![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
CP: Rapid EKG interpretation |
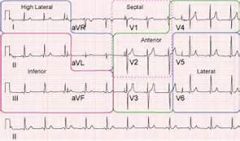
STEMI: 1mm elevation in 2 contiguous leads
Rhythm: P before every QRS (sinus) Axis: if upright in I and AVF, nl!
Ischemia: - flipped T waves: can be ischemia - elevations: infarction - depression: infarction opposite of that lead
|
|
|
CP: history |
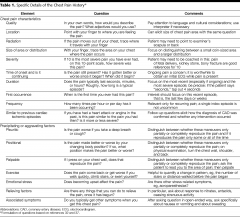
associated s/s: N/V, diaphoresis, abdominal pain or back pain, syncope
similar to previous pain or MI?
Past hx: HTN, hyperlipidemia, MI, CHF, echo with EF in chart?
h/o stress tests or caths: confirm if possible (negtaive cath can still have 30% occlusion)
Meds: BP meds, statins, ASA, plavix, coumadin, pradaxa (dabigatran) -> ask about viagra in case of getting nitro) |
|
|
CP: PE |
volume: volume up, down, or euvolemic CV/Lungs: murmurs? wet lungs or wheezing? Abdominal and back exam: palpable AAA? Legs: edema or swelling? pulses: asymmetric deficits suggest a dissection |
|
|
CP: differential |
PET MAC:
PE Esophageal rupture, Tension PTX MI Aortic dissection Cardiac tamponade |
|
|
CP: workup |
Every patient: CXR and EKG -> chest pain + suspicious EKG (ST elevation or new LBB (widened qrs))
CXR: PTX, dissection (about 60-70% sensitive), esophageal rupture
Labs: CBC (anemia), Chem10 (electrolyte abnormalities), Coags (baseline), Cardiac Enzymes (troponin, CK) |
|
|
CP: treatments |
1) ASA 325mg PO 2) nitroglycerin (0.4mg sublingual q5 min x 3 total dose, holdsystolic BP < 100 or pain free, contraindicated with viagra, cialis, etc.) -> have an IV in place before giving nitro, if hypotensive usually fluid responsive to 500c NS bolus, avoid nitro in posterior MIs.
3) if pain refractory to above, morphine and zofran
4) get a pain free EKG!!! make sure no changes
5) if patient has persistent pain despite interventions, consider unstable angina and admission to CCU instead of tele floor |
|
|
CP: pulmonary embolism risk factors, PEARL, w/u, PEARL |
Symptoms- pleuritic chest pain, SOB, tachycardia, tachypnea, hypoxia Risk factors- OCPs, pregnancy, trauma, recent surgery, malignancy PEARL- Therapeutic INR (2-3) is NOT 100% protective against PE Workup- EKG and CXR CBC (low yield but consultants want it) Chem 10 (creatinine for a CT) Coags (baseline) PEARL- DON’T indiscriminately order D-dimers |
|
|
CP: pulmonary embolus decision making |
Decision making in PE First step- Gestalt (“gut feeling”) Low probability- no workup or proceed to PERC criteria below Moderate or high probability- CT pulmonary angiogram (CTPA)
PERC criteria- low risk gestalt PLUS all of the following- BREATHS Blood in sputum (hemoptysis) Room air sat <95% Estrogen or OCP use Age >50 years old Thrombosis (in past or current suspicion of DVT) Heart rate >100 documented at ANY time Surgery in last 4 weeks
|
|
|
CP: pulmonary embolus -> treatment |
If negative- no testing (risk of PE 1.8%, risk of anti-coagulation 2%) If positive- if negative D-dimer- no further testing, if positive- CTPA
Treatment If you diagnose a PE- get cardiac enzymes and BNP for risk stratification Regular PE (vitals stable, no elevation in cardiac enzymes or BNP)- lovenox (enoxaparin) 1mg/kg SQ, admit Submassive PE (vitals stable with elevation in CEs or BNP, right heart strain on echo)- lovenox 1 (enoxaparin) mg/kg SQ, strongly consider ICU admit Massive PE (unstable vitals, systolic BP less than 90 at any time)- thombolytics and ICU admit, ?interventional radiology intervention |
|
|
CP: esophageal rupture -> hx, dx, tx |
History- recent forceful vomiting, recent endoscopy, alcoholic, sick and toxic looking patient Chest x-ray- Free air under diaphragm, rigid abdomen on exam Treatment- resuscitation, surgical intervention |
|
|
CP: aortic dissection -> pearl, risk factors, exam, dx, testing |
