![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
294 Cards in this Set
- Front
- Back
|
What is aneuploidy?
How often does it happen? |
Abnormal number of chromosomes. Happens once in 160 births
|
|
|
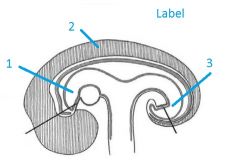
How does Spermatogenesis happen?
|
1. Spermatogonia to spermatids (via miosis)
2. Spermatids to spermatozoa (via process called spermiogenesis) Whole process takes 9 weeks. |
|
|
What is the acrosome?
|
Region on the sperms head that contains the hydrolytic enzymes.
|
|
|
What constitutes seminal fluid?
|
60% contributed by seminal vesicles, 30% by prostate, 10% by bulbourethral glands
|
|
|
What are the 3 roles of seminal fluid?
|
1. nutrient source for sperm
2. neutralize vaginal acidity 3. promote sperm motility |
|
|
What is azoospemia?
Oligospermia? |
-no sperm
- deficiency of sperm |
|
|
Once in the vagina how long do sperm survive?
|
Usually 2 days, but maximum is between 5 and 6 days
|
|
|
What is capacitation?
Is it species specific? |
Once the sperm spend 4 to 6 hours in the female rep system, sperm motility and metabolism rocket
- needed for egg binding and acrosome reaction - not species specific |
|
|
Describe the process of oogenesis.
|
primary oocyte->secondary (meiosis 1, begins in fetal ovary, doesnt complete until ovulation)
- secondary oocyte-> ovum ( meiosis 2 begins just before ovulation, doesnt complete if the egg is not fertilized) |
|
|
What is a primordial follicle?
|
Primary oocyte surrounded by a single layer of flat epithelial cells.
|
|
|
Where does spermatogenesis happen?
|
Seminiferous tubules.
|
|
|
What is the normal sperm concentration?
|
40-200e6 sperm per ml of semen
|
|
|
What is theca?
|
Outermost cells of follicle that secrete the substrate used by the granulosa cells to make estrogen.
|
|
|
What is the cumulus oophorus?
|
Cells that surround the oocyte, and that are surrounded by the crescent shaped antrum.
|
|
|
What makes the zona pellucida?
|
Granulosa cells.
|
|
|
What is the Oocyte maturation inhibitor?
|
Substance secreted by the granulosa cells that arest the primary oocyte in the prophase I of meiosis.
|
|
|
What is a "stigma"?
Hint: Graafian follicle |
An avascular spot on the surface of the ovary
|
|
|
What spikes when a secondary follicle is mature?
|
Luteinizing hormone.
|
|
|
Upon completion of meiosis I, where does the first polar body lay?
|
In the perivitelline space, between the plasma memb. of the secondary oocyte and the zona pellucida.
|
|
|
What makes up the corona radiata?
|
Granulosa cells surrounding the secondary oocyte.
|
|
|
What are the 3 roles of corona radiata cells?
|
1. Assist in ovum pickup (getting into the uterine tube)
2. Increase target size for the sperm 3. trap -> direct sperm right to the nucleus of the ovum |
|
|
What is the species specific receptor involved in the zona pellucida-sperm binding?
|
ZP3
|
|
|
What reaction is triggered by sperm binding to the zona pell.?
|
Acrosome reactoin
|
|
|
How is polyspermy blocked?
|
Via the Zona reaction:
Contact between sperm and oocyte membranes triggers the release of cortical granules, making oocyte membrane impermeable to sperm. |
|
|
When does the first embryo cleavage take place?
|
24 hours following production of 2nd polar body
|
|
|
Cells formed by cleavage are called__________.
|
Blastomeres. Cluster of blastomeres = morula.
|
|
|
What does totipotential mean?
|
A totipotential blastomere can form an entire organism.
|
|
|
What are the two regions in a compacted morula?
|
The outer layer is called the trophoblast and the inner part = inner cell mass.
TB: responsible for the implantation ICM: develops into the embryo |
|
|
When does the blastocyst cavity appear in the morula?
What happens to the ICM at this point? |
@ 32 cell stage ( 4 days after fertilization).
ICM pushed off to a pole. |
|
|
When is zona pellucida broken down?
|
At day 5/6
|
|
|
What is a syncytiotrophoblast?
What does it produce? |
multinucleated mass that forms at the site where the trophoblast contacts the endometrium; it burrow through the endometrium
-> it produces the human chorionic gonadotrophin (hCG) |
|
|
What is :
salpingstomy? salpingectomy? |
1) removing the embryo from the uterine tube (via a hole)
2) removing an entire uterine tube |
|
|
When is a bilaminar embryo formed?
Describe it. Describe the boundaries of the amniotic cavity. |
- at the same time an embryo implants
- the layer of ICM facing towards the syncitiotroph. is called the embryonic EPIBLAST and the layer facing the blastocyst cavity is called the embryonic HYPOBLAST. Amniotic cavity = space between the Epiblast and the cytotrophoblast. Ultimately, the borders of the amnitic cavity will completely be derived from the ICM |
|
|
How is the primitive yolk sac formed?
|
The hypoblast grows out forming the pouch
|
|
|
When does the first embryo cleavage take place?
|
24 hours following production of 2nd polar body
|
|
|
Cells formed by cleavage are called__________.
|
Blastomeres. Cluster of blastomeres = morula.
|
|
|
What does totipotential mean?
|
A totipotential blastomere can form an entire organism.
|
|
|
What are the two regions in a compacted morula?
|
The outer layer is called the trophoblast and the inner part = inner cell mass.
