![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
394 Cards in this Set
- Front
- Back
|
What factors predict a difficult ventilation? |
BOOTS |
|
|
1. How is the Mallampati class used in airway assessment? |
1. Class 1 - full view of uvula and posterior pharynx. |
|
|
What factors predict a difficult ventillation? |
BOOTS |
|
|
What factors contribute to a difficult intubation |
MAP |
|
|
What factors must be present for a nasopharyngeal airway insertion? |
Patient must have a gag reflex |
|
|
What is a definitive airway? How can it be placed? |
A cuffed endotracheal tube placed in the trachea. It can be placed by mouth, nasally, cricothyroidotomy or tracheotomy. |
|
|
What advantage does a definitive airway offer? |
It has a cuff, which reduces but doesn't prevent aspiration. |
|
|
Give 5 reasons to obtain a definitive airway. |
Five P's |
|
|
How can increased ICP be managed via intubation? |
Intubation and hyperventillation can decrease ICP temporarily by decreasing CO2 |
|
|
Which drugs can be administered via endotracheal intubation? |
NAVEL |
|
|
What is the ideal way to intubate a patient requiring a cervical collar? |
The cervical collar should be removed and an assistant should stabilize the c-spine. Less movement of spine occurs with this technique. A jaw thrust is then performed and laryngoscope inserted. |
|
|
What is the BURP technique for intubation? |
Backward, rightward, upward pressure on larynx in order to visualize cords. |
|
|
Why should cricoid pressure be applied? |
To prevent aspiration during intubation in patient who is suspected of having a full stomach or with increased abdominal pressure (ascites, pregnant, obese). |
|
|
How should rapid sequence indubation or induction be performed? |
9 P's of RSI |
|
|
Succinylcholine |
1. Suxamethonium chloride (succinylcholine) - depolarizing muscle relaxant. Used for endotracheal intubation. |
|
|
1. What are the adverse effects of succinylcholine? |
Malignant hyperthermia, hyperkalaemia and anaphylaxis, fasciculations. |
|
|
What are the 6 most common life threatening causes of Shortness of Breath that must be ruled out in the ER? |
PE |
|
|
What are the 2 most common causes of bradypnea? |
Opiate intoxication and CNS event. |
|
|
How does pulse oximetry work? |
Measures relative proportion of oxygenated to deoxygenated hemoglobin. This is compared to oxyhemoglobin dissociation curve. |
|
|
What mmHg of blood O2 does a PaO2 of 90% equal? Why relevant? |
1. PaO2 of 90% = 60mmHg of O2. |
|
|
Which states impact on pulse oximetry measurement. |
Anything that decreases capillary blood flow: |
|
|
Name 6 investigations you would consider in a patient with SOB. |
CBC |
|
|
What test can be used to assess pulmonary function in the ER? |
Peak expiratory flow rate. Uses a hand held meter and gives an indication of response to treatment in COPD and Asthma. |
|
|
Define respiratory failure. |
pO2 < 50mmHg. Can be with or without hypercapnia (pCO2 >45mmHg). |
|
|
What information can you garner from an ABG? |
Arterial Oxygenation |
|
|
Define Type 1 respiratory failure. |
Hypoxemia (<50mmHg) without hypercapnia (no pCO2 above 45mmHg). |
|
|
Define Type 2 respiratory failure. |
Hypoxemia (<50mmHg) with hypercapnia (pCO2 >45mmHg). |
|
|
What are the indications for airway protection? |
The 5 Ps. |
|
|
What are the indications for Positive pressure ventilation? |
decreased respiratory effort |
|
|
What FiO2 can you achieve with nasal prongs? |
24-44%. For each L of O2 you get a 4% rise in FiO2. Can't go above 6L without drying out nasal mucosa. |
|
|
What FiO2 can you achieve with a face mask? |
Up to 50-60% at 10 L/min. |
|
|
What is a double flush system? |
Face mask connected to 2 O2 outlets on Max = 30 L/min. Can achieve nearly 100% O2. Useful for CHF pt. who is breathing spontaneously and is responding to diuretics and afterload reducers |
|
|
1. When are bag-mask devices indicated? |
1. An AMBU bag is a temporizing measure until intubation can be achieved. |
|
|
What is CPAP? How can CPAP be used? |
A mask that provides pressure during expiratory phase. Most commonly used in CHF and severe COPD exacerbations. May reduce the need for intubation. |
|
|
Give 5 risk factors for Colon cancer |
Familial adenomatous polyposis |
|
|
What are the most common presenting symptoms of colon cancer? Give 6. |
Abdominal pain — 44 percent |
|
|
What is the most common tumour type in colon cancer? |
The vast majority of colon and rectal cancers are endoluminal adenocarcinomas that arise from the mucosa. Colonoscopy is the single best diagnostic test in symptomatic individuals, since it can localize lesions throughout the large bowel, biopsy mass lesions, detect synchronous neoplasms, and remove polyps |
|
|
Define Syncope |
A transient, self-limited loss of consciousness with loss of postural tone, followed by spontaneous recovery. |
|
|
1. Describe your approach to syncope. |
1. Cardiac (50%) Arrythmia, MI, CHF - sudden, risk factors often present |
|
|
What percent of syncopal episodes have an identified cause? Which causes carry worst prognosis? |
1. 50% of syncopal episodes have a cause. |
|
|
Which risk factors increase likelihood that a syncopal episode is cardiac in origin? |
Male |
|
|
How does the duration of warning period in a syncopal episode help to clarify the etiology? |
The prodromal phase is short when the cause is cardiac, orthostatic and micturational. Other causes such as metabolic, CNS and psychogenic tend to have a long period of feeling uneasy before the syncopal episode. |
|
|
1. What are the 4 major causes of syncope? |
1. Cardiac, CNS, Metabolic & Psychogenic/Vasovagal |
|
|
Describe the 5 high risk factors for a syncopal episode described in the San Francisco Syncope Rule. |
1. Hx of CHF |
|
|
Name 3 causes of sudden death in athletes. |
1. Hypertrophic cardiomyopathy |
|
|
Who should be considered for admission with a syncopal episode? |
1. Older males |
|
|
How do you stratify risk of rabies with a dog bite? How do you treat each? |
1. Vacinnated dog - Td only |
|
|
Why don't you vaccinate all patients with a dog bite? |
1. Expensive and short shelf life. |
|
|
1. What are the 3 most common organisms found in dog bites? |
1. Pasteurella species, staphylococci, streptococci, and anaerobic bacteria. |
|
|
How should animal bites be treated? |
Generally: |
|
|
What antibiotics can be prescribed for animal bites? |
1. Antibiotic choices include: Amox-clav 875/125 bid, cefuroxime 500mg bid or TMP-SMX 1DS bid, |
|
|
1. What organisms can infect a cat scratch or bite? |
Pasteurella species, staphylococci, streptococci, and anaerobic bacteria. Capnocytophaga canimorsus, a fastidious gram-negative rod, can cause bacteremia and fatal sepsis after animal bites, especially in asplenic patients or those with underlying hepatic disease. |
|
|
Clonidine: |
