
|
|
|
Pathogenesis:
-spread by Aedes aegypti -virus surrounded by an envelope derived from the host cell membrane, to prevent the host's immune system from recognizing the virus as foreign Symptoms: -red eyes, flushed face -red tongue, vomiting -liver and kidney failure -delirium, seizures, coma, headache, -fever, chills, backache -jaundice |
Yellow Fever
|
|
|
Pathogenesis:
-Lice take in the bacteria from the blood of an infected rat or human, then bites another human, effectively spitting the bacteria into the person's wound -Bacteria enter the body, then spread quickly in the bloodstream -Break into skin cells, multiply and then break out again, destroying the host cell Symptoms: -Headache, Fever, Possible coma -Rash on chest, stomach and back |
Typhus (Rickettsia prowazekii and Rickettsia typhi)
|
|
|
Pathogenesis:
-spread by Sandflies -infects macrophages Symptoms: -Fever -Sores over whole body -Enlarged spleen and liver -Weight loss |
Leishmaniasis
|
|
|
Pathogenesis:
-Drinking water that has been contaminated by animals is the basic route of infection Symptoms: -Fever, Chills -Sore eyes -Nose bleeds -Jaundice -Loss of appetite, Nausea -Bruising -Muscular aches and pains all over body |
Leptospirosa
|
|
|
Pathogenesis:
-tick-borne disease Symptoms: -Erythema migrans "bull's eye" rash -Headache, fatigue -Stiff neck -Loss of concentration, short-term memory loss, chills, fever -Shooting pains -Severe joint pain and swelling, arthritis -Muscular aches and pain -Numbness or tingling in hands and feet |
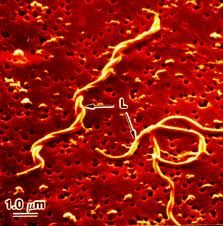
Lyme Disease (Borrelia burgdorferi)
|
|
|
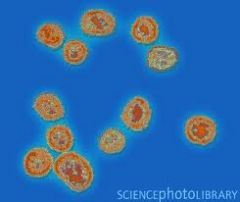
Pathogenesis:
-Aedes mosquito-disease borne -viruses circulate in the blood stream for two to seven days Symptoms: -High temperature -Vomiting -Enlarged liver -Rash all over body -Loss of appetite -Hemorrhagic fever |

Dengue virus
|
|
|
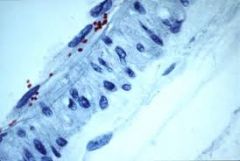
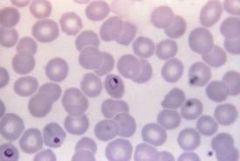
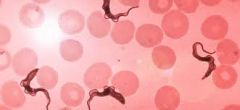
Pathogenesis:
-parasites move from the mosquito's salivary gland into the person's bloodstream -the parasites are then carried to the liver, where they invade cells and produce many copies of themselves -after a couple of days the cells burst, releasing thousands of new parasites into the bloodstream, and triggering a bout of fever Symptoms: -Recurrent Fever, chills -Headache, Fatigue -Possible vomiting -Possible nausea -Possible diarrhea |
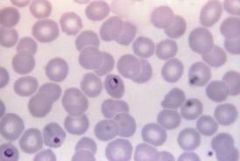
Malaria (plasmodium spp.)