TB: responsible for the implantation ICM: develops into the embryo |
|
|
When does the blastocyst cavity appear in the morula?
What happens to the ICM at this point? |
@ 32 cell stage ( 4 days after fertilization).
ICM pushed off to a pole. |
|
|
When is zona pellucida broken down?
|
At day 5/6
|
|
|
What is a syncytiotrophoblast?
What does it produce? |
multinucleated mass that forms at the site where the trophoblast contacts the endometrium; it burrow through the endometrium
-> it produces the human chorionic gonadotrophin (hCG) |
|
|
What is :
salpingstomy? salpingectomy? |
1) removing the embryo from the uterine tube (via a hole)
2) removing an entire uterine tube |
|
|
When is a bilaminar embryo formed?
Describe it. Describe the boundaries of the amniotic cavity. |
- at the same time an embryo implants
- the layer of ICM facing towards the syncitiotroph. is called the embryonic EPIBLAST and the layer facing the blastocyst cavity is called the embryonic HYPOBLAST. Amniotic cavity = space between the Epiblast and the cytotrophoblast. Ultimately, the borders of the amnitic cavity will completely be derived from the ICM |
|
|
How is the primitive yolk sac formed?
|
The hypoblast grows out forming the pouch
|
|
|
What is a teratoma?
|
encapsulated tumor with tissue or organ components resembling normal derivatives of all three germ layers
|
|
|
How is the notochord formed?
|
- epiblast cells ingressing thought the Hensens node rostrally up the middle between ecto & endoderm form the notochord.
- |
|
|
What is formed by the ectoderm?
|
CNS/skin/epidermis/hair/nails & glands(sweat & sebaceous)
|
|
|
Describe the process of neurulation.
|
1) Notochord and paraxial mesoderm induce overlying ectoderm to become the neural plate.
2) Neural folds elevate (medially made up of neural plate, laterally, nonneuro ecto) 3) neural folds fuse forming the neural tube which becomes brain and spin chord. Laterally, neural crests will be formed. |
|
|
Describe the fusion of neural folds.
|
THe fusion first happens at the cervical segments. it then proceeds caudally and rostrallly from there. Last parts to fuse are called neuropore (caudal and rostral).
|
|
|
What is myeloschisis?
What is anencephaly? |
@ caudal end, the neural folds dont close
Neuroectoderm interacts with the amnionic fluid, no skull forms, recognizable on the US -> failure of fold closing in the caudal part |
|
|
What structures are formed by the neural crest cells?
|
- sensory neurons of dorsal root gang
- endocrine cells in medulla of adrenals - schwann cells of peripheral nerves -melanocytes -symph chain ganglia |
|
|
CNS neurons are developed from ________ cells in the wall of the _______________.
|
neuroectoderm cells, neural tube
|
|
|
The Treacher Collins syndrome is caused by malfunction of which cells?
|
neural crest cells => leads to craniofacial deformities
|
|
|
What does endoderm develop into?
|
-lining tissue of GI tract, secretory cells of the liver, gall bladder and pacnreas, lining of the resp system
|
|
|
The endoderm is immediately opposite to the __________.
|
Yolk sac
|
|
|
What is paraxial mesoderm?
|
Mesoderm lateral to the notochord.
|
|
|
What develops from the primitive foregut?
|
mouth, esophagus, stomach, duodenum to the bile duct opening
|
|
|
What develops from the primitive hindgut?
|
large intestine, bladder & urethra
|
|
|
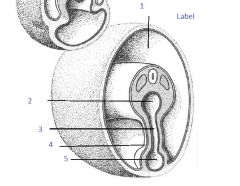
1. Primitive Foregut
2. Neuroectoderm 3. Primitive Hindgut |
|
|
Folding in the Long Axis is due to _______.
|
elongation of the neural tube.
|
|
|
What causes the sides of the embryo to fold?
|
Enlargement of somites (results in the transverse axis fold).
|
|
|
What connects the primitive midgut to the yolk sac?
|
Vitelline ducts (aka yolk stalk)
|
|
|
What becomes of the prim midgut?
|
small intestine: from the CBD openning to the ileocecal junction
large intestine: cecum to distalk part of trans. colon |
|
|
What is responsible for Meckel's diverticulum?
|
Persisting yolk stalk, usually disappears @ 6 weeks.
|
|
|
1. Amniotic cavity
2. Prim Midgut 3. Vitelline Duct 4. Umbillical cord 5. Yolk sac |
|
|
Mesoderm forms most of ______ and ______ tissues in the embryo.
|
Muscle, connective
|
|
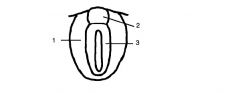
Label the numbered structs
|
1. Paraxial mesoderm
2. Intermediate mesoderm 3. lateral plate mesoderm |
|
|
What are somites?
What do they develop into? |
from in the craniosacral sequence as paired blocks of paraxial mesoderm.
They become cerebral disks and vertebra, ribs, skel muscles of body wall & limbs |
|
|
What is located between the somatic & splanchnic mesoderm?
|
Intraembryonic coelom.