1. Clonidine is an α2 adrenergic agonist. It has specificity towards the presynaptic α2 receptors in the vasomotor center in the brainstem. This binding decreases presynaptic calcium levels, and inhibits the release of norepinephrine (NE). The net effect is a decrease in sympathetic tone.[3] |
|
|
Corticosteroid side effects |
Mania |
|
|
Digoxin: |
digoxin, a product of the foxglove plant. |
|
|
Side effects of Digoxin |
Disturbances of color vision with a tendency to yellow-green coloring. |
|
|
Cardiac side effects of digoxin overdose (5). |
1. any dysrhythmia. |
|
|
Side effects of Fluoroquinolones. |
Cartillage damage in children - not used in children. |
|
|
Mechanism of action of fluoroquinolones. |
They are bacteriacidal. |
|
|
Furosemide |
1. Loop diuretic. The name of Lasix is derived from lasts six. |
|
|
Contraindications to Fluorquinolones. |
Epilepsy |
|
|
Fibrates: |
1. Although less effective in lowering LDL, fibrates improve HDL and triglyceride levels by increasing HDL levels and decreasing triglyceride levels, and seem to improve insulin resistance when the dyslipidemia is associated with other features of the metabolic syndrome (hypertension and diabetes mellitus type 2). They are therefore used in many hyperlipidemias. |
|
|
Fibrates |
Agonists of the PPAR-α (Peroxisome proliferator-activated receptor alpha) receptor in muscle, liver, and other tissues. Activation of PPAR-α signaling results in: |
|
|
Side effects of fibrates. |
Myositis |
|
|
Halothane |
1. Inhaled general anaesthetic |
|
|
HCTZ - Hydrochlorothiazide |
1. Hypertension and edema |
|
|
Hydralazine |
1. Interferes with the second mesenger IP3 to inhibit Ca++ release from sarcoplasmic reticulum in smooth muscle cells. This causes relaxation of smooth muscle cells and decreased peripheral resistance, lowering BP. |
|
|
Hydralazine |
1. Common side-effects include: |
|
|
Isoniazid |
A prodrug must be activated by bacterial catalase. Blocks fatty acid synthase. This process inhibits the synthesis of mycolic acid required for the mycobacterial cell wall. |
|
|
Isoniazid |
Rash |
|
|
MAOI toxicity |
Hypertensive tyramine reaction |
|
|
6 clinical features of methanol ingestion |
Visual disturbances |
|
|
How does methanol become toxic with ingestion? |
Metabolized to Formaldehyde in a process initiated by the enzyme alcohol dehydrogenase in the liver. |
|
|
How is methanol ingestion treated? |
Ethanol or fomepizole. |
|
|
Define shock. |
An abnormality in the circulatory system resulting in underperfusion of the tissues. If not corrected results in cell death and organ failure. |
|
|
Which systems can be at the root of shock? |
1. Pump - Roght or Left heart pathology |
|
|
Give 6 clinical signs of shock. |
1. CNS - Agitation followed by obtundation. |
|
|
In shock palpating the pulses can give you an estimation of blood pressure. Describe how you can estimate systolic BP from the pulses. |
Radial = >80 |
|
|
What is a normal cap refill? |
<2 seconds |
|
|
1. Describe how you estimate the degree of blood loss in shock. |
1. Class 1 - <750cc, Pulse <100, Normal BP, cap refill, resp, urine output. Anxious. Give 3 x 750cc NS. |
|
|
How much fluids should you replace in shock? |
3:1 rule. Warmed Crystalloids are the fluid of choice. Blood should be added in Class 3 and 4 shock. |
|
|
When should you add packed RBCs in shock? |
In class 3 or 4 shock or when patient fails to respond to 2-3L of fluid. |
|
|
Give 6 treatments for anaphylactic shock. |
IV crystalloid NS 1-2L (20cc/kg for children) |
|
|
Name the 3 most common allergens causing anaphylactic shock. |
1. Peanuts and Tree Nuts - 50% |
|
|
Give 4 treatments for cardiogenic shock. |
1.IV crystalloid NS |
|
|
How should tension pneumothorax be managed? |
Needle thoracostomy followed by chest tube insertion. |
|
|
Give 6 treatments for septic shock. |
1. Control airway and breathing. |
|
|
Give 5 possible causes of Vertigo in a 40 year old male. |
90% are vestibular |
|
|
1. You suspect a patient you’ve just seen in ER may have cancer but you’re not sure. You’re referring the patient for an out-patient consultation. You should tell the patient: |
c) Something general and then answer any patient questions honestly. |
|
|
1. An oxygen saturation of 90% approximately corresponds to an arterial pO2 of: |
c) 60 mmHg |
|
|
1. A 72 y/o man with no previous history of headaches presents complaining of headaches worsening over the past 2-3 weeks. All of the following are suggestive of raised intracranial pressure headache secondary to tumour, EXCEPT: |
c) better in early AM |
|
|
1. Symptoms of lower airway obstruction include: |
d) wheezing |
|
|
ABG |
1. PaO2 80-100, PaCO2 36-44, pH 7.35-7.45, HCO3 24. |
|
|
1. Which statement is FALSE: |
d) a parent who first suffered angina at the age of 70 is an important risk factor for a 45 y/o patient with chest pain * |
|
|
1. A bHCG test is indicated in all women of child bearing age who present with abdominal pain EXCEPT when they: |
e) have had a hysterectomy |
|
|
1. In most patients with acute asthma, the best way to assess severity of airflow obstruction is: |
c) measurement of PEFR (Peak Expiratory Flow Rate) or FEV1 and best measurement of oxygenation is an ABG. |
|
|
1. In patients with acute severe pulmonary edema not responding to first-line medications, what alternative therapy is NOT indicated? |
d) blood transfusion * |
|
|
10 first-line treatments of pulmonary edema secondary to CHF exacerbation |
ABCs & LMNOP |
|
|
What are the x-ray signs of CHF? |
Cardiomegaly |
|
|
What is the role of Brain Natriurectic peptide in CHF? |
Elevated in CHF. Useful for diagnosis and prognosis when the clinical and other investigations are not definitive for CHF. |
|
|
What is Cushing's Response? |
1. hypertension, bradycardia, and respiratory depression. Occurs when brainstem, perfusion is compromised by increased ICP. |
|
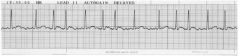
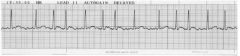
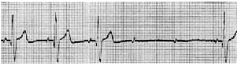
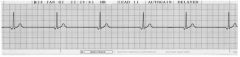
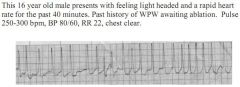
X. Identify his rhythm. (1 mark) |
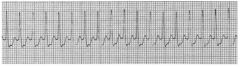
X. * PSVT - Paroxysmal supraventricular tachycardia |
|
60 year old woman on coumadin for a known irregular heart beat. Asymptomatic, P 70. BP 120/75. Has not taken her metoprolol for 2 days. Came to ED because of sprained ankle. |
1. Stable Chronic atrial fibrillation.. |
|
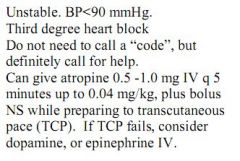
75 year old male presenting with 15 second syncopal episode. Chest pain, diaphoretic, lightheaded, nauseated, BP 100/60mmHg, chest clear, known coronary artery disease. |
1. Mobitz Type 2. |
|
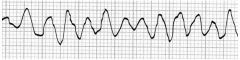
Patient is pulseless and apneic. |
1. V Fib |
|
1. Are the P’s related to the QRS, (i.e. are they conducted)? |
In the first strip there are P waves seen before |
|
|
A 41 y/o male alcoholic is brought into the ED by ambulance. He has been seizing for approximately 20 minutes. Appropriate actions in the next 5 minutes may include all of the following EXCEPT: |