|
|
|
Pathogenesis:
-virus normally enters the body through saliva via a bite injury, and attaches to skeletal muscle cells -multiplies at the wound site, then moves into the nerves -viruses can travel to the spinal cord, and eventually to the brain; from here, they use other nerves to move throughout the body Symptoms: -Feelings of terror -Restlessness, dislike of water -Loss of muscle control -Paralysis |
Rabies (Family: Rhabdoviridae, Lyssavirus)
|
|
|
Pathogenesis:
-mosquito eggs are already infected -once the livestock is infected, any blood-sucking insect can move the virus to other animals or to humans -humans can come into contact with the blood or uncooked meat of infected animals Symptoms: -Dizziness, seizures, mild fever -Weakness -Back pain -Eye damage -Extreme weight loss -Liver problems |
Rift Valley Fever (Family: bunyaviridae)
|
|
|
Pathogenesis:
-the main way this virus gets around is on board birds, who cover large distances on their annual migrations; it then uses mosquitoes to jump to other animals Symptoms: -Headache, mild fever -Vomiting -Possible neck stiffness -Possible: stupor, coma, terrors, disorientation, vision loss, convulsions, brain damage -Possible rash on chest, stomach, and back -Nausea |
West Nile Virus
|
|
|
Pathogenesis:
-the virus lives in animals, but it can jump to humans Symptoms: -high fever, convulsions, drowsiness, disorientation -Inflammation of brain -Muscle Pain |
Nipah Virus
|
|
|
Pathogenesis:
-tick-borne bacteria -grow inside the cells of small and medium-sized blood vessels within its victim -they multiply and destroy the cells, causing the blood vessels to become leaky and leading to the development of black spots all over the person's body Symptoms: -Vomiting -Headache, Fever -Black spots -Nausea -Gangrene -Paralysis |
Rocky Mountain Spotted Fever (Rickettsia rickettsii)
|
|
|
Pathogenesis:
-unknown origin, but speculated in a type of small rodent known as the multimammate rat Symptoms: -Puffy and swollen neck and face -Vomiting -Bleeding gums and nose -Headache, seizures, fever -Deafness -Sore throat, cough -Low blood pressure -Inability to produce urine, diarrhea -Joint pains |
Lassa Virus
|
|
|
First known outbreak of DHF?
|
Manila, Philippines
|
|
|
When and where was Dengue serotype 1 discovered?
|
1978, Cuba
|
|
|
Type of transmission between human mosquito cycle in tropical areas (urban or sylvatic)?
|
Urban
|
|
|
Type of transmission between monkey mosquito cycle in Africa and Asia (urban or sylvatic)?
|
Sylvatic
|
|
|
5 Human host risk factors to severe dengue disease (secondary infection):
|
1. female gender
2. HLA (human leukocyte antigen) class I alleles 3. DC-SIGN (receptor gene variant) 4. SNP of TNF (tumor necrosis factor) gene 5. AB group |
|
|
3 Factors that Reduced Risk for Dengue
|
1. Race
2. Second or third degree malnutrition 3. Polymorphism in Feg and vitamin D receptor genes |
|
|
Dengue, envelope protein sits outside, interacts with _______
|
Dendritic Cells
|
|
|
Progression of Dengue:
Increased vascular permeability, thrombocytopenia, hemorrhagic |
Dengue Hemorrhagic Fever
|
|
|
Progression of Dengue:
Fluid leakage into the interstitial spaces |
Dengue Shock Syndrome
|
|
|
WHO case definition of this disease:
A patient with the following four criteria: 1. acute sudden onset of high fever for 2-7 days 2. hemorrhagic manifestations with at least a positive tourniquet test 3. platelet count < 1 x 10^5/min^3 4. Hemoconcentration or other evidence of plasma leakage |
Dengue
|
|
|
WHO grading of DHF (1997):
-no shock; only positive tourniquet test Management: intravenous fluids temperature control monitor observe stop fluids |
Grade I
|
|
|
WHO grading of DHF (1997):
-no shock; has spontaneous bleeding other than a positive tourniquet test Management: intravenous fluids temperature control monitor observe stop fluids |
Grade II
|
|
|
WHO grading of DHF (1997):
-shock Management: Intravenous fluids Monitor Give oxygen If significant bleeding occurs, give platelets Correct electrolyte and metabolic abnormalities |
Grade III
|
|
|
WHO grading of DHF (1997):
-profound shock with un-measurable blood pressure or/and pulse Management: Intravenous fluids Monitor Give oxygen If significant bleeding occurs, give platelets Correct electrolyte and metabolic abnormalities |
Grade IV
|
|
|
Definition:
Pro-inflammatory cytokines may be primarily responsible for DHF/DSS pathology Secondary infection with a heterotypic strain initiates a mal-adaptive "cytokine tsunami" |
Antibody-Dependent Enhancement (ADE)
|
|
|
Emerging Parasitic Disease:
Transmission: mosquito insect vector 1.5 - 2.7 million deaths per year More than 5000 people die each day, mostly African children below the age of five |
Malaria (plasmodium spp.)