Aortic dissection - ripping or tearing chest that goes into the back or shoulder area PEARL- Chest pain + motor or neuro deficit OR chest pain but a seemingly unrelated complaint elsewhere in the body- think about dissection- aorta connects them both Risk factors- HTN (#1), pregnancy, connective tissue diseases (Marfan’s and Ehler-Danlos) Exam- unequal BPs (more than 20 mmHg, 60-70% sensitive), pulse deficits (20% sensitive) Chest x-ray- widened mediastinum (60-70% sensitive) Testing- CT Aorta with contrast, TEE if dye allergy or creatinine elevated, cardiac MRI
|
|
|
Abdominal Pain: history, female considerations, medical hx |
History Look at the triage note and vitals and address them Before talking the patient- look at them as they sit on the stretcher Appendicitis- usually want to remain very still Kidney stones- usually writhing, can’t get comfortable OPQRST questions about pain Onset, Provocation, Quality, Radiation, Severity, and Time Associated signs and symptoms Nausea/vomiting/diarrhea, back pain, urinary symptoms Female patients Missed periods, vaginal bleeding, discharge PO intake Relation of pain to food intake, worse pain with movement? Medical history Special attention to surgical history, previous colonoscopy |
|
|
Abdominal Pain: exam |
Don’t dive for the abdomen- do an HEENT exam, heart/lung exam Uncover the abdomen and ask patient to point where it hurts the most Check bowel sounds first Can press down with stethoscope to see if they are tender Start pressing opposite of where they have pain Start lightly and presser harder If they have trouble relaxing, bend knees to 45 degrees Peritoneal signs- usually indicate appendicitis or other surgical pathology Lightly shake stretcher- for kids- have them jump up and down All of these signs are positive if increased pain in RLQ Psoas sign- roll onto left side, extend leg back Obturator sign- flex and externally rotate right leg Rovsing’s sign- push in LLQ, pain in RLQ Reverse Rovsing’s- push in RLQ, pain in LLQ (diverticulitis) Murphy’s sign- patient takes a deep breath, push in RUQ, positive if patient stops inhaling due to pain PEARL- Do a testicular exam in all males- don’t miss a torsion! |
|
|
Abdominal Pain: workup |
Labs- not everyone needs them but if you think it’s surgical abdominal pain, get them (reasons for getting them in parentheses)
UA/HCG for females (no culture unless you admit or treat for UTI) CBC (consultants want them, up to 30% of appys have normal WBC) Chem 10 (hypokalemia can cause an ileus, low bicarb= acidosis, creatinine for a CT) Coags (standard pre-op lab, liver disease elevates coags before LFTs) LFTs (cholecysitis workups, may not need them for an appy) Lipase (pancreatitis, amylase is unnecessary- not sensitive or specific) VBG with lactate (for older patients, high lactate = bad disease) |
|
|
Abdominal Pain: pain control |
Pain control- don’t withhold it! Morphine 0.1mg/kg IV, most start with 4-6mg IV though. Write PRNs if you can. Give Zofran (ondansetron) 8mg IV to counteract nausea/vomiting. Benadryl (diphenhydramine) 25mg IV PRN for itching
PEARL- Demerol (meperedine) is a poor choice of opiate to use. It has lots of side effects and causes lots of euphoria. It doesn’t cause clinically significant sphincter of oddi spasm- that is a myth, there’s really no reason to use it all. Morphine, fentanyl and dilaudid (hydromorphone) are all excellent painkillers
Give IV fluids- younger people 1-2 liters, older patients- 500cc at a time |
|
|
Abdominal Pain: differential dx |
Appendicitis Cholecystitis Pancreatitis Diverticulitis Bowel obstruction Bowel perforation Mesenteric ischemia Kidney stone Gastritis Gastroenteritis AAA |
|
|
Abdominal Pain: imaging according to pain distribution |