( somatic mesoderm is outermost/parietal) |
|
|
What does somatic mesoderm give rise to?
|
- conn tissues
- blood vessels - smooth muscle of body wall and limbs |
|
|
What does splanchnic mesoderm give rise to?
|
-SM, BV and conn tissue of the GI organs
|
|
|
What does the intraembryonic coelom become?
|
Major body cavities:
- pleural - pericardial - peritoneal |
|
|
Urinary and reproductive systems develop from which part of the embryo?
|
Intermediate mesoderm.
|
|
|
When does the embryonic period occur?
Describe the two stages. |
Between weeks 0-8.
0-2 -> implantation 2-8 -> morphogenesis and organogenesis |
|
|
For a defect happening in the listed time frame, describe the likely nature of the defect:
1) 0-2 weeks. 2) Gastrulation 3) 4-8 weeks 4) Fetal period |
1) death
2) multiple significant abnormalities 3) organ specific malform. 4) Growth retardation/ functional defects (i.e. endocrine, enzyme deficiency) |
|
|
What is a laryngotracheal diverticulum?
|
A ventral outgrowth of the rostral part of prim foregut
|
|
Label the numbered parts
|
1. Laryngotracheal diverticulum
2. Tracheoesophageal ridge 3. Prim Foregut 4. Tracheoesophageal septum |
|
|
What forms the conn tissues/muscles/pleura and vessels of the lung?
|
Splanchnic mesoderm
|
|
|
What is a tracheo-esophageal fistula?
How common is it? |
90% of time uppper portio of esophagus ends in a blind pouch and the lower part of esoph. forms a fistule with the trachea
1:3000 births, more common in males |
|
|
What controls airway branching during lung development?
|
Mesoderm via Fibroblast Growth Factor (FGFs)
|
|
|
The lung branch development takes place up to when?
|
8 years.
|
|
|
What substance can stimulate surfactant production (ie during a preterm birth)?
|
Glucocorticoid steroids.
|
|
|
Increased thickness of the blood:air barrier is a result of which disease in the developing fetus?
|
Hyaline membrane disease.
|
|
|
Growth of lungs after birth is mainly due to an increase in the number of alveoli.
True/False? |
True
|
|
|
Describe the development of the diaphragm.
|
The Pleuroperitoneal folds close, joining with the septum transversum. Also, the mesentary of the esophagus contributes a part.
|
|
|
What happens when the pleuroperitoneal membrane is absent?
|
Intestine occupies the space where the lung is trying to develop => mediastinum shift!
|
|
|
Pericardial Cavity is derived from _________.
|
Intraembryonic coelom.
|
|
|
What is the primitive heart tube made up of?
|
1. endothelium
2. cardiac jelly 3. myocardium layers |
|
|
Heart develops in which primitive tissue layer?
|
Splanchnic mesoderm
|
|
|
Arrange the following from most rostral to most caudal:
primitive ventricle, primitive atrium, bulbus cordis, sinus venosus, truncus arteriosus |
truncus arteriosus, bulbus cordis, primitive ventricle, primitive atrium, sinus venosus
|
|
|
Which way does the primitive heart tube kink?
What happens when it kinks the other way? |
It kinks to the right, when it kinks to the left you get dextrocardia.
|
|
|
From which primitive heart structure do the aorta and pulmonary trunk develop from?
|
Truncus arteriosus.
|
|
|
What develops from bulbus cordis?
|
Smooth parts of both ventricles
|
|
|
What develops from the primitive ventricle?
|
Trabeculated parts of both ventricles.
|
|
|
What develops from the prim atrium?
|
Trabeculated parts of both atria.
|
|
|
From which primiitve cardiac structure does the coronary sinus develops from?
|
Sinus venosus ( also gives rise to the sinus venarum).
|
|
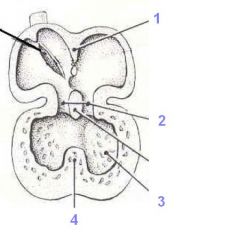
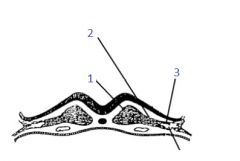
Label the following developing heart image
|
1. Sinus primum
2. Endocardial cushions 3. Left ventricle 4. Interventricular septum |
|
|
What directly surrounds the cardiac tube? What surrounds that layer?
|
1st is cardiac jelly then outside of it is myocardium and then the pericardial cavity.
|
|
|
Sinuatrial Junction is between ____ and ______
|
sinus venosus and primitive atrium
|
|
|
What are Endocardial cushions?
|
Outgrowths of the dorsal and ventral walls of the heart tube, which grow into the atrioventricular canal, splitting the passageway into two canals
|
|
|
What is the gap between the septum primum and endocardial cushion called?
|
Foramen primum
|
|
|
How is foramen secundum formed?
|
Apoptosis of the septum primum
|
|
|
Describe the position of septum secundum in relationship to the septum primum.
|
It develops on the right atrial side of the septum primum.
|
|
|
Which structure forms the valve of the foramen ovale?
|
Septum primum
|
|
|
What forms the auricle of right atrium?
|
Remains of the primitive atrium
|
|
|
Where does the sinus venarum go as heart development progresses?
|
To the side of right atrium
|
|
|
Left auricle forms from which primitive structure?
|
Primitive atrium
|
|
|
How is the aorticopulmonary septum formed?
|
The bulbar ridges fuse with the trunkal ridges, forming the septum.
|
|
|
True/False:Bulbus cordis is superior to truncus arteriosus.