|
|
|
Emerging Parasitic Disease:
Transmission: fecal-oral (oocyst in cat feces) oral (consumption of undercooked meat) Most abundant protozoan parasite in the US; 5-50% of population infected, mostly asymptomatic High risk for immunocompromised individuals Rhoptry organelle contribution to host cell invasion: secretion of protein kinases that down-regulate transcription of IL-12 and modulate the host's immune system |
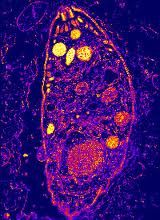
Toxoplasma gondii
|
|
|
Type of Toxoplasmosis:
-tachyzoites transmitted through placenta -infected fetus with severe cerebral complications (hydrocephalus, neonatal encephalitis) |
Congenital Toxoplasmosis
|
|
|
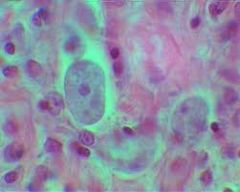
Transmission:
Tsetse fly 50,000 - 70,000 deaths per year Restricted to sub-Saharan Africa where tsetse flies are found as transmission vector West-African form (chronic) East-African form (acute) Early signs: swollen lymph nodes |
Trypanosoma brucei
|
|
|
Transmission:
Reduvid bug (kissing bug) Over 18 million people infected in Latin America Chronic disease, 27% fatal if untreated US: over 100,000 people sero-positive Hearts damaged by chronic myocarditis |

Trypansoma cruzi
|
|
|
Emerging Parasitic Disease:
Transmission: Sandfly Over 200 million people exposed to infection worldwide Chronic disease, visceral form fatal if untreated Incidence of over 500,000 new cases annually |
Leishmania spp.
|
|
|
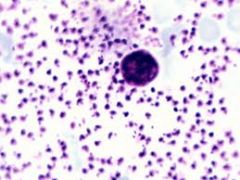
Emerging Parasitic Disease:
Transmission: fecal-oral (contaminated water) Initial symptoms: diarrhea with cramping (blood and mucus in stool) lower abdominal pain low-grade fever |
Entamoeba histolytica
|
|
|
Emerging Parasitic Disease:
Transmission: Fecal-oral (contaminated water) Initial symptoms: profuse watery diarrhea epigastric cramping pain, nausea In AIDS patients: prolonged profuse watery diarrhea |
Cryptosporidium parvum
|
|
|
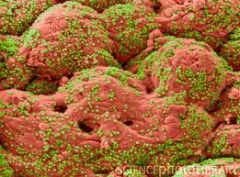
Emerging Parasitic Disease:
Transmission: oral route, consumption of infected undercooked meat, pork, ham from wild boar or other game animals Found worldwide in all climates Adults worms: can cause intestinal inflammation, diarrhea, nausea, high eosinophilia Encysted larvae in muscle: muscle and joint pain, fever, edema of the eyes, hemorrhages under nails (petechia) |
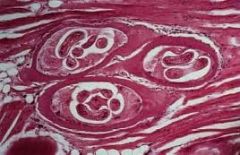
Trichinella spiralis
|
|
|
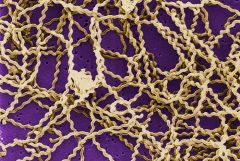
Emerging Parasitic Disease:
Transmission: Mosquito insect vector, transmits infective microfilariae 90 million people infected worldwide, tropical Africa, Asia, America Adult worms in lymphatic channels cause proliferation of the lining of the endothelium, leading to granulation, obstruction and secondary infection of the lymphatic system Late symptoms include lymphangitis, lymphadenopathy, elephantiasis, filarial abscess |

Lymphatic Filariasis (Wucheria bancrofti)
|
|
|
Emerging Parasitic Disease:
Transmission: Blackflies 17 million people infected worldwide; tropical Africa and America Adult worms cause subcutaneous fibrous nodules Microfilarial larvae cause the disease are released into circulation, cause itching, depigmentation of the skin, lymphadenopathy; when invading the eyes they cause inflammatory lesions leading to sclerosing keratitis and blindness |