d) ordering a stat EEG * |
|
What is this rhythm? |
Agonal rhythm |
|
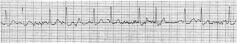
1. What is the rhythm? |
1. Wide complex tachycardia, regular, no P’s seen. |
|
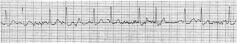
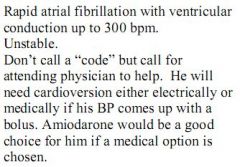
1. Describe what you see here. |
Narrow complex, fast (up to 300 bpm in certain parts of strip), irregularly, irregular, unable to see P waves. Most consistent with rapid atrial fibrillation. At rapid rates can be difficult to discern from PSVT, look for |
|
15 year old boy comes to ED complaining of palpitations for 1 hour. He has had |
1. Wide complex tachycardia. VT until proven otherwise. Stable. Urgent - even though a patient is stable, an arrhythmia that is potentially unstable should be assessed within minutes. |
|
|
HOCM or HCM |
1. Hypertrophic (obstructive) cardiomyopathy. Hypertrophy can occur in any region of the left ventricle but frequently involves the interventricular septum, which results in an obstruction of flow through the left ventricular (LV) outflow tract. |
|
|
Which of the following statements about insect stings is NOT true? |
c) FALSE. Immunotherapy can reduce recurrence in insect stings by 97%! |
|
|
1. What is the ER mgt. of Anaphylaxis? |
1. IV Fluids 1-2L NS IV (20cc/kg for children), O2 100% non-rebreather, Inhaled salbutamol, epinephrine 0.3-0.5mg IM q3-5min, Ranitidine 1mg/kg IV, Diphenhydramine 1mg/kg IV, |
|
|
Medical testing after sexual assault frequently includes all EXCEPT: |
d) testing for hepatitis B serology |
|
|
The INCORRECT statement below with regard to rabies: |
a) local wound care has no effect on diminishing the risk rabies transmission * |
|
|
How should a wound from an animal suspected of having rabies be managed? |
a) local wound care diminishes the risk rabies transmission - +++ irrigation |
|
|
A 6 mo. old boy is brought to the hospital because of a 3-day history of profuse vomiting and diarrhea. He weighs 5 kg. He has been unable to tolerate any fluid. Mother is unsure of the last urine output because of the diarrhea. On initial exam, he is lethargic, mottled and has a capillary refill of 3-4 seconds. Vital signs are BP 90/p, HR 180, RR 40. Initial fluid resuscitation of this infant should be: |
e) 100cc 0.9% NaCl = 20cc/kg |
|
|
Shock in children |
1. signs of shock - mottled skin, cool extremities, diminished pulses, delayed cap refill, MS changes, oliguria and tachycardia. |
|
|
Cardiac arrest in children |
1. Airway and fluids are critical - Resp failure and hypovolemia are most common cause in children. |
|
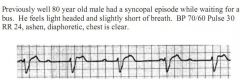
75 year old male in ER for syncope. He vomits as the nurse is starting an IV and |
1. Third degree Heart block |
|
|
A 24 mo. old child is brought to the ED with a temperature of 39C rectally. Parents state she has had the fever for 5 days now and feel she is less active than normal. On exam the child is quiet and cooperative and no focus of infection is found. You decide to do the following investigations: |
d) none as the child does not appear lethargic or toxic |
|
|
Rochester Criteria |
1. Infants <60 days who appear well (non-toxic) with a fever. |
|
|
How should the following febrile children be approached: |
a. <30d - all febrile infants under 30 days get full septic w/u + Amp + cefotaxime or Amp + gent. |
|
|
1. What % of otitis media infections are viral? |
1. Up to 80% of otitis media infections are viral - hence no role for Abx. |
|
|
How should Otitis Media be managed in: |
(i) <6 mths - Antibacterial therapy x 10d |
|
|
Streptococcal Pharyngitis |
Streptococcal Pharyngitis |
|
|
Uncomplicated UTI |
Uncomplicated UTI |
|
|
Describe the Tx of an asthma exacerbation in the ER. Give 8 steps. |
1. O2 if sat <90% |
|
|
Asthma exacerbation discharge |
1. Ventolin/Salbutamol by MDI with spacer - 4 puffs q4h x 24h, then 2 puffs qid x 1wk. |
|
|
Bronchiolitis |
1. First episode of wheezing with cough in a child under 2. |
|
|
Croup - Laryngotracheobronchitis |
1. viral infection of the upper trachea and larynx |
|
|
An 8 y/o girl with a history of a viral-like illness 2 weeks ago and a 1 week history of difficulty passing hard, infrequent stools. Her appetite is not as good as usual according her father. Investigations for this condition include: |
b) urinalysis - she is dehydrated |
|
|
A 10 y/o boy presents to the ED after twisting his ankle while playing soccer. He is unable to weight bear and is complaining of pain over the lateral of his ankle. On examination he has tenderness and swelling over the lateral malleolus. X-ray of his ankle does shows no evidence of fracture. Optimal treatment for this child includes: |
c) immobilize the leg in a cast, crutches - see Ottawa ankle rules |
|
|
Ottawa Ankle Rules |
Ottawa rules only apply to patients older than 16 and under 65. |
|
|
10. A patient intoxicated with OTC diet pills complains of palpitations and chest pain. Physical examination reveals that the patient is tachycardic at 150 with a blood pressure of 180/110. Which on of the following substances would present with the same toxidrome? |
ANSWER = Theophylline is a sympathomimetic. Hypertension, tachycardia, mydriasis, diaphoresis, sweats, seizures. |
|
|
1. Describe a sympathomimetic toxidrome. |
1. sympathomimetic. Hypertension, tachycardia, mydriasis, diaphoresis (sweating), seizures. |
|
|
Cholinergic Toxidrome |
1. Due to inactivation of acetylcholinesterase - salivation, lacrimation, incontinence, diarrhea, bronchospasm, bronchorrea, bradycardia, vomiting |
|
|
An 18 y/o female is brought from a house party, agitated and combative. Which feature of her physical examination would reveal whether her presentation was secondary to diphenhydramine versus “Ecstasy” (a designer amphetamine)? |
e) presence/absence of diaphoresis * |
|
|
What is diaphoresis? |
excessive sweating. |
|
|
A 48 y/o man who is known to drink large amounts of alcohol on a daily basis presents to the ED with severe abdominal pain of 3 hours duration. A reasonable differential diagnosis for the cause of this man’s pain includes all of the following, EXCEPT: |
a) bleeding esophageal varices are generally painless and will present with weakness, shock, vomiting, anemia. |
|
|
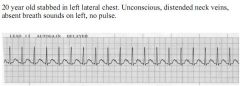
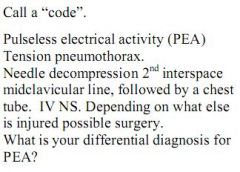
A 40 y/o man presents after a stab wound to the left chest, complaining vigorously of shortness of breath. On examination, he is pale, diaphoretic, and has a blood pressure of 60/40. Your clinical evaluation determines the presence of a left sided tension pneumothorax. Your initial management in this patient involves which one of the following: |
c) insertion of a needle in the left second interspace, midclavicular line followed by insertion of a chest tube. |
|
|
The most important historical feature to ascertain in the assessment of head trauma is: |