|
False
|
|
|
What forms the infundibulum(smooth part of vent/conus arteriosus)? Where is it located?
|
Bulbar ridges and its in the RV.
|
|
|
How is the muscular part of the interventricular septum formed?
|
Expansion of ventricles.
|
|
|
What forms the membranous part of the interventricular septum?
|
Fused endocardial cushions
|
|
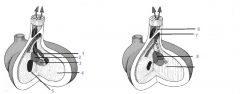
Name the structures
|
1. Left bulbar ridge
2. Right bulbar ridge 3. Endocardial cushion growth 4. Muscular interventricular septum 5. Right atrioventricular canal 6. Aorta 7. Pulmonary trunk 8 Membranous interventricular septum |
|
|
The end of the primitive hindgut is called the _______>
|
Cloaca.
|
|
|
What is a proctodeum?
|
Depression on the caudal external surface of the embryo.
|
|
|
Only the _____ is connected to the anterior body wall via a ventral mesentary.
|
Foregut
|
|
|
When does the vitelline duct disappear?
|
During 5/6th week.
|
|
|
Remnants of the vitelline duct are usually associated with the ____.
|
Ileum.
|
|
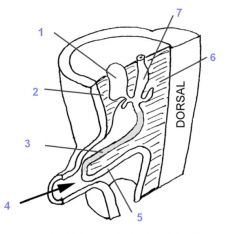
Label the numbered structs
|
1. Liver
2. ventral mesentary 3. Proximal half of midgut loop 4.Midgut loop projecting into the intra-embryonic body cavity 5. Distal half of the midgut loop 6. Dorsal mesentary 7. Stomach |
|
|
What is the rule of 2s concerning the vitelline duct remnants?
|
2% population have it
2" long @2' of terminal ileum 2x often in males |
|
|
Critical events in the development of the foregut (LONG):
|
1. Laryngotracheal diverticulum
2. Appearance of the gastric dilatation 3. Elongation of esophagus moving stomach into the abdomen 4. Occlusion of foregut proximal and distal to the gastric dilat. by endoderm 5. Cavitation (via vacuole formation): recanalization of foregut 6. Stomach rotates, taking mesentery to the left...dorsal mesentary forms the greater omentum + gastrolineal+ splenorenal ligaments, while ventral forms the lesser omentum + tria., falciform, coronary ligaments of the liver 7. Differential growth is responsible for the production of the greater curvature of the stomach. 8. Liver,pancreas + gallbladder Outgrowth |
|
|
What happens to the midgut loop as it returns to the abdomen during the 10th week of gestation?
|
It rotates 180 degrees counterclockwise.
|
|
|
Where is the cecum located once the midgut loop returns to the abdomen?
|
It is sub-hepatic.
|
|
|
What is an omphalocele?
|
Failure of the midgut loop to return to abdomen
|
|
|
What is Gastroschisis?
|
Rupture in the anterior body wall, usually on the right side of the umbilical cord, which allows the intestines to freely float in the amnionic fluid.
|
|
|
What is Umbilical hernia?
|
Delayed closure of the umbilical ring
|
|
|
The sigmoid colon develops from which primitive embryonic structure?
|
Prim hindgut.
|
|
|
How are the urogenital and anorectal canals formed?
|
They are partitioned by the cloaca via the urorectal septum
|
|
|
Urogenital sinus contributes to which 2 structures?
|
Bladder and urethra
|
|
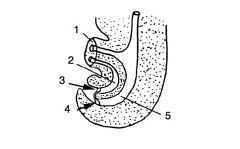
Label the structures numbered
|
1. Umbilical cord
2. Urogenital sinus 3. Urogenital membrane 4. Anal membrane 5. Rectoanal canal |
|
|
What is the cause of the congenital membranous atresia?
|
Failure of the anal membrane to disappear.
|
|
|
What are the 2 conditions associated with the dorsal deviation in the development of the urorectal septum?
|
Stenosis and possible complete atresia of the anus ( also called imperforate anus).
|
|
|
Outgrowth of endoderm near the distal part of the foregut gives rise to _________,_______ and _________
|
Liver, Gall bladder and pancreas.
|
|
|
As liver grows, which structure is responsible for the development of the falciform ligament?
|
Outgrowth of liver into the ventral mesentary
|
|

Label structs
|
1. Liver bud
2. Gall bladder 3. Ventral pancreatic bud 4. Dorsal pancreatic bud |
|
|
What brings the dorsal and ventral growths of the pancreatic ducts together?
|
1. Rotation of the gut
2. Differential growth of the foregut |
|
|
When the dorsal bud of the pancreas persists it becomes the ______________.
|
Accessory pancreatic duct.
|
|
|
Cranial part of the septum transversum makes a significant contribution to the development of ______________.
|
Diaphragm (central part).
|
|
|
Congenital diaphragmatic hernia happens when the ______________ fail to ______________.
|
i) Pleuroperitoneal folds
2) Close (separate the abdominal cavity from the thoracic cavity? |
|
|
When a congenital bower obstruction happens, the distension happens ______ to the site of obstruction.
|
Proximal
|
|
|
If there is forceful reflux at the time of feeding, the obstruction is _________.
|
Upper obstructions. When the reflux is less forceful, the obstruction is more distal.
|
|
|
What causes polyhydramnios?
|
Obstruction of the esophagus leads to an increase of net volume due to reduced clearance by swallowing.
|
|
|
Which two organs are susceptible to obstruction due to failure to recanalize?