How to image the abdomen effectively by quadrants (female specific causes excluded!) (CT A/P= CT abdomen and pelvis)
LUQ abdominal pain- rarely requires imaging unless you have a rigid abdomen or suspect a bowel obstruction
Epigastric- rarely requires imaging. May get it for pancreatitis to check for pseudocyst but probably doesn’t need it in the ED. If you find pancreatitis, check a RUQ US for gallstone pancreatitis
RUQ pain- RUQ US is the best test for cholecystitis
RLQ pain- CT A/P for appendicitis. Can be done without contrast with same results, some institutions require PO and/or IV contrast
Suprapubic- in isolation- usually a UTI
LLQ pain- CT A/P for diverticulitis, once again +/- IV and or PO contrast
Flank pain- CT A/P without contrast for kidney stones, CVA tenderness PEARL: 20-30% of patients with stones have NO hematuria on UA
|
|
|
Abdominal pain: mesenteric ischemia |
Mesenteric ischemia- clot thrown into mesentery or low flow state, Classically an older patient with a-fib with pain out of proportion (patient in lots of pain but not tender on exam). Low flow mesenteric ischemia is usually a hypotensive patient on pressors in the ICU. Diagnosed with CT angiogram A/P. Need emergent surgery and/or interventional radiology
|
|
|
Abdominal pain: bowel obstruction |
Bowel obstruction- patient with multiple abdominal surgeries, diffuse abdominal pain and vomiting as their chief complaint. Diagnosed with CT A/P, PO contrast is helpful
|
|
|
Abdominal pain: bowel perforation |
Bowel perforation- usually from a perfed ulcer or recent colonoscopy- be concerned if they have a rigid abdomen. Upright Chest x-ray can be helpful if you see free air, need the OR emergently
|
|
|
Abdominal pain: AAA |
AAA- back pain, abdominal pain, syncope, hematuria among other presentations, elderly patient with HTN, use ultrasound to diagnose at bedside- over 5cm needs the OR immediately, 2-5cm needs followup |
|
|
Abdominal pain: everything looks negative but concerning abdominal exam |
surgery consult! (nothing is 100%) |
|
|
D/c instructions abdominal pain: |
Discharge instructions for abdominal pain Document a repeat abdominal exam before discharge Sample discharge conversation with the patient:
I think you have a GI bug. These usually get better on their own but we can make you feel better with zofran so that you can keep fluids down. However, I have been fooled before and sometimes early appendicitis presents like a GI bug. So if you go home and have increased pain, if you are vomiting constantly despite the zofran, if you develop new pain or it moves to your right lower abdomen, or if anything else is concerning you, please come back into the ER. Also, if you don’t feel better in 12-24 hours, you should come back in as well.
PEARL- don’t discharge your patients with an excessive number of anti-emetics. If they are taking zofran or Phenergan every 6 hours and they aren’t better they need to come back to the ED, 5 tablets or ODTs is usually sufficient
|
|
|
Female Abdominal Exam: history |
History First question- is the patient pregnant? -Urine HCG and UA often done from triage -If delay in getting urine, get an IV and check a serum qualitative HCG OPQRST questions about pain Onset, Provocation, Quality, Radiation, Severity, and Time Associated signs and symptoms Nausea/vomiting/diarrhea, back pain, urinary symptoms Female specific questions Missed periods, vaginal bleeding, discharge Gs and Ps G= Pregnancies P= Live births- know them for OB consultation Medical history Special attention to surgical history, history of ectopic pregnancies or spontaneous/elective abortions Sexual history Is the patient sexually active currently or in the past? (Kick parents out of room for younger patient) Monogamous relationship? History or concern for STDs?