c) loss of consciousness * |
|
|
Canadian CT Head Rule |
CT Head Rule is only required for patients with minor head injuries with any one of the following: |
|
|
Jones Fracture |

1. Ankle roll-over is most common cause. |
|

1. What kind of fracture is this? |
1. An avulsion fracture of the base of the 5th metatarsal (pseudo-jones) |
|
|
What is the most common reason that a fracture would threaten life immediately? |
1. Blood loss |
|
|
How much blood can be lost with the following fractures: |
1. 3 L |
|
|
What are the 5 P's of compartment syndrome? |
Pain |
|
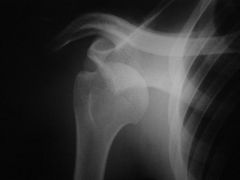
1. What injury is this? |
1. Anterior shoulder dislocation. >95% of dislocations are anterior |
|
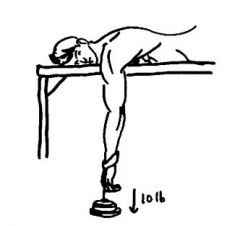
1. Name 2 methods to reduce a shoulder dislocation. |
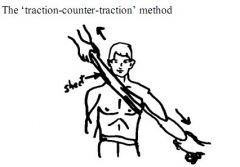
1. Traction-counter-traction method & Stimson method. |
|
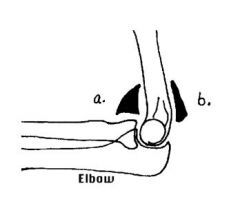
Lateral Elbow X-Ray |
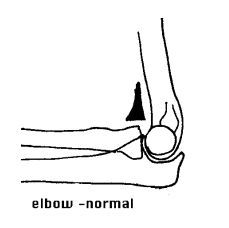
1. These are signs of an elbow effusion - a pronounced anterior is abnormal. ANy fluid collected in the posterior fat pad is abnormal. |
|
|
Calcaneal Fracture |
1. Jumping from a height or vehicle crash. |
|
|
Some wounds require oral antibiotics routinely. Which of the following wounds necessitate the use of antibiotics? |
c) cat bites are almost always puncture wounds and are considered high risk. |
|
|
Give 1st, 2nd and 3rd line antibiotic choices for mammalian bite wounds. |
1st line = Amox-clav. |
|
|
Name 5 wound factors and 3 patient factors that make a wound high risk and thus require antibiotic prophylaxis. |
1. Puncture (cat bite), crush injury, older than 12 hours, hand and foot wounds, near a joint. |
|
|
Name 5 wounds that are tetanus prone. |
Deep (>1cm), >6h old, crush, contaminated, bite |
|
|
1. Who should get Td with a wound? |
1. No booster within the last 5 years. |
|
|
1. What is the most common method of transmission of rabies to humans in North America? |
Bat bites - about 80% |
|
|
Animal bite - Suspect Rabies |
1. Contact public health |
|
|
Can Rabies Immune Globulin and Vaccine (HDCV) be used in pregnancy? |
YES! |
|
|
When should you initiate rabies prophylaxis in relation to a bat? |
1. Confirmed bite |
|
|
How should a fight bite be managed? |
1. High risk for septic arthritis and osteomyelitis. |
|
|
Which of the following is NOT a common cause of CHF? |
c) Mitral stenosis * |
|
|
Name 6 common causes of CHF |
CAD, HTN, Valvular heart disease (not mitral stenosis), cardiomyopathies, pericardial disease, metabolic disorders (TSH), viral myocarditis, toxins |
|
|
Name 6 common causes of CHF exacerbation. |
1. Cardiac - MI, Ischemia |
|
|
1. What is the difference between systolic and diastolic CHF? |
Systolic - dilated left ventricle with impaired contractility and decreased cardiac output. |
|
|
Name 2 causes of posterior shoulder dislocation. |
Rare - <5% of dislocations. Most common causes are electrocution and epilepsy. |
|
|
What % of adults will have an acute back pain episode? |
90% lifetime incidence |
|
|
What is the most common cause of back pain? |
Lumbosacral strain and Sciatica |
|
|
What are the 2 classes of SERIOUS non-traumatic back pain. |
1. SPINAL - cauda equina syndrome, spinal compression, epidural abcess, epidural hematoma, central disc herniation and osteomyelitis. |
|
|
Name 8 RED FLAGS for back pain. |
1. Fever - infxn & cancer |
|
|
Name 4 symptoms that indicate back pain is more likely of a benign etiology. |
1. Worse with flexion |
|
|
Spinal Epidural Abcess |
1. An expanding suppurative infection in the spinal epidural space impinges on the spinal cord, producing sensory symptoms and signs, motor dysfunction, and, ultimately, paralysis and death |
|
|
Cauda Equina Syndrome |
1. Compression of the spinal nerve roots of the cauda equina which begins at L1-2. It is a SURGICAL EMERGENCY. |
|
|
3 most common causes of surgical abdomen in the elderly. |
1. Cholecystitis |
|
|
1. Which ECG lead is best used to look at P waves? |
1. Lead 2 |
|
|
Describe your approach to ECGs in the ER. (5) |
1. QRS - wide vs. narrow |
|
|
Give 5 possible Dx of a wide QRS complex tachyarrythmia. |
1. VT |
|
|
Give 4 DDx of a Narrow QRS bradyarrythmia. |
1. Sinus bradycardia |
|
|
Give 6 DDx of a Narrow complex QRS tachyarrythmia. |
1. A Fib - Irreg, no P |
|
|
How are A Fib and Multifocal Atrial Tachycardia similar and different? |
Similar - Irregular, Narrow QRS, Tachycardia |
|
|
Narrow complex QRS, Irregular, Rate 150, no P waves. Dx? |
Atrial Fibrillation |
|
|
Multifocal Atrial Tachycardia |
1. Multple foci within the atria usually seen in severe hypoxia, theophylline overdose, hypoxia and most commonly in COPD exacerbation. |
|
|
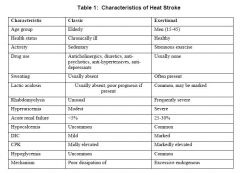
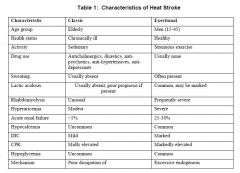
Which of the following is NOT a presentation of heat stroke? |
c) onset is gradual rather than sudden |
|
|
Pt. presents with decreased level of consciousness. On exam he has pinpoint pupils and is unresponsive. Which of the following is NOT a likely etiology? |
b) TCA overdose |
|
|
A 3 wk-old child presents to ED with unwell and decreased activity. He has episodes of bradycardia and apnea. On exam his RR is 20, HR 100, BP 60/?. He does have episodes of apnea but responds readily when stimulated. What would you do in the NEXT step of management? |
d) apply pulse oxymeter, if below 92% place oral airway and give 100% O2 |
|
|
A 8y/o child has a Hx of Henoch-Schoenlein purpura (HSP) and presents with episodes of colicky and crampy abdominal pain. Which of the following must be ruled out? |
c) intussusseption - |
|
|
Henoch-Schoenlein Purpura (HSP) |
1. IgA mediated - likely an anaphylactoid |
|
|
What is the TRIAD of Henoch-Schoenlein Purpura (HSP) |
puritic rash on lower extremities, abdominal pain and arthralgias. 50% of cases also have hematuria and cellular casts. |
|
|
A 10y/o boy fell and presented to another ED with a fractured wrist on X-Ray and was casted. He has been complaining of persistent pain overnight and on exam you notice his digits are swollen and slightly bluish in colour. He has good flexion but limited extension. What is you next step in management? |
c) remove cast and examine the hand - rule out compartment syndrome before calling pediatric ortho. |
|
|
Vagal Manoevres |
1. Carotid Sinus massage - apply pressure/massage the carotid at the angle of the jaw. Causes Vagal stimulation, decreasing heart rate and BP. Must rule out carotid bruit first. Used for A Fib, A Flutter, SVT (first line). |
|
|
Give 3 treatments for SVT |
1. Vagal manoevre (carotid massage), Adenosine 6mg, Adenosine 12mg, then Synchronized cardioversion if no response. |
|
|
Ventricular Tachycardia (VT) |
1. Wide QRS, no P, tachy, usually regular. |
|
|
Name the contributing factors to VF/VT and Pulseless arrest that must be searched for during a code. |
6 H's and 5 T's |
|
|