|
duodenum and esophagus
|
|
|
What is congenital volvulus?
|
bowel becomes twisted on itself, cut off lumen and blood flow
|
|
|
What is meconium made up of?
|
Made up secretions, cells sloughed from the gut walls and lanugo hairs that have been swallowed with the amniotic fluid. Usually it is passed within the first 24 hours of birth.
|
|
|
What are the 3 developmental phases of the nephrogenic cords?
|
1. The pronephric phase
2. The mesonephric 3. The metanephros |
|
|
When does the pronephric phase start?
|
Late 3rd week.
|
|
|
How is the pronephric duct formed?
|
Cavities (vesicles) within the nephrogenic cord link up (opposite to the cervical segments of the embryo)
|
|
|
Remainder of the pronephric duct is called the ________.
|
Mesonephric duct. Appears during 4th week, when the pronephric part of the nephrogenic cord degenerates.
|
|
|
When does the mesonephric phase begin?
|
@ end of 4th week
|
|
|
Mesonephros degenerates during _______. Its remnants contribute to the __________.
|
4th month......male reproductive system.
|
|
|
Mesonerphric tubules develop and fuse/open in to the ____________.
|
Mesonephric duct.
|
|
|
What gives rise to the ureteric bud? When? Which signalling molecules are involved in this process?
|
It is an outgrowth of the caudal part of the mesonephric duct, during the 5th week.
FACTORs involves = HGF & GDNF released by the metanephric mass of mesoderm. |
|
|
Metanephric mass survives as a result of secretions of FGF2,TGFalpha and BMP7 by the ____________.
|
Ureteric bud.
|
|
|
What develops from the ureteric bud?
|
the urine collecting system
|
|
|
What develops from the metanephric mass of mesoderm?
|
Urine producing system (nephrons)
|
|
|
What signals the ureteric bud to start branching?
|
Metaneprhic mass secretes Wnt2b and TGFb
|
|
|
What happens when the branches of the ureteric bud and the nephrons from the metanephric vesicles dont fuse?
|
Nephrons cant drain and there might be cysts.
|
|
|
During kidney ascent, what other transformation happens?
|
They rotate medially, as initially the pelvi face anteriorly
|
|
|
True/False: Kidneys and adrenal glands develop at the same location.
|
False, kidneys migrate upwards and meet up with the adrenal glands.
|
|
|
How do kidneys acquire accessory renal arteries?
|
As they ascend, they don't give up the formal renal arteries /branches to aorta.
|
|
|
In fused kidneys, the full ascent is blocked by _____________.
|
The inferior mesenteric artery.
|
|
|
In 10% of the population, the ureteric bud splits prior to entering the metanephric mass. What is this called?
|
Bifid ureter.
If the the two ureteric bud branches are widely separated, you can get supernumerary kidney (3 of them). |
|
|
What happens in the case of the crossed ectopion?
|
Both kidneys on one side!
|
|
|
What is renal agenesis?
|
The ureteric bud fails to interact with the metanephric mass = no kidneys formed
|
|
|
Potter's facies are associated which renal malformation?
|
Renal agenesis.
|
|
|
Oligohydromnios is typically caused by....
|
bilateral renal agenesis or genitourinary obstruction, decrease in net volume of the amniotic fluid
|
|
|
Polyhydromnios is typically caused by....
|
obstructed bowel..increase in net volume of amniotic fluid
|
|
|
Segment of the mesonephric duct that is between the urogenital sinus and point where the ureteric bud opens into the sinus is called the ______________.
|
common excretory duct
|
|
|
Allantois becomes _____ which then becomes _____________.
|
Urachus......median umbilical ligament.
|
|
|
What is bladder extrophy?
|
When the bladder opens to the body surface
|
|
|
The urorectal septum is located between ___________ and ___________.
|
urogenital sinus and rectoanal canal.
|
|
|
@ indifferent stage of fetal development, how can the male and female fetuses be distinguished?
|
Presence of Y chromosome in male and the expression of HY antigen
|
|
|
Where do the gonads first appear?
|
Enlargement on the posterior abdominal wall medial to the mesonephros (gonadal ridge)
|
|
|
How are the sex cords formed?
|
Coelomic epithelium extensions penetrate the mesoderm of the ridge.
|
|
|
The primordial germ cells that appear during the 4th week, appear where?
When do these cells enter the sex cords? |
They appear in the yolk sac near the origin of allantois
@6 weeks these cells enter the sex cords, further stimulating gonad development |
|
|
What causes the sex cords to fragment?
|
Absence of the Y chromosome.
|
|
|
In females, the primordial germ cells become the _______.
What about the sex cords? |
Oogonia.
Sex cords develop into the follicular cells surrounding the oocytes. |
|
|
What happens to the sex cords in the presence of a Y chromosome?
|
Sex cords elongate, forming the seminiferous tubules.
|
|
|
What set of cells secretes the antimuellerian factor?
|
Sertoli cells.
|
|
|
What is the name of cells capable secreting testosterone?
|
Leydig cells.
|
|
|
Leydig calls arise from __________.
|
Mesoderm of genital ridge between the sex cords.
|
|
|
Spermatogonia form from___________.
|
Primordial germ cells.
|
|
|
What are the two phases of testicular descent?
|
1. Trans-abdominal phase
2. Trans-inguinal phase |
|
|
The ________ tethers the testicle to the scrotum.
|
Gubernaculum!
|
|
|
When does the testicle get to the mouth of the deep inguinal ring?
|
3rd month.
|
|
|
When does the trans-inguinal phase of testicle descent begin?
|
7th month of development.
|
|
|
What happens to the proximal part of the processus vaginalis?