Onchocerca volvulus
|
|
|
Emerging Parasitic Disease:
Transmission: Infective larvae penetrate the skin 900 million infected worldwide in warm climates Initial symptoms: larvae can cause pneumonitis (larval migration through the lungs) Adult worms in the jejunum ingest blood resulting in occult gastrointestinal bleeding; iron deficiency, anemia |
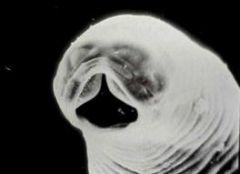
Hookworm (Necator americanus and Ancylostoma duodenale)
|
|
|
Emerging Parasitic Disease:
Transmission: Infective larvae penetrate the skin 70 million people infected worldwide Initial symptoms: larvae can cause pneumonitis (larval migration through the lungs) In AIDS patients: hyperinfection symdrome (massive autoinfection with filariform larvae in the presence of severe immunosupression) |

Strongyloides stercoralis
|
|
|
Emerging Parasitic Disease:
Transmission: Infective larvae penetrate the skin 70 million people infected worldwide Initial symptoms: larvae can cause pneumonitis (larval migration through the lungs) In AIDS patients: hyperinfection syndrome (massive autoinfection with filariform larvae in the presence of severe immunosupression) |

Strongyloides stercoralis
|
|
|
Emerging Parasitic Disease:
Transmission: fecal-oral route: uptake of infective eggs 350 million people infected worldwide; all climates Initial Symptoms: perianal itching (particularly in the morning) Most common parasitic helminth in the US, particularly in children (daycare centers) and nursing homes |

Pinworm (Enterobius vermicularis)
|
|
|
Emerging Parasitic Disease:
Transmission: Oral route: uptake of infective eggs 1.47 billion people infected worldwide in warm climates Initial symptoms: larvae can cause pneumonitis with eosinophilia (larval migration through the lungs) Adult worms can cause obstruction of small intestine, bile ducts and trachea; appendicitis |

Roundworms (Ascaris lumbricoides)
|
|
|
Emerging Parasitic Disease:
Transmission: Fecal-oral route: uptake of infective eggs Oral route: consumption of infected undercooked pork 5 million people infected worldwide Initial symptom: larvae can cause cysticercosis in pork infections (local inflammation, later calification of cysticerci) |

Tapeworm (Taenia spp.)
|
|
|
Emerging Parasitic Disease:
Transmission: Fecal-oral route: uptake of infective eggs Causes hydatid disease |

Tapeworms (Echinococcus granulosus)
|
|
|
Emerging Parasitic Disease:
Transmission: Aquatic snails as intermediate host Infective cercariae larvae penetrate the skin Initial Symptoms: larvae can cause mild dermatitis at penetration site Adult worms: released eggs cause ulceration, inflammatory granuloma and tissue damage; hypertrophy of the bladder or spenomegaly/hepatomegaly, periportal fibrosis involving liver and portal vein |

Schistosoma spp.
|
|
|
Definition:
Any microorganism, infectious substance, or biological product, whether bio-engineered or naturally occurring, capable of causing: death, disease, or biological malfunction in a human, an animal, a plant or any other living organism |
Biological Agent
|
|
|
Earliest record of use of a bioweapon
|
Assyrians poison wells with ergot (fungal toxins)
|
|
|
Who?