|
|
|
Female Abdominal Exam: Exam |
Exam Don’t dive for the abdomen- do an HEENT exam, heart/lung exam Uncover the abdomen and ask patient to point where it hurts the most Top of iliac crest- more often abdominal cause of pain Lower towards inguinal ligament- pelvic pathology Not absolute but can help you guide your workup
|
|
|
Female Abdominal Exam: Differential dx |
Differential Diagnosis Ectopic Pregnancy Threatened abortion/miscarriage Normal pregnancy STDs- Gonorrhea, Chlaymdia, Trichomonas Pelvic Inflammatory Disease Tubo-Ovarian abscess Ovarian Torsion Ovarian Cyst Bacterial Vaginosis Vaginal Candiadiasis (BV and Candiadiasis don’t cause pain but are frequently encountered in the workup) |
|
|
Female Abdominal Exam: workup |
Workup UA and HCG (looking for UTI, pregnancy status) CBC (check for WBC- low yield and anemia) Chem 10 (standard part of abdominal pain workup) LFTs Lipase Coags (these may not be necessary in every patient- let your clinical judgement be your guide but appy often overlaps with pelvic pathology) Pelvic Exam GC/Chlaymdia Wet Prep/KOH Quantitative HCG (if the patient is pregnant)
|
|
|
Female Abdominal Exam: pelvic exam tips |
Pelvic Exam tips
Do an external exam to look for lesions or obvious discharge As you insert the speculum, examine for lesions or discharge GC and Chlamydia swab- insert in cervix and twist 360 degrees Wet Prep/KOH- swab vaginal walls Bimanual exam Touching the cervix is uncomfortable- do this slowly Say to the patient “I know this is uncomfortable but does this hurt when I move my fingers” and look for reaction. If the patient seems comfortable this is NOT cervical motion tenderness If the patient is in a lot of distress, then this is CMT Check the adnexa Palpate the abdomen while checking adnexa to see where the patient has the most pain
|
|
|
Female Abdominal Exam: imaging |
PEARL- HUGE overlap between pelvic and abdominal pathology- keep your differential open
Transvaginal Pelvic ultrasound- helpful in suspected ectopic pregnancy (covered in a later podcast). Should see IUP at HCG of approximately 1,500
|
|
|
Female Abdominal Exam: Ovarian Torsion |
Ovarian Torsion- “Classic”- Sudden onset of sharp stabbing pain in lower abdomen with nausea or vomiting. PEARL- A negative pelvic ultrasound DOES NOT rule out torsion Intermittent torsion is possible Time sensitive diagnosis- ovary salvage rate greatly declines after 4 hours High suspicion= OB/GYN consult and admission for observation Most torsions have large cysts but not all PEARL- If radiologist doesn’t want to do TVUS after hours because “an ultrasound doesn’t rule out torsion”, say you are concerned for tubo-ovarian abscess or large hemorrhagic cyst |
|
|
Female Abdominal Exam: Ovarian cyst |
Ovarian Cyst- Cyst on same side as pain with good blood flow to ovary Can be discharged with pain control, OB/GYN followup
|
|
|
Female Abdominal Exam: STDs |
STDs Treatment depends on how fast your GC/Chlamydia test is Send-out = Empirically treat all patients with discharge and/or CMT PEARL- ALWAYS treat for gonorrhea and chlamydia (Often co-exist and missing it can have long term fertility consequences)
Cervicitis treatment (no CMT but positive swab) Ceftriaxone 125mg IM 1 gram of azithromycin PO x1 dose (PCN or cephalosporin allergic- 2 grams azithromycin PO x1) PID treatment (CMT and/or discharge) Ceftriaxone 250mg IM Doxycycline 100mg PO BID for 14 days
PEARL- Admit patients who are ill appearing, pregnant, unresponsive to outpatient treatment, PO intolerant Caution patient to not have sex for seven days after treatment stopped and to get partner tested to avoid re-infection |
|
|
Female Abdominal Exam: Fitz-Hugh Curtis |