What structure is formed by the distal part of the processus vaginalis? |
It degenerates.
The tunica vaginalis. |
|
|
Where does the testicle develop prior to its descent?
|
Between peritoneum and the rest of the body wall
|
|
|
The ligement of the scrotum forms from______.
|
The gubernaculum remnant.
|
|
|
What are cryptorchid testes?
What happens in the case of ectopic testes? |
Testes didn't descend all the way.
They got through the superficial inguinal ring, but they are not on the normal line of descent. |
|
|
What forms from the part of gubernaculum that attaches the ovary to the uterus?
|
Ligament of the ovary.
|
|
|
What structure gives rise to the round ligament of the ovary?
|
The part of gubernaculum between labium majus and the uterus
|
|
|
Muellerian ducts/ paramesonephric ducts grow alongside ________ into the developing pelvis.
|
Mesonephric ducts.
|
|
|
Uterovaginal primordium is formed by the fusion of ______ and ______.
|
Paramesonephric and mesonephric ducts (posterior to the urogenital sinus).
|
|
|
How is the vaginal plate formed?
|
Contact between the caudal tip of the uterovaginal primordium and the urogenital sinus posterior wall, triggers proliferation of cells of urogen. sinus to the utvag. primordium, and it is this mass of endoderm that is called the vaginal plate.
|
|
|
Antimuellerian hormone is produced by _______ cells (in male).
Due to secretion of this hormone, degeneration of these 2 structures happens in the male: 1) 2) |
Sertoli.
1)paramesonephric ducts 2)uterovaginal primordium |
|
|
In male development, androgens of Leydig cells induce:
1) 2) 3) |
1)formation of efferent ductules via linking of mesonephric excretory tubules with the rete testis
2) mesonephric duct to develop into epididymis, vas def, and ejac duct 3) seminal vesicles developing as outgrowths of mesonephric ducts |
|
|
What 3 things develop from the mesonephric duct in regards to male genital development?
|
vas def, epidydimis and ejac. duct
|
|
|
Prostatic utricle and appendix of the testes are remnants of ____ and ___.
|
uterovaginal primordium and paramesonephric ducts (in that order).
|
|
|
What happens to the paramesonephric ducts in the absence of antimuellerian hormone? What about the uterovag primordium?
|
They develop into uterine tubes .
Primordium develops into the uterus. |
|
|
In absence of testosterone, what happens to the mesonephric tubules?
What are the remnants called? |
They degenerate.
epoophoron and paroophoron ( associated with the broad lig) or associated with the uterus as a Gartner's cyst. |
|
|
Vagina develops from contriubutions of ______ and _______.
|
uterovaginal primordium and endoderm of the urogenital sinus (via vaginal plate)
|
|
|
When is the earliest time you can find out the sex of the baby by looking at the external genitalia?
|
9th week.
|
|
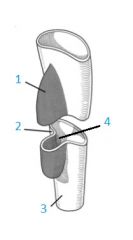
Label the swellings present at the indifferntiable stage of genital development
|
1.Labiosacral swellings
2. Genital tubercle 3. urogenital fold |
|
|
In a female, the glans clitoris develops from ______.
|
genital tubercle
|
|
|
Labia majora form from _________.
|
Labioscrotal swellings.
|
|
|
The penile urethra is formed by the __________.
|
Fusion of urogenital folds.
|
|
|
The scrotum is formed from the _______ _______.
|
Labioscrotal swellings.
|
|
|
During the male genital development, the glandular plate is formed by ___________.
|
invagination of the ectoderm on the ventral surface of glans. It then breaks down, forming a fissuer between the urogenital sinus and the space between the urogenital folds.
|
|
|
During male development, what is the site where testosterone is taken up and converted to dihydrotestosterone?
|
Cells of the urogenital sinus. Then DHTest enters the nucleus and mediates the masculization of the male genitalia @ week 10.
|
|
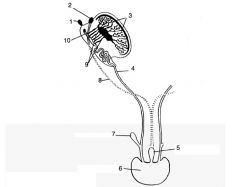
Label!
|
1.Appendix of epidydimis
2.Appendix of testis 3. Seminiferous tubules 4. vas deferense 5. prostatic utricle 6.Prostatic urethra 7. seminal vesicle 8. paramesonephric duct 9. efferent ductules 10. epidydimis |
|
|
Development of testis is brought on by factor ______, while development of ovaries _________.
hint: from indiff gonads |
SF1 male, WNT4 female
|
|
|
What happens in the pre-lacunar stage of placenta development?
What time period does it span? |
Blastocyst implantation, syncytiotrophoblast/cytotrophoblast development.