White Supremacist 1995, arrested for purchasing yersinia pestis 1998, arrested on charges of developing and stockpiling a biological weapon (anthracis) |
Larry Wayne Harris
|
|
|
-Used to assinate Georgi Markov in 1978
|
Ricin
|
|
|
Type of Biological Weapon Delivery System:
-letter or package -sprayer |
Point Source Delivery
|
|
|
Type of Biological Weapon Delivery System:
-US experiments with Yellow Fever infected mosquitoes -Japanese use of Plague infected fleas in China |
Vectors
|
|
|
Type of Biological Weapon Delivery System:
-Highly modified crop duster or rooftop dispersion -Issues of the inversion and dilution |
Upwind Line Delivery
|
|
|
Type of Biological Weapon Delivery System:
-"person-to-person"- suicidal delivery -only certain agents are transmissible |
Human Carrier
|
|
|
Biological Weapon
Agent Classification: -can be easily disseminated or transmitted person to person -cause high mortality, with potential for major public health impact -might cause public panic and social disruption -require special action for public health preparedness ex. anthrax, plague, tularemia, small pox, hemorrhagic fever viruses |
Category A
|
|
|
Biological Weapon
Agent Classification: -moderately easy to disseminate -cause moderate morbidity and low mortality -require specific enhancements of CDC's diagnostic capacity and enhanced disease surveillance ex. Q fever, glanders, SEB, ricin, salmonella, E. coli, vibrio, cryptosporidum |
Category B
|
|
|
Biological Weapon
Agent Classification: -could be engineered for mass dissemination in the future because of: -availability -ease of production and dissemination -potential for high morbidity and mortality and major health impact ex. nipah virus, hantavirus, encephalitis viruses, yellow fever, MDR-TB |
Category C
|
|
|
Network:
-establish an integrated multilevel laboratory network to provide rapid and critical capacity for response to: 1. bioterrorism 2. emerging infectious diseases 3. other public health threats and emergencies |
The Laboratory Response Network (LRN)
|
|
|
Network:
-since 1995, collaboration of CDC, 10 state health departments, USDA, FSIS, and FDA -active, population-based surveillance for lab confirmed cases of foodborne infections |
FoodNet
|
|
|
An outbreak of _____ was confirmed in Haiti on October 21, 2010
|
Cholera
|
|
|
1862, President Abraham Lincoln signed into law the Agricultural Act that created the ______
|
US Department of Agriculture (USDA)
|
|
|
1906, President Roosevelt signed the _____ and _____ due to the publishing of the "The Jungle"
|
Food and Drug Act, Meat Inspection Act
|
|
|
1938, the _____ was passed after the Elixir of Sulfanilamide Incident
|
Federal Food, Drug and Cosmetic Act
|
|
|
All foreign product and seafood must be identified at point of sale with _____
|
country of origin
|
|
|
Biphasic nature of Bartonella species:
-acute hemolytic anemia |
Oroya Fever
|
|
|
Biphasic nature Bartonella species:
-chronic disease |
Verruga peruana
|
|
|
Disease syndromes caused by B. henselae:
-lymphadenopathy and few other symptoms, found predominantly in immunocompetent individuals |
Cat-scratch Disease
|
|
|
Disease syndromes caused by B. henselae:
-lesions of the skin or internal organs associated with systemic infection organs associated with system infection and characterized by proliferation of the vascular endothelium, found predominately in immunocompromised |
Bacillary Angiomatosis
|
|
|
Definition:
Bartonella -Blood vessel formation from pre-existing vessels and vascular endothelial cells -Physiological- wound healing, tissue regeneration, fetal development, menstruation -Pathogenic- survival mechanism for tumors and tumor-like lesions |
Angiogenesis
|
|
|
4 Factors Contributing to the Increase in TB morbidity:
|
1. Deterioration of the TB public health infrastructure
2. HIV/AIDS epidemic 3. Immigration from countries where TB is common 4. Transmission of TB in congregate settings |
|
|
M. tb spread via airborne particles called _____
|
droplet nuclei
|
|
|
LTBI vs TB:
-usually has a TB skin test of TB blood test reaction indicating TB infection -radiographs is typically normal -sputum smears and cultures are negative -does not require respiratory isolation |
LTBI
|
|
|
LTBI vs TB:
-usually has a TB skin test or TB blood test reaction indicating TB infection -radiographs may be abnormal -sputum smears and cultures may be positive -may require respiratory isolation |
TB
|
|
|
4 Factors Contributing to the Increase in TB morbidity:
|
1. Deterioration of the TB public health infrastructure
2. HIV/AIDS epidemic 3. Immigration from countries where TB is common 4. Transmission of TB in congregate settings |
|
|
What have been the most useful aspects of universal DNA fingerprinting of TBC?