Fitz-Hugh Curtis- PID infection that has spread to the liver capsule and causes perihepatitis- may have RUQ pain and tenderness, right shoulder pain. LFTs may be elevated but not always. Treatment is to treat for PID
|
|
|
Female Abdominal Exam: tubo-ovarian abscess |
Tubo-Ovarian Abscess- non-specific symptoms- abdominal/pelvic pain, history of STDs, severe or recurrent PID. Usually untreated PID that has formed an abscess. Diagnosed with TVUS, treated with IV abx, surgical drainage
|
|
|
Female Abdominal Exam: trichomonas, BV, Candidiasis |
Trichomonas- Motile organisms on Wet Prep. Sxs- itching, discharge, dysuria dyspaurenia Tx- Flagyl (metronidazole) 2 grams PO x1 or 500mg PO BID for 7 days Treat partner as well- men are often asymptomatic No alcohol while on flagyl (disulfaram reaction = vomiting) Bacterial Vaginosis- not an STD but frequently diagnosed- overgrowth of Gardanella Vaginalis. Sxs- malodorous diascharge. Clue cells on Wet Prep Treat all symptomatic patients AND pregnant patients Tx- Flagyl (metronidazole) 2 grams PO or 500mg PO BID for 7 days Candiadiasis- “yeast infection” usually after abx. Fungal elements on Wet Prep. Treatment- Fluconazole- 150mg PO x1 or topical treatments Topical treatments can control sxs better, can use with fluconazole PEARL- with all pelvic swabs- false negatives occur so treat clinically for what you think is the most serious cause
|
|
|
Headache: history |
History- OPQRST questions Headache red flags (concerning for subarachnoid hemorrhage (SAH)) -Sudden or gradual in onset -Worst of life? (Ask patient “how does this compare to your other headaches?) -Maximal at onset (worst when it started or did it gradually get worse?) -Associated symptoms- sensitivity to light/sound, nausea/vomiting, vision changes, slurred speech, weakness, syncope, ataxia, dizziness, fever, neck pain -Previous headaches/workups- previous CT/MRIs?
DOCUMENTATION- on every headache whom I am not suspecting a SAH I write “I doubt SAH/ICH given headache is not worst of life, not maximal or sudden in onset with multiple normal neuro exams”
|
|
|
HA: neuro exam |
Cranial nerves -Pupil response, papilledema -Extraocular movements -Facial sensation -Puff out cheeks -Smile symmetry -Shrug shoulders -Turn head left and right, flex and extend Upper extremity Motor strength -Grip strength -Push towards/away while still holding grip -Pronator drift- palms up, arms at shoulders, close eyes -Positive if asymmetry or if one arm falls Fine motor and cerebellar exam -Nose to finger- have patient touch their nose then your finger -Rapid alternating movements- hands in lap, rapidly pronate/supinate -Finger movements- touch 2nd finger to thumb, move to 3rd-5th fingers -Gross sensation- check upper extremities on both sides for differences Lower extremity motor strength -Hip flexors- place hand above knee, have patient push upwards -Hip extensors- place hand under thigh, have patient push downwards -Leg extension- hold knee up, extend lower leg -Leg flexion- hold knee up, flex lower leg -Foot flexion- push “down on the gas pedal” with foot -Foot extension- push “up towards your head” with foot -Gross sensation lower extremities Gait- very important to test -Walk towards and away from you- look for instability -Walk on heels and then toes -Romberg- face away from you with palms and arms up, closes eyes, stand behind patient, swaying is ok, falling backwards is positive Reflexes- low yield in headaches but part of a full neuro exam
|
|
|
HA: differential |
Headache differential
Subarachnoid hemorrhage (SAH)- sudden onset of worst headache of life that is maximal at onset, headache with syncope, ruptured aneurysm or trauma