Days 6-8 |
|
|
What is a lacunae (context of placenta dev)?
|
vacuoles in syncytiotroph. (blood enters lacunae from mom)
|
|
|
When does primary villous stage take place?
|
days 12-15
|
|
|
Mesoderm conecting the embryo to the chorionic plate = ______
|
connecting stalk
|
|
|
What is responsible for formation of primary villi?
|
Penetrating cytotrophoblast
|
|
|
When does the tertiary villous stage start?
|
day 18
|
|
|
Extravilous cytotrophoblast cells participate in formation of ______ arteries.
|
Spiral.
|
|
|
What is the process of decidualization?
|
endometrial stromal cells and uter glands and vessels & immune cells are modified. Progstrn dependant
|
|
|
What are the 3 types of decidua?
|
1)Decidual Basalis (btwn emb & myomet)
2) Decidua capilaris 3) Decidua Parietalis (contacts chorionic leave) |
|
|
Deox blood from fetus to placenta via _____.
|
Arteries!
|
|
|
Describe the flow of oxygenated blood flow in the fetus.
|
1) Umb vein
2) ductus venosus 3) ivc |
|
|
Describe the conditions required for twin-twin tranfusion syndrome to happen.
|
common placenta & chorion, can have diff amnions
|
|
|
Which process is responsible for transfer of prots/polypeps via the placenta
|
Pinocytosis.
|
|
|
When does placenta start producing progesterone and what is the impact progstrn has?
|
4th month/maintain pregnancy
|
|
|
What is a hydatidiform mole?
|
nonviable egg impanted in uterus.
high hcg levels, can be cancerous 20% time (choriocarcinoma) |
|
|
What forms the myocoele?
|
Defined by the apical membrane of epithelial cells ( which got formed by transformation of mesenchymal cells)
|
|
|
When do somites form?
|
End of 3rd week.
|
|
|
Migration of neural crest cells out of neural tube to form the neurons of the dorsal root ganglia is guided by what?
|
They avoid the the caudal part of the somites ( avoid collagen type II, aggregan and ephirin).
|
|
|
When the ventromedial somites dissociate and transform to mesenchymal phenotype, what is the name of the structure they form?
What about the dorsolateral cells? |
Sclerotome (will form the bony parts of the vertebrea and the disks).
Myotome (muscles of the trunk). |
|
|
What do dermatome cells contibute to?
|
Skin formation.
|
|
|
How are vertebral discs formed?
|
From the middle parts of sclerotome pairs.
|
|
|
How are vertebral bodies formed?
|
Superiorpart is contributed by a caudal part of a sclerotome pair, while toe inferior part is contributed by the rostral piece.
|
|
|
What is Klippe Fiel syndrome?
|
Fused vertebra in neck.
|
|
|
What is spina bifida occulta?
What about meningocele/meningomyocele? |
15-20% of people. Unclosed arch.
Meningcele = CSF hernia through the opening. If chord is herniated = meningomyocele Both are vertebral defects. |
|
|
What is myeloschisis? Myelomeningocele?
|
No neural tube formed/
same+ herniation/cyst (no skin covering) both are neural tube defects. |
|
|
What is Arnold Chiari Malformation?
|
Blockade of foramen of Magendie leading to CSF accumulation due to cerebellar tonsils blocking flow/may lead to hydrocephalus
|
|
|
What is Arnold Chiari Malformation?
|
Blockade of foramen of Magendie leading to CSF accumulation due to cerebellar tonsils blocking flow/may lead to hydrocephalus
|
|
|
From which primitive layer do limbs develop from?
|
Somatic mesoderm (aslo Wolfian ridge also contributes)
|
|
|
Which growth factor simulates initial limb bud formation?
|
FGF 10
|
|
|
Where does the apical ectoderm ridge develop?
|
Junction between dorsal and ventral mesoderm.
|
|
|
In limb development, where is the progress zone located?
|
underlying the AER (induced to develop by fgfs 2,4,8)
|
|
|
Cells that first leave the progress zone form _______.
|
Upper skeletal parts.
|
|
|
What factor is responsible for interdigital apoptosis?
|
BMP
|
|
|
Preaxial side is the side where the ______ is.
|
thumb (also called cranial side)
|
|
|
In relative terms, where is the zone of polarizing activity located in healthy limb development ?
|
postaxial
|
|
|
There is going to be higher concentration of Shh near the _________ during limb development.
|
zone of polarizing activity (will induce development of little toe/pinky)
|
|
|
Explain the role of TF/GF responsible for deciding the dorsal/ventral nature of limb development.
|
@ dorsal side:wnt7a->lmx->mesoderm dorsalized
@ventral side: ENGRAILED supresses wnt7a in ventral side, but it won't reach dorsal side of limb bud |
|
|
T/F:Muscle in limbs develops from the hypaxial part of myotome and not the limb bud.
|
true
|
|
|
What is responsible for amniotic band syndrome?
|
Ring stricture due to amniotic membrane being torn and wraps around the limb.
|
|
|
When do the frontonasal process and pharyngel arches appear?
|
Start of the 4th week @ oropharyngeal membrane (prochordal plate same thing, mouth develops from it).
|
|
|
What is responsible for prominence formation?
|
1) Growth of mesoderm
2) Migration of neural crest cells. |
|
|
Bone & conn tissue of the face, sens & autonomic ganglia of head and neck are formed from which cell type?
|
Neural crest cells.
|
|
|
List the nerves associated with the 1st four pharyngeal arches.
|
1) trigeminal
2) facial 3) glossopharyngeal 4) vagus |
|
|
The first pharyngeal arch and the frontonasal prominence give rise to ______ and ______.
|
Face and palate.
|
|
|
Maxillary and mandibulary prominence arise from ________.
|
The first pharyngeal arch
|
|
|
The opthalmic div of trigeminal nerve grows into which part of developing embryo?
|
The frontonasal prominence.
|
|
|
What is stomatodeum?
|
Pit formed by the sinking of the oropharyngeal membrane. In 4th week the membrane disappears, and the stomatodeum forms into the pharynx.
|
|
|
What separates the olfactory pit from the oral cavity?
|
oronasal membrane
|
|
|
Merge of the medial nasal prominences gives rise to which 2 structures?
|
philthum and primary palate
|
|
|
Which 2 structures come together to form the continuous upper lip?
|
Medial nasal prom. and the maxillary prom.
|
|
|
Describe the position of the nasolacrimal duct?
|
It formed from the ectoderm underlying the nasolacrimal groove (btwn lat nasal prom and maxill. prom), and it connect the lacrimal sac with the inferior meatus of the nasal cavity.
|
|
|
The forehead, nasal bridge & nasal septum develop from which primitive structure?