Wolff-Parkinson-White |
1. Alternative conduction pathway that bypasses the AV node, resulting in early depolarization of the ventricle and a characteristic Delta wave. |
|
|
Atrial Flutter |
1. Narrow QRS, often regular, QRS rate around 150, P waves present and around 300, usually with a 2:1 or 3:1 block |
|
|
Heart Block Properties and Tx |
1. N = 0.12-0.2s |
|
|
Management of UNSTABLE 3rd Degree Heart Block |
1. Stop all Beta-blockers, CCB |
|
|
1. What is a common cause of Heart Block? |
1. Inferior MI |
|
|
Adenosine |
1. Blocks AV node for 10-15s - loss of pulse/asystole by reducing cAMP and hyperpolarizing AV node cells. |
|
|
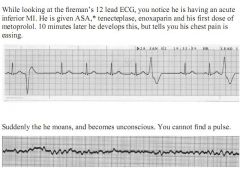
1. What is the most common Post-MI thrombolysis Arrythmia with tKA? |
1. Junctional Bradycardia |
|
|
Which of the following is NOT a risk factor for developing frostbite? |
b) alcohol ingestion * |
|
|
Which of the following is NOT part of the skill set of a primary care paramedic? |
b) synchronous cardioversion |
|
|
Which of the following demographic groups pose the highest incidence of drowning? |
b) toddlers and teens |
|
|
Which of the following is TRUE for a bite wound? |
d) b) & c) |
|
|
The responsibilities of a Base Hospital Physician include: (select 3) |
b) responsibility for an Delegated Medical Act performed by the Emergency Medical Attendant * |
|
|
Rapid neurologic evaluation of a comatose patient includes: (select 4) |
a) otoscopic exam of tympanic membrane * |
|
|
Which are NOT features of exertional heat stroke? (select 2) |
c) rhabdomyolysis usually absent * |
|
|
A 45 y/o female is brought to the ED from an apartment fire. Select 4 clinical signs or symptoms consistent with CO poisoning. |
c) headache * |
|
|
What is the first thing you should do if you get an abnornally high potassium result on a pt.? |
Check the sample - was the sample hemolyzed. Redo the sample STAT! |
|
|
Name 4 common causes of Hyperkalemia in the ER |
1. Hemolysis - an artifact |
|
|
Hyperkalemia. |
1. Weakness, cramps, focal neuro deficits. |
|
|
What common electrolyte and lab abnormalities are seen in pts. with renal failure? |
Azotemia = Accumulation of waste products. |
|
|
Hyperkalemia |
a. Heart - Calcium chloride 1 amp |
|
|
1. What percent of MI patients die before reaching the ER? |
1. 40% |
|
|
What impact does thrombolytic therapy have on mortality? |
Decreases mortality by 25-50% |
|
|
1. Name 8 symptoms of an MI. |
1. Retrosternal chest pain, diaphoresis, pain radiating to left or right arm, jaw pain, SOB, syncope, N + V |
|
|
Which features of MI are more common in elderly? |
Dyspnea, Stroke, Syncope, Delerium, Weakness. |
|
|
Name 5 alternate diagnoses that must be ruled out when considering an MI. |
1. Aortic dissection - ripping/tearing to back |
|
|
Name 5 risk factors for MI. |
1. Previous MI |
|
|
Name 7 PE features of an MI |
1. Decreased BP |
|
|
Killip Class |
1. A classification of hemodynamic status. |
|
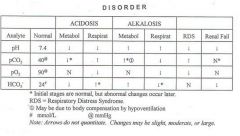
Cover over the boxes and complete the following table regarding acid-base disorders and ABG interpretation. |
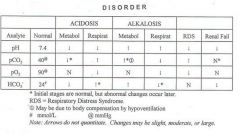
ABG Interpretation |
|
|
1. What ECG changes would prompt you to order a 15 lead ECG? |
1. 15 lead will give you a picture of the Right Ventricle. It should be done on all patients with an inferior wall MI (ST elevation in II, III and AVF). |
|
|
1. Where is an INFERIOR WALL MI seen on ECG? |
1. ST elevation seen in II, III and AVF |
|
|
Name 5 changes seen on ECG with an MI |
1. Increased voltage in R waves in precordial leads |
|
|
What ECG ST segment changes will be reflected in: |
a. II, III, aVF |
|
|
How long does it take for Troponin levels to rise? |
levels rise after 2-6 hours after onset of symptoms. Should do serial enzymes for 6-9 hours after presentation. |
|
|
Name 6 complications of an MI |
1. Arrythmia - most common cause of death |
|
|
Name 4 key MEDICATION treatment priorities and their order in managing an MI |
1. ASA - 2-4 baby, chewed |
|
|
describe your management of a patient presenting with a suspected MI. |
1. ABCs - O2, IV access, Fluids |
|
|
When is thrombolysis (TKA) preferred over reperfusion (PCI)? |
Currently PCI is the preferred choice and should be given within 90 minutes. If not available, thrombolysis within 30 minutes. |
|
|
Name 4 advantages of LMWH (enoxaparin or daltaparin) over unfractionated heparin. |
1. more predictable effect |
|
|
Give 6 examples of when Beta-blockers be avoided in MI |
1. Inferior MI |
|
|
4 treatments for Methanol ingestion |
1. Ethanol if patient is allergic to fomepizole or not available |
|
|
A 50 year old street person comes into the ER after ingesting 50cc of methanol. He has abdominal pain and is feeling nauseas. |
1. Ethanol if patient is allergic to fomepizole or not available. |
|
|
Ethylene Glycol |
1. antifreeze, laquers, detergents |
|
|
Give 3 test that give evidence of chronic alcohol ingestion. |
1. Elevated liver enzymes - especially GGT |
|
|
How should a patient intoxicated with EtOH be managed in the ER? |
1. Neurovitals q1h |
|
|
How should EtOH withdrawal be managed? |
1. CIWA protocol |
|
|
Describe your management of Delerium Tremens. |
1. ABCs - consider sedation with propofol and intubation and monitored bed. |
|
|
Wernicke's Encephalopathy |
1. Thiamine deficiency secondary to chronic EtOH abuse |
|
|
Pt. presents to ED suffering from multiple trauma. What is the minimal acceptable urinary output? |
d) 30cc/hr * |
|
|
Which of the following are at the highest risk of Tetanus wound infection? (Select 4) |
a) wound of 12 hours duration * |
|
|
Which of the following are commonly used to manage near drowning survivors? (select 4) |
a) supplemental oxygen * |
|
|
Which age groups have the highest risk of drowning? |
Toddlers and teens |
|
|
Name 6 risk factors that contribute to drowning |
1. toddlers and teens |
|
|
Give 6 reasons why hypoxemia results from near-drowning. |
1. loss of surfactant leads to atelectasis |
|
|
Define Dry-Drowning |
Aspiration of water leads to laryngospasm and respiratory failure without water entering the lungs. |
|
|
Name 7 investigations that should be done in all near-drowning patients. |
1. CXR |
|
|
Give 5 treatments for a near drowning. |
1. Oxygen by face mask or BiPAP |
|
|
If a woman discloses that she is being abused, it is often very helpful to: (select 4) |
a) let her know that you are glad she could tell you about it * |
|
|
A 9 mo. old boy arrives in your ED with a barking cough and stridorous breathing which woke him up 2 hours ago from his sleep. RR=50, HR=120, T=38.5C, chest retractions present. He vomited twice in the car on the way to the hospital. Your first step is to provide the child with humidified oxygen. The child remains very stridorous at rest and the vital signs remains unchanged. You now: (select 2) |
1. |
|
|
A 60 day old infant presents to ED unwell and decreased oral intake. Based on the Rochester Criteria, which of the following would you ask the mother: |