Bacterial meningitis/encephalitis- fever and headache, stiff neck, toxic appearing
Temporal arteritis- “Classic” presentation- 60 year old female with unilateral throbbing temporal or frontal headache with tenderness on temporal area
Carbon monoxide poisoning- cold climate with a furnace at home Tumor or mass- neuro deficit with insidious onset Subdural hematoma- spontaneous bleed in a patient on anticoagulation or an alcoholic patient without trauma, or a patient with major trauma Epidural hematoma- trauma to temporal area (middle meningeal artery), lucid interval with decompensation, blown pupil Acute angle glaucoma- older patient in a dark area then has their pupil dilated (movie theatre), non-reactive pupil Hypertensive emergency- very elevated blood pressure in the setting of end organ damage (renal failure, stroke, intracranial bleeding, MI, aortic dissection) Tension headache- most common discharge diagnosis, band-like pain that is non-pulsating and dull Migraine headache- unilateral pulsating or throbbing pain, nausea/vomiting, photo/phonophobia, visual changes/aura Cluster headache- younger male with unilateral sharp stabbing pain to the eye, associated injection and tearing, responds well to high flow oxygen
|
|
|
HA: labs |
Labs -Low yield- get a pregnancy test on females (some meds class C and D) -If doing an LP- CBC (platelets) Chem 10 (electrolytes) Coags (coagulopathy) -LP labs- cell count tubes 1 and 4, glucose/protein, gram stain/culture (if suspecting meningitis)
|
|
|
HA: imaging |
CT head without contrast- detects acute bleeds, sensitivity about 90%, current practice is that a negative head CT is followed by an LP
Lumbar Puncture (LP) Looking for xanthachromia (yellowish tinge of fluid from RBC breakdown) or elevated RBC count -Usually in the 1,000s- 10,0000s with SAH but no cutoffs have ever been defined -No cutoff below which SAH can be excluded (reported as low at 800 RBCs), “clearing” of RBCs between tubes 1 and 4 does not rule out SAH -Best if you can get RBC counts <100 but if story is concerning, may need CTA brain (with contrast) or MRI to rule out SAH |
|
|
HA: special populations |
Special populations Pediatrics- persistent vomiting, vomiting first thing in the morning may be a tumor Elderly- low threshold to CT, be aware of temporal arteritis- elevated ESR and/or CRP need high dose steroids and urgent temporal artery biopsy to confirm diagnosis (by opthomology/general surgery), don’t delay steroids
|
|
|
HA: treatment |
Treatment Compazine (prochlorperazine)- 10mg IV Benadryl (diphenhydramine) 25mg IV, can run in 1 liter of normal saline (Compazine/prochlorperazine is Class C in pregnancy) PEARL- Compazine/Benadryl proven more effective in ED patients than triptans Run this slowly to prevent akasthesia from Compazine
Reglan (metoclopramide)- 10mg IV, instead of Compazine/benadryl, class B in pregnancy
Toradol (ketorolac)- 30mg IV -Caution in older patients, those with renal failure or insufficiency -Class C in third trimester only but generally not given to any pregnant patient, -Don’t use if suspecting subarachnoid without doing CT first (anti-platelet medication) Decadon (dexamethasone)- 10mg IV- shown to reduce return rates in patients with migraine
|
|
|
Back Pain: history |
Triage note- incontinence/urinary retention? Leg weakness? Fever?
History- OPQRST about pain Pain worse at night or wakes the patient up from sleep (red flag) vs. gets worse gradually as the day goes on Numbness or tingling to groin (saddle) area? Urinary/stool retention (early sign) or incontinence (late sign) Does it feel different when you wipe yourself when you go to the bathroom? Fever, night sweats, or unintended weight loss? IV drug use?