What about the ala of the nose? |
The frontonasal prom.
Lateral nasal prom. |
|
|
Fusion of which 2 structures is responsible for setting the mouth width?
|
Maxillary and mandibular promininences. If they dont fuse you get macrostomia.
|
|
|
What is responsible for the unilateral clefting defect?
What about the bilateral clefting defect? |
max prom didnt fuse with the medial prom
-same but on both sides |
|
|
What are the 2 main sources of palate development?
|
1)medial nasal prom form the prim palate.
2) palattal process (appear in 6th week) of maxilla forms the secondary palate & uvula |
|
|
true/false: cleft palat is more common in girls.
true/false: cleft lip is more common in girls. |
True.
False. |
|
|
From which pharyngeal arch do common carotids develop?
Which arch is responsible for development of the aortic arch? Right subcalvian? |
3rd arch.
Left 4th pharyngeal arch. Right 4th. (6th arch gives rise to the pulm arteries, left one gives rise to ductus arteriosum). |
|
|
From which arch does incus and malleus develop from?
|
1st arch (meckel's cart).
|
|
|
Muscles of facial expression develop from which pharyngeal arch?
What about muscles of larynx and pharynx? |
2nd.
4th-6th. |
|
|
A patient has a non-malignant cyst in the neck. Can you suggest a possible embryological explanation?
|
Non-transient cervical sinus which forms as a result of growth of 2nd pharyngeal arch.
First pharyngeal groove becomes the auditory meatus. |
|
|
What contributes to ear drum formation.
|
First pharngeal pouch endoderm and ectoderm of the first groove
|
|
|
Palatine tonsils develop from _________.
|
The second pharyngeal pouch.
|
|
|
Ventral part of the 3rd phar. pouch becomes ______, while the dorsal part becomes _______.
|
thymus, inf parathyroids
|
|
|
Where does the thyoid gland develop?
|
Between 1st and 2nd pharyngeal arches, as an endoderm invagination
|
|
|
The parathymal lobe of thyroid is a remnant of which structure?
|
thyroglossal duct (as opposed to cervical sinus cyst, this is a medial neck growth, instead of lateral)
|
|
|
T/F: neurohypophysis develops from the stomatodeum.
|
false (that would be adenohypophisis), it develops as an outgrowth of the hypothalamus.
|
|
|
What is Rathke's pouch?
|
Invagination of the stomadeum ectoderm that will form the adenohypophysis.
Accessory adenohypophyseal tissue is due to remnants of the Rathke's pouch. |
|
|
Anterior 2/3 of tongue develop from ______ (innervated by ______).
Posterior 1/3? |
1st phar. arch , trigeminal nerve
From arches 3 & 4 (innervated by IX glossopharyngeal & vagus) Musculature of the tongue: somite migration from the occipital(hypoglossal region). |
|
|
What part of the somites do crest cells avoid?
|
Caudal
|
|
|
What is Spina Bifida Occulta?
|
- Asymptomatic type of Spina Bifida
- Neural arch on a vertebrae has not closed - Vertebral defect, not neural tube defect |
|
|
What is Meningocele?
|
- Vertebral defect
- Neural arch on many continuous vertebra are not closes - Meninges can herniate through and form CSF filled cyst |
|
|
What is Meningomyelocele?
|
- Same as Meningocele except it is more serious since spinal cord also herniates into the sac of meninges
- Damage to nerve roots leads to sensory/motor defects |
|
|
What is Myeloschisis?
|
- Caudal part of neural tube does not close
- Neural plate is exposed to amniotic cavity - No neural arches - Neural plate defect, not vertebral defect |
|
|
What is myelomeningocele?
|
Same as Myeloschisis except now you have CSF elevating neural plate into a cyst
|
|
|
What is hydrocephalus?
|
- CSF build up in brain ventricles
- Often found in people with myeloschisis - Requires shunting |
|
|
What is Arnold Chiari Malformation?
|
- Cerebellum and brain stem downshift into the foramen magnum
- CSF build up in ventricles - Often found in people with myeloschisis |
|
|
Is the vaginal canal derived from mesoderm, ectoderm, or endoderm?
|
Combination of mesoderm and endoderm
|
|
|
Is the uterus derived from mesoderm, ectoderm, or endoderm?
|
Mesoderm
|
|
|
Is the male urethra derived from mesoder, ectoderm, or endoderm?
|
Combination of endoderm and ectoderm
|
|
|
Are the gonads derived from mesoder, ectoderm or endoderm?
|
Mesoderm
|
|
|
In females, what does the gubernaculum become?
|
The round ligament of the uterus and the suspensory ligament of the ovary
|