All the above |
|
|
Which of the following can you administer via an ETT? (Select 4) |
NAVEL |
|
|
A G2P2 female presents with 2 day Hx of RLQ pain. Her LMP was 2 wks ago and she’s known to have irregular periods. She has not noticed any vaginal bleeding. Select 4 most likely differential diagnoses: |
a) hepatitis -no Hx to suggest |
|
|
10 features that can increase scarring when a laceration is sutured. |
1. Leaving devitalized tissue |
|
|
1. 4 time dependent, essential items for treatment in sexual assault. |
1. Pregnancy - 2 Ovral tablets orally q12h or 2 tabs plan B STAT. |
|
|
What is the upper time limit for primary wound closure with a laceration? |
6-8 hours |
|
|
A palliative patient has been using 25mg of hydromorphone in a 24 hour period. What should his breakthrough dose be? |
1/10th of 24h dose, or 2.5mg. |
|
|
1. A palliative patient presents to the ER in an acute pain crisis and takes 360mg of morphine a day. What should his initial dose be? |
1. 1/10th daily dose = 36mg IV! |
|
|
You prescribe a patient a 4mg q4h hydromorphone dose for acute cancer pain. what should the breakthrough dose be? |
2mg q1h (50% of q4h dose). |
|
|
Nausea and Vomiting |
1. Chemo acts at the N+V center via 5HT3 - use odansatron 8mg IV q8h |
|
|
Give a stepwise approach to management of constipation. |
START from below and then from above. |
|
|
Give 4 treatments for acute delerium. |
1. control the environment - clocks, lights, noises |
|
|
1. Name 2 treatments for the death rattle. |
1. Scopolamine 0.6mg SC q4h prn or glycopyrrolate 0.6mg SC q4h prn. |
|
|
You are assessing and resuscitating a trauma patient with your mentor. Things are going well, when, just as you being the secondary survey, the patient begins to deteriorate. The FIRST thing that should be done is to: (1 mark) |
* Airway, breathing, circulation |
|
|
What is the minimum systolic blood pressure required to produce a palpable pulse in the following areas (3 marks) |
Carotid: 60 |
|
|
1. A 49 y/o male with a strong family history of coronary artery disease presents with retrosternal chest pain of 2 hours duration, associated with diaphoresis and dyspnea. His ECG in the ER is normal, and a CK & CK-MB done on arrival is negative. Can one reasonably rule out a myocardial infarction in this patient at this point? (1 mark) |
1) Troponin, CK & CK-MB rises above normal at least 6 hrs post MI - first test may be normal. |
|
|
What is the best way to diagnose hypothermia? (1 mark) |
Esophageal is the best measure, while Rectal temperature is more practical and more accurate than tympanic. |
|
|
Define hypothermia |
core body temperature <35 on rectal temp. |
|
|
What types of heat loss contribute to hypothermia and what % do they involve in heat loss? |
1. Radiation - 55% |
|
|
Give 6 risk factors for hypothermia |
1. Elderly, very young |
|
|
Describe 6 symptoms of hypothermia (core temp <32). |
1. Confusion, lethargy |
|
|
1. Why must you not rewarm the peripheral body in hypothermia? |
1. Peripheral rewarming leads to cold blood being recirculated to the heart and leads to fatal arrythmias - AFTERDROP. |
|
|
Briefly discuss the conditions which must be met for an Emergency Physician to administer treatment to a patient without the patient’s consent: (2 marks) |
* 1) Patient is incapable of consent and no SDM is available |
|
|
47. Pt. presents with severe headache lasting the past few days. What are the possible positive findings on CT? (4 marks) |
* extradural hematoma |
|
|
Pt. presents with severe pulmonary edema. What 2 adjunctive measures can be given in addition to medications (2 marks)? |
* CPAP / Bi-PAP / PPV |
|
|
Pt. presents with severe asthma and respiratory distress. List the steps of management, starting with where to place the pt. in the emergency room, and specifically how you will monitor the pt. (10 marks) |
1. Place pt. in acute area or resus if space available |
|
|
A chronic alcoholic presents to ED complaining of tachypnea. He was found to be in no respiratory distress and has no other complaints. Laboratory investigations are as follows: |
1. AG = Na - (Cl + HCO3) =20 (normal = <10) |
|
|
How do you calculate: |
1. Na - (Cl + HCO3) |
|
|
MUDPILES and Anion Gap. Give the words for the acronym. |
Methanol, Uremia, DKA, Polyethylene glycol, Isopropyl, Lactic, Ethylene glycol, Salicylates |
|
|
Regarding shoulder dislocation: |
a. * anterior |
|
|
1. Mechanism of action of penicillen and cephalosporins. |
Both are bacteriacidal Beta-lactams and inhibit cell wall synthesis. Cephalosporins are more resistant against penicillenases. |
|
|
1. Mechanism of action of aminoglycosides. |
Inhibit protein synthesis by binding to the 50S or 30S ribosomal subunit. |
|
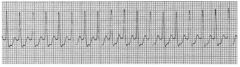
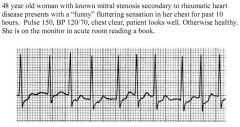
1. Dx |
|
|
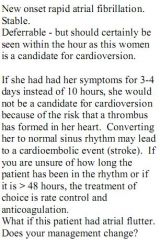
1. Dx |
|
|
1. Dx |
|
|
1. Dx |
|
|
1. What is the diagnosis? |
|
|
|
|
|
|
|
|
|
|
|
|
1. Give 3 clinical signs of an upper airway obstruction. |
1. a) drooling |
|
|
1. A 27 year-old man is brought into the ER after a bicycling accident. A car door suddenly opened in front of him, of which he smashed into and was thrown 15 feet. On examination, he is drowsy and confused. He opens his eyes when his name is called. He mumbles words that you understand but the sentences do not make sense. He moves all four limbs but does not respond to any commands. He is able to pull both hands away when pinched and squirms when his sternum is rubbed, making no effort to stop you. What is his Glasgow COMA Scale score? |
10 |
|
|
Which of the following are not consistent with primary (spontaneous) bacterial peritonitis? |
d. Multiple organisms on culture and sensitivity of ascitic fluid |
|
|
Prolonged vomiting is associated with what electrolyte abnormality? |
Hypochloremic hypokalemic metabolic alkalosis |
|
|
A 25 year-old known substance abuser is brought to the ED with a suspected overdose. Which of the following is not considered a universal antidote? |
Calcium gluconate - although useful for cardioprotection in hyperkalemia |
|
|
Give the numbers for GCS |

|
|
|
A 37 year-old male arrives at the Emergency Department unconscious. He is warm and sweaty. His heart rate is 52 bpm, his BP is 90/60. His pupils are constricted, his eyes are teary, and he is drooling. You assume he is suffering from a toxidrome. |
1. Cholinergic - salivation, lacrimatin, incontinence, diarrhea, bronchorrhea, bradycardia. |
|
|
A 16 year-old girl is brought to hospital by her frantic parents after a bee sting. Vitals signs are BP 70/40, RR 30 and laboured, HR 140, T 37.5. Which of the following would not be an option in her management? |
Atropine - it will increase heart rate |
|
|
Tension pneumothorax is best diagnosed with: |
Clinical exam & needle thoracostomy |
|
|