|
|
|
Back Pain: Exam |
Exam- complete HEENT exam, heart and lungs Ask patient to point where it hurts- CVA vs. midline? Abdominal exam- tenderness? (different workup if abdominal + back pain) In males- testicular exam Sensory exam of saddle area Rectal exam- can use selectively (20 year old lifting a box probably doesn’t need it, 60 year old with incontinence does) -Check perianal sensation as well as tone Lower extremity motor exam Hip flexor- hand on knee, push up Hip Extensor- hand on posterior thigh, push down Leg flexor- hold knee up, hand on lower leg, push up Leg Extensor- hold knee up, hand on calf, push down Ankle extensor- hand on bottom of foot, “push down on the gas” Ankle flexor- hand on the top of foot, push up towards the head
Lower extremity sensory exam- check sensation on both sides Straight leg raise test- patient on their back, with straight leg, raise it to 30 to 70 degrees, if pain in sciatic distribution from buttocks to knees suggests a herniated disc
|
|
|
Back Pain: Differential Dx |
Abdominal Aortic Aneurysm- older patient with hypertension and new onset back pain, possibly hematuria. Use bedside ultrasound- symptomatic AAA 5cm or larger needs the OR immediately, 2 to 5 cm needs referral for followup
Aortic Dissection- can be chest and/or back pain, ripping and tearing quality to pain, most have history of hypertension
Renal colic/urolithiasis (kidney stone)- usually younger patients with sudden onset unilateral back pain with CVA tenderness, microscopic hematuria in 70-80%, usually writhing on stretcher, can’t get comfortable
Cauda Equina Syndrome- bowel or bladder retention/incontinence, sudden onset of ripping or tearing back pain, saddle anesthesia, represents an acutely herniated disc, needs an emergent MRI for diagnosis, managed emergently in the OR
Epidural abscess- IV drug user with fever and back pain, also in diabetics or patients with recent epidural injections, needs an emergent MRI for diagnosis
Tumor or mass- patients with weight loss, night sweats, back pain at night or wakes up from sleep, history of cancer, needs emergent MRI, may need emergent radiation therapy to shrink tumor burden to preserve function
Fracture- direct trauma, pathologic fractures, pain in the middle of the back
Pyelonephritis- back pain and a fever with or without urinary symptoms
Abdominal pathology- a reminder that this can present with pure back pain
Zoster- older patient with dermatome distribution of pain, pain can precede vesicles by several days
Musculoskeletal sprain/strain- diagnosis of exclusion once the above have been addressed, most common discharge diagnosis
|
|
|
Back Pain: most serious causes |
PEARL- Major serious causes of back pain- CRAFTI
Cauda Equina Renal Aorta (aneurysm or dissection) Fracture Infection
|
|
|
Back Pain: Workup |
Labs- usually low yield
UA- low threshold especially in female patients (UTI) CBC/Chem 10/ type and cross for 8 units/emergency release blood- if suspecting AAA ESR/CRP- elevated in epidural abscess
Imaging
Bedside ultrasound- for AAA- if larger than 5 cm and symptomatic = OR STAT CT Aorta with contrast- if suspecting aortic dissection CT Abdomen/Pelvis without contrast- if suspecting kidney stone Plain films- generally low yield
American College of Radiology guidelines for plain films
Recent significant trauma or milder trauma age >50 Unexplained weight loss Unexplained fever Immunosuppression History of cancer IV drug use Osteoporosis Prolonged use of steroids Age >70 Focal neuro deficit or disabling symptoms Duration greater than 6 weeks
Emergent MRI- needed for diagnosis of cauda equina, epidural abscess, tumor
Post-void residual- useful in diagnosis of cauda equina- ask the patient to urinate then insert urinary catheter, normal is less than 100 cc Bedside ultrasound post void residual- ultrasound the bladder in transverse plane (indicator to the right), use the calculation function (sonosite) for volume, get maximal horizontal and vertical measurements, hit “save calc”, turn the probe 90 degrees (indicator towards the head) and measure largest depth, hit “save calc”, sonosite will calculate volume
Diagnostic philosophy- assume a serious cause, do a good history, physical, and exam and check for red flags, if not concerning, try to talk yourself into a serious cause, if you can’t then you can end workup
|
|
|
Back Pain: treatment |
Toradol (ketorolac)- 30mg IV, caution in older patients and those with renal failure/insufficiency
Morphine- 0.1 mg/kg IV is a good starting dose, zofran (ondansetron) IV as needed for nausea/vomiting, be sure the patient has a ride
Vicodin (hydrocodone/acetaminophen)- discharge medication, 1-2 tabs q4-6 hours PRN, no more than 15 tablets
Flexeril (cyclobenzaprine)- analgesia and sedation 5- 10mg PO three times per day
Valium (diazepam)- 5mg PO three times per day, don’t take within 4 hours of vicodin, can use at night for sleep
PEARL- If you are prescribing sedating medications or opiates, tell the patient not to drive or drink alcohol while using these medications, document on their chart (sedation warnings given)
|