|
1. Detecting false positive cultures
2. Uncovering previously unrecognized cases of transmission 3. Assessing efficacy of TB control programs. |
|
|
M. tb spread via airborne particles called _____
|
droplet nuclei
|
|
|
LTBI vs TB:
-usually has a TB skin test of TB blood test reaction indicating TB infection -radiographs is typically normal -sputum smears and cultures are negative -does not require respiratory isolation |
LTBI
|
|
|
LTBI vs TB:
-usually has a TB skin test or TB blood test reaction indicating TB infection -radiographs may be abnormal -sputum smears and cultures may be positive -may require respiratory isolation |
TB
|
|
|
What have been the most useful aspects of universal DNA fingerprinting of TBC?
|
1. Detecting false positive cultures
2. Uncovering previously unrecognized cases of transmission 3. Assessing efficacy of TB control programs. |
|
|
Laboratory Diagnosis of a Dengue Virus Infection
Confirmed or Probable? Virus Isolation Antigen Detection IgM or IgG seroconversion |
Confirmed Dengue Infection
|
|
|
Laboratory Diagnosis of a Dengue Virus Infection
Confirmed or Probable? IgM positive Elevated IgG titre (that is, 1,280 or greater by hemagluttination inhibition test) |
Probable Dengue Infection
|
|
|
Serological methods to identify and distinguish between Dengue serotypes
|
Direct and Indirect fluorescent antibody tests (DFA, IFA)
|
|
|
Molecular methods to identify and distinguish between Dengue serotypes
|
PCR (serotyping)
Sequencing (genotyping) |
|
|
Types of Weapons of Mass Destruction:
(abbreviations) |
BNICE (Biological, Nuclear, Incendiary, Chemical, Explosive)
CBRNE (Chemical, Biological, Radiological, Nuclear, Explosive) |
|
|
Definition:
Biological agent used as a weapon to injure or destroy humans, animals or plants |
Biological Weapon
|
|
|
Definition:
The use of biological weapons in warfare |
Biological Warfare
|
|
|
Definition:
Deliberate act committed for political, religious, or social objectives Involves use of biological weapon on individual, group, or population |
Bioterrorism
|
|
|
Definition:
Unintentional outbreak Food or drink contamination with microbes and/or toxins |
Natural Outbreaks
|
|
|
History of Biological Weapons:
1000 BC, earliest record of use of a bioweapon. Assyrians poison wells with _____ (fungal toxin). |
Ergot
|
|
|
History of Biological Weapons:
1600, Aztecs conquered by Cortez due to _____ epidemic caused by one of Cortez men. |
Smallpox
|
|
|
History of Biological Weapons:
1763, General Jeffrey Amherst authorizes use of _____ blankets to be given to Delaware Indians at a peace conference. Missouri River tribes decimated. |
Smallpox
|
|
|
History of Biological Weapons:
WWII, General Ishii of Manchurian Unit 731 attacked China with _____ infected fleas. (109 deaths) |
Plague
|
|
|
History of Biological Weapons:
1969, President Nixon _____ |
eliminated offensive bioweapons
|
|
|
History of Biological Weapons:
1979, large scale release of _____ Sverdlovsk, Soviet. |
Anthrax
|
|
|
History of Biological Weapons:
1984, members of a religious group Bhagwan Shree Rajneesh sprayed _____ in salad bars to affect local elections. |
Salmonella
|
|
|
History of Biological Weapons:
1996, lab worker in Dallas infected coworkers with pastries laced wtih _____ |
Shigella
|
|
|
During a bioterrorist event, State and Federal public health laboratories are responsible for _____
|
Rapid, definitive identification
|
|
|
Three reasons why Public Health Laboratory (PHL) is involved in bioterrorist events.