A patient presents with decreased level of consciousness. On exam he has pinpoint pupils and is unresponsive. Which of the following is NOT a likely etiology? |
TCA overdose - Causes an anticholinergic toxidrome - Dilated, Dry, Red, Hot. |
|
|
How do you assess a patient that presents to the ED? When do you restart this assessment? |
Airway/C-spine, Breathing, Circulation, Disability, Environment/Exposure. Restart when conditions deteriorates. |
|
|
How does consent change in the context of Emergency Medicine (EM)? |
Consent is not needed when patient is at imminent risk from serious injury AND obtaining consent is not possible. |
|
|
What is the Cushing’s reflex? |
Sign of increased ICP: high BP, low HR, irregular respirations |
|
|
What are the universal antidotes in EM? |
Oxygen, glucose, naloxone, thiamine |
|
|
What should every patient with an MI receive? |
1. ASA chewed - 160mg |
|
|
What are the signs of a basal skull fracture? |
Battle sign, hemotympanum, racoon eyes, CSF otorrhea/rhinorrhea |
|
|
Shock in a trauma patient is ____ until proven otherwise? |
Hemorrhagic |
|
|
Level of consciousness is assessed using what scale? |
GCS or AVPU |
|
|
At what GCS should you intubate? |
8 or less |
|
|
Name 1 KEY investigation for a potential spinal cord trauma patient? |
C-spine X-rays with 4 views - AP, Lat, Swimmer and Odontoid |
|
|
What is the management of a tension pneumothorax? |
11. Large bore IV needle inserted into 2nd ICS mid-clavicular line, followed by chest tube in 5th ICS ant-axillary line |
|
|
What imaging modalities should be considered in abdominal trauma? |
FAST, DPL, X-ray, CT |
|
|
For penetrating trauma, when is laparotomy mandatory? |
Shock, peritonitis, evisceration, free air, gunshot, blood in NG, Foley, or on DRE |
|
|
What are the contraindications to a Foley catheter? |
Blood at the urethral meatus, ecchymosis of the scrotum, “high riding” prostate |
|
|
What nerves are at risk with an anterior shoulder dislocation? |
Axillary nerve (lateral), and musculocutaneous nerve (extensor aspect of forearm) |
|
|
When is an X-ray series of the ankle required? |
Any pain in the malleolar zone AND tenderness in either malleolar zone OR inability to weight bear |
|
|
When is an X-ray series of the foot required? |
Any pain in the midfoot zone AND Tenderness at the navicular or 5th metatarsal OR inability to weight bear |
|
|
1. What is the maximum dose of subcutaneous lidocaine that can be given with and without epinephrine? |
1. 7 mg/kg with epinephrine, 5 mg/kg without epinephrine |
|
|
Where should lidocaine with epinephrine NOT be used? |
Ears, nose, fingers, toes, and hose (penis) |
|
|
What is the most commonly used antibiotic for cellulitis? |
Cefazolin/Ancef (IV) and Cephalexin/Keflex (PO) |
|
|
What is the first line antibiotic for human bites? |
Amoxicillin + clavulinic acid |
|
|
What are the 2 leading causes of death in the age group of 1-44 y/o? |
1. Trauma |
|
|
When do the majority of deaths occur in trauma? What is our goal in trauma resuscitation/ |
In the first hour, in the field. These are the unsalvageable. Our goal is to reduce the early deaths in the first 4 hours or the "Golden Hour". |
|
|
Describe the GENERAL approach to assessment and resuscitation of the trauma patient. |
1. Primary Survey - ABCDE |
|
|
Describe the step-wise approach to management of an airway in a trauma patient. |
1. Chin lift |
|
|
Tension Pneumothorax |
1. |
|
|
Name 6 clinical features that you can monitor to evaluate for shock. |
1. Level of consciousness |
|
|
Name the potential causes of shock. |
SSHOCK |
|
|
How can you manage an open book fracture of the pelvis in the ER? |
Wrap a bedsheet around the patient and tie tight. This will tamponade the amount of blood that can collect in the pelvis. |
|
|
A patient was invovled in a car accident 30 minutes ago. The FAST shows a splenic rupture and he is now hypotensive. |
1. 2L blous of NS |
|
|
What does AVPU mean? |
Used in place of GCS in trauma patients. |
|
|
What is the single most important radiology investigation in the trauma patient? Second? |
CXR |
|
|
Give 6 indications to send a trauma patient directly to the OR. |
1. Evisceration |
|
|
Give 3 signs of a basal skull fracture. |
1. racoon eyes |
|
|
Give 3 contraindications to an NG tube. |
1. Suspected basal skull fracture |
|
|
Describe the features that you need to see on X-Ray to clear a c-spine (5). |
Think General and ABCD |
|
|
Describe your approach to Pulseless Electrical Activity and Asystole |
ABCs, 6H's and 5T's |
|
|
Describe your approach to bradycardia with circulatory compromise. |
ABCDs and: |
|
|
1. What are the indication for Synchronized Electrical Cardioversion? |
Synchronized electrical cardioversion is performed on unstable tachycardias with circulatory compromise due to the fast rate |
|
|
When would you perform Unsynchronized Electrical Cardioversion? |
Give unsynchronized shocks at VF/PVT energy levels without delay for unstable tachycardia with critical circulatory compromise due to the fast rate - VT/VF. Also give unsynchronized shocks if you cannot synchronize, or if polymorphic VT is present. |
|
|
How should you approach a stable, narrow, regular tachycardia? |
1. Stable? Yes |
|
|
1. Give a DDx for the following rhythms. |
1. Narrow Irregular Tachycardia |
|
|
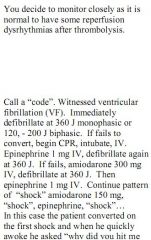
Describe the Ventricular Fibrillation (VF)/Pulseless Ventricular Tachycardia (PVT) Algorithm |
SCREAM |
|
|
Hypercalcemia |
1. |
|
|
Causes of Ketonuria |
1. Dehydration and decreased PO intake |
|
|
Give 5 contraindications to Tenectaplase (TKA). |
1. Recent Stroke - 3 mo |
|
|
Give 3 side effects of Tenectaplase (TKA). |
1. Reperfusion arrythmia - don't need to treat |
|
|
How does treatment differ in MI with cardiogenic shock? |
1. TKA will not be effective due to decreased coronary perfusion. |
|
|
What are the treatment goals for TKA and PCI and when should you no longer administer? |
1. 90 minutes from arrival for PCI |
|
|
TKA and PCI |
1. INDICATIONS |
|
|
A pt. comes into the ER comatose, found on the street. You're not sure what the toxidrome is. Name 3 drugs you can give NOW. |
1. Thiamine |
|
|
Describe a RAPID NEUROLOGICAL EXAM on a comatose patient. (4). |
1. Head and Neck - Skin, Skull, Tympanic,C-Spine X-rays, Flex neck for Menigitis. CN - PERL, fundi, corneal and gag reflex. |
|
|
You have a comatose patient with focal neurological findings - left hemiparesis. You also suspect menigitis. Should you do an LP? |
NO! Need a head CT with any focal signs in order to rule out increased intracranial pressure and prevent herniation. |
|
|
Give the criteria for a MIGRAINE Headache. |
TWO of |
|
|
Give 5 treatments for Migraine Headache in the ER. |
USE ALL of These Together: |
|
|
Give 4 treatments for the PREVENTION of MIGRAINES. |
1. Beta-Blockers |
|
|
What is the most sensitive test for Subarachnoid Hemorrhage? |
LP - 100% sensitive by 12 hours and Xanthochromia lasts up to 14 days. |