|
1. Mandate by Congress
2. Experience with Biological Agents of Concern and Outbreak Investigation 3. Link between Local Laboratory Level and CDC/Federal agencies |
|
|
Hierarchy of the LRN during a bioterrorist event.
|
Sentinel Labs
Reference Labs National Labs |
|
|
Food Safety:
May, in Miaimi-Dade County, allergic reaction to histamine as well as nausea, dizziness, low blood pressure, diarrhea and headache from consuming _____ |
scromboid blue marlins
|
|
|
Food Safety:
1951-1974, three reported deaths in Florida from tetrodotoxin (TTX) after consuming _____ |
puffer fish (fugu)
|
|
|
Food Safety:
1993, epidemic in the United Kingdom due to feeding scrapie-containing sheep meat and bone meal to cattle which were eaten by humans. |
Bovine Spongiform Encephalopathies
|
|
|
Food Safety:
2002, a multi-state outbreak in the Northeastern US. Majority of cases occurred among pregnant women, elderly, and persons with weakend immune system. Linked to sliceable turkey deli meats. |
Listeria monocytogenes
|
|
|
Food Safety:
November 1, 2002, voluntary recall of 1.5 million cans of powdered infant formula contaminated with _____ |
Cronobacter (Enterobacter) sakazakii
|
|
|
Three Achievements in Public Health (1900-1999) regarding food safety:
|
1. Refrigeration
2. Pasteurization 3. Pesticide Residue Limits |
|
|
This was an FDA food-safety plan for astronauts 30 years ago by Pillsbury
|
Hazard Analysis and Critical Point (HACCP)
|
|
|
National and International network of public health and food regulatory agencies coordinated by the CDC
|
PulseNet
|
|
|
Food Safety:
2006, _____ was found in carrot juice in Georgia and Florida. |
Clostridium botulinum
|
|
|
Food Safety:
2007 to 2008, _____ was found in Chinese milk products. Ended up executing those in charge of the production. |
Melamine
|
|
|
3 Key Elements of Food Defense (all start with a P)
|
Personnel
Product Property |
|
|
_____ integrates the nation's food-testing laboratories at the local, state, and federal levels into a network that is able to respond to emergencies involving biological, chemical, or radiological contamination of food.
|
The Food Emergency Response Network (FERN)
|
|
|
B. bacilliformis, B. henselae, and B. quintana are known to induce _____
|
Angiogenic lesions
|
|
|
Bartonella form in cultures:
Clumps (rough) |
Autoadherent
|
|
|
Bartonella form in cultures:
Single bacteria (smooth) |
Nonadherent
|
|
|
How does Bartonella henselae cause angiogenesis:
-Interactions with _____ to produce pro-angiogenic factors -Interactions with _____ to inhibit apoptosis and to promote proliferation and tubule (capule) formation |
-macrophages
-endothelial cells |
|
|
Zebrafish embryo used as a model for the sudy of Bartonella henselae infection due to the similarities with human _____
|
Immune System
|