|
|
Name 5 features of a Subarachnoid Hemorrhage Headache. |
1. Sudden onset |
|
|
GIve 5 features of a headache that is due to INCREASED ICP. |
1. Worst in morning |
|
|
Give 5 features of a headache due to MENINGITIS. |
1. Fever |
|
|
Describe Kernig and Brudzinski Signs. |
Meningitis Signs. |
|
|
Temporal Ateritis |
1. Over 50, temporal headache, tenderness to temporal artery, +/- visual changes and eventually blindness. |
|
|
How should MENINGITIS be treated in the adult patient? (2) |
1. Start empiric antibiotics before LP results or diagnosis. AMP + CEFT + VANCO or AMP + CEFT + GENT |
|
|
GENERIC NAME: cyclobenzaprine |
GENERIC NAME: cyclobenzaprine |
|
|
Acute MI - Give 8 Medications and their contraindications. |
1. ABCs (O2, ECG etc.) |
|
|
Give 2 definitions of acute MI |
1. ST elevation in 2 contiguous leads greater than 1mm of elevation. |
|
|
A 27 year-old man is brought into the ER after a bicycling accident. A car door suddenly opened in front of him, of which he smashed into and was thrown 15 feet. On examination, he is drowsy and confused. He opens his eyes when his name is called. He mumbles words that you understand but the sentences do not make sense. He moves all four limbs but does not respond to any commands. He is able to pull both hands away when pinched and squirms when his sternum is rubbed, making no effort to stop you. What is his Glasgow COMA Scale score? |
10 |
|
|
Which of the following are not consistent with primary (spontaneous) bacterial peritonitis? |
d) Multiple organisms on culture and sensitivity of ascitic fluid |
|
|
Describe the features, risk factors and criteria for Spontaneous bacterial peritonitis (SBP). |
Spontaneous bacterial peritonitis (SBP) is an acute bacterial infection of ascitic fluid. Generally, no source of the infecting agent is easily identifiable, but contamination of dialysate can cause the condition among those receiving peritoneal dialysis (PD). Spontaneous bacterial peritonitis occurs in both children and adults and is a well-known and ominous complication in patients with cirrhosis.1 Of patients with cirrhosis who have spontaneous bacterial peritonitis, 70% are Child-Pugh class C. In these patients, the development of spontaneous bacterial peritonitis is associated with a poor long-term prognosis. Once thought to occur only in those individuals with alcoholic cirrhosis, spontaneous bacterial peritonitis is now known to affect patients with cirrhosis from any cause. |
|
|
A 25 year-old known substance abuser is brought to the ED with a suspected overdose. Which of the following is not considered a universal antidote? |
c) Calcium gluconate |
|
|
4) Prolonged vomiting is associated with what electrolyte abnormality? |
b) Hypochloremic hypokalemic metabolic alkalosis |
|
|
5) A 37 year-old male arrives at the Emergency Department unconscious. He is warm and sweaty. His heart rate is 52 bpm, his BP is 90/60. His pupils are constricted, |
d) Atropine |
|
|
6) A 16 year-old girl is brought to hospital by her frantic parents after a bee sting. Vitals |
e) Atropine |
|
|
7) Tension pneumothorax is best diagnosed with: |
d) Clinical exam |
|
|
8) A patient presents with decreased level of consciousness. On exam he has pinpoint |
b) TCA overdose |
|
|
9) A 41 y/o male alcoholic is brought into the ED by ambulance. He has been seizing for |
d) Ordering a stat EEG |
|
|
Calcium Channel Blockers - classify |
Classify - Dihydropyridine (pines) – amlodipine and nefedipine (Norvasc and Adalat) – relax cardiac and smooth muscle. Non- Dihydropyridine – Diltiazem and Verapamil – same as above and inhibits AV and SA nodes |
|
|
Mechanism of action of Calcium Channel Blockers |
Dihydropyridine – inhibit Ca++ influx into cardiac and smooth muscle cells, relaxing vessels and the heart . Non- Dihydropyridine - same properties as above, plus inhibits AV node and SA node to lesser extent |
|
|
Uses of Calcium Channel Blockers. |
Uses - Dihydropyridine (pines) – HTN, Migraine prevention. Non-Dihydropyridine – Angina, PSVT, Atrial Fib/ Flutter |
|
|
Name 3 side effects of calcium channel blockers. |
Hypotension, leg edema and |
|
|
Describe the symptoms, ecg features and management of PSVT |
Asymptomatic, usually young male with palpitations. Regular sinus tachycardia 150-180bpm. Vagal manoevres, adenosine 6mg x2 then 12mg. |
|
|
Describe the symptoms, key features and management of Pulmonary Hypertension |
Management – Sildenafil, Prostacyclin or Bosantin |
|
|
Describe how endothelial cell relaxation and constriction is medicated , how the various treatments work on this system and the connection to Pulmonary Hypertension. |
2 parallel cycles – endothelin vs. NO, Prostacyclin vs. Thromboxane. Relaxation – mediated by NO and prostacyclin – Sildenafil increases NO concentration, Prostacyclin works against thromboxane to relax endothelial cells. Constriction – Endothelin and Thromboxane |
|
|
How should niacin be taken, most common side effect and how to minimize it? |
Take at night with some lifh food, most common side effect is flushing, can couterqct it in those that have it by taking ASA 325mg 30 minutes prior to niacin. |
|
|
How should you manage hypertension in heart block syndromes such as a Mobitz Type 2 Wenkeback? |
NEVER give Non-Dihydropyridin (diltiazem and verapamil)), Beta-Blocker or Digoxin. Consider ACEi, ARB, HCTZ |
|
|
How should niacin be taken, most common side effect and how to minimize it? |
Take at night with some lifh food, most common side effect is flushing, can couterqct it in those that have it by taking ASA 325mg 30 minutes prior to niacin. |
|
|
What is the role of High-sensitivity C-reactive protein in relation to CAD? |
High-sensitivity C-reactive protein may be clinically useful in identifying individuals who are at higher risk for CAD than that predicted by a global risk assessment, in particular in patients with abdominal obesity or a calculated 10-year risk between 10% and 20%. A high-sensitivity C-reactive protein level of less than 1.0 mg/L indicates low risk for cardiovascular disease, between 1.0 mg/L to 3.0 mg/L indicates moderate risk and more than 3.0 mg/L indicates high risk. High risk patients should have their LDL aggressively lowered to below 2, ideally 1.5. |
|
|
Give 4 treatment options for an elevated LDL. |
Atorvastatin/Lipitor 10 mg - 80 mg, Rosuvastatin/Crestor 10 mg - 40 mg, Simvastatin/Zocor 10 mg - 80 mg, Ezetimibe 10 mg, Bezafibrate 400 mg, Fenofibrate 100 mg, Niaspan 0.5 g - 2 g |
|
|
Give 3 side effects of losartan and ARBs. Give a standard dose for CHF and evidence supporting use. |
Hypotension, hyperkalemia and and renal impairment. HEAAL STUDY Lancet 2009 shows that 150mg od reduces mortality in NYHA 2-4 in those intolerant to ACEi and should be titrate up to this dose unless side effects supersede. |
|
|
Give 4 side effects of ACEi |
Hypotension, hyperkalemia, renal impairment and cough is most common. |

