![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
What are the conducting cells?
|
SA and AV node cells; atrial internodal tracts, bundle of His and Purkinje system cells
|
|
|
What are contractile cells?
|
Bulk of cardiac wall; interconnected through gap junctions
|
|
|
What is the SA node?
|
The source of the initial electrical impulse and accounts for "normal" sinus rhythm
The pacemaker of the heart |
|
|
What is overdrive suppression?
|
The SA node preempts and thus suppresses all other conducting cells from spontaneously firing
|
|
|
What effect does forcing a cell to depolarize more often than its intrinsic discharge rate have on automaticity?
|
Decreases automaticity
|
|
|
What causes depolarization of the right and left atrium?
|
The depolarizing wave from the SA node spreading to the internodal/interatrial fibers
|
|
|
Why can't electrical impulses freely pass from the atria to the ventricles?
|
B/c the annulus fibrosis blocks their propagation
|
|
|
What is the only way the depolarizing wave can reach the ventricles?
|
By passing through the AV node on the atrial side of the annulus fibrosus
|
|
|
What is the importance of the electrical delay that is caused by forcing the depolarization wave to pass through the AV node?
|
Permits atrial contraction before ventricular contraction begins, optimizing ventricular filling time
|
|
|
What region of the heart does the depolarization wave enter after leaving the AV node?
|
The bundle of His
|
|
|
What allows the electrical stimulus to pass from the atrium to the ventricle by penetrating the annulus fibrosus?
|
The bundle of His
|
|
|
What does the depolarization wave enter after leaving the bundle of his?
|
the Purkinje fibers
|
|
|
Where in the heart is conduction slowest? fastest?
|
Slowest in the AV node
Fastest through the Purkinje fibers |
|
|
What is automaticity?
|
The ability of a cell to generate its own action potential
|
|
|
What is rhythmicity?
|
The ability to generate these potentials in a regular repetitive manner
|
|
|
What structure allows the heart to behave as a functional syncytium? (as if it were one large cell)
|
Gap junctions
|
|
|
Where does the fast response action potential occur?
|
In normal atrial and ventricular cardiomyocytes and specialized conducting fibers (Purkinje fibers)
|
|
|
Where does the slow response action potential occur?
|
SA and AV nodes
|
|
|
What is phase zero of the cardiac AP? what channels open? what ions move?
|
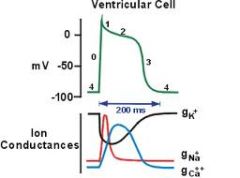
"fast upstroke"
Nav channels open! Leading to an influx of Calcium |
|
|
What is phase 1 of the cardiac AP? what channels open/close? what ions move?
|
"partial repolarization"
Nav channels inactivate, rapid opening and closing of Kv channels. Initial efflux of K+ out of the cell accounts for partial repolarization |
|
|
What accounts for the partial repolarization in a cardiac AP after phase 0?
|
Opening of Kv channels
|
|
|
What is phase 2 of the cardiac AP? what channels open/close? what ions move?
|
"plateau"
Results from opening of Cav channels, allowing influx of Ca, counterbalanced by slow efflux of K through Kv channels |
|
|
What is phase 3 of the cardiac AP? what channels open/close? what ions move?
|
"repolarization"
Due to inactivation of Cav channels and efflux of K via Kv channels |
|
|
What corrects the excess Na inside the cell, and excess K outside the cell?
|
The Na/K ATPase
|
|
|
What is phase 4 of the cardiac AP? what channels open/close? what ions move?
|
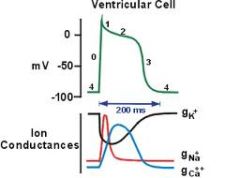
"resting membrane potential"
Characterized by background Na influx and K efflux through K leak channels (Kir channels) |
|
|
What precedes phase 0 of the cardiac AP?
|
A suprathreshold stimulus from a pacemaker cell that abruptly changes the resting membrane potential to a critical threshold value ~-65mV
|
|
|
What gates control Na influx?
|
The activation gate which is closed at rest but opens w/ depolarization
The inactivation gate which is open at rest but has a delayed closure from depolarization |
|
|
Do Ca channels only open on phase 2 of the cardiac AP?
|
No a small Ca influx begins at ~-50mV as a result of cell depolarization
|
|
|
What is the purpose of the fast-response AP in atrial and ventricular cardiac muscle?
|
AP leads to calcium influx and contraction of cardiac muscle cells
|
|
|
What is the sequence of excitation-contraction coupling?
|
Calcium enters cell => Ca binds to troponin C => Troponin C interacts w/ tropomyosin => tropomyosin shifts exposing the actin and myosin active sites => cross-bridge cycling => contraction
|
|
|
What happens if K efflux exceeds Ca influx during phase 2 of the cardiac AP?
|
Plateau duration will be short and final repolarization begins early
|
|
|
What is the importance of L-type Ca channels?
|
Ca channels are voltage-regulated time-dependent channels that activate and inactivate slowly making a current that is long lasting
|
|
|
What is the effective refractory period?
|
Similar to absolute refractory period in nerve/skeletal muscle; cell will not respond to any electrical stimulus
|
|
|
What is the relative refractory period?
|
SOME sodium channels are excitable (inactivation gates have opened) allowing a large electrical stimulus to produce an AP but a smaller one than usual
|
|
|
What is the importance of the "refractoriness" of the heart?
|
Provides the heart w/ a measure of electrical safety b/c it prevents extraneous pacemakers from triggering ectopic beats
|
|
|
What phase of the cardiac AP is responsible for the diastolic potential or pacemaker potential of the cardiac cell?
|
phase 4
|
|
|
What ions are moving during phase 4 of the cardiac AP?
|
1. Decreasing potassium efflux: due to inactivation of Kv channels
2. Increasing sodium influx: Sodium enters cell through HCN cation channel 3. Spontaneous local Ca release from the SRER 4. Increased Ca influx as membrane passes -50mV |
|
|
What is the effect of a combined increase in sodium influx and a decrease in potassium efflux?
|
A gradual depolarization of the membrane during phase 4 of the AP
|
|
|
What phase of the cardiac AP does the HCN channel open at?
|
early phase 4
|
|
|
What channel opens at -50mV of the cardiac AP?
|
L-type Calcium channels
|
|
|
What channels contribute to the upstroke of phase 0 of the SA AP?
|
L-type Ca channels
|
|
|
Why is the upstroke in the SA AP slower than the normal upstroke?
|
B/c the inward current source is calcium
|
|
|
What channel do SA and AV node cell membranes lack?
|
fast-response voltage-gated sodium channels
|
|
|
What will diminish the slow of phase zero and amplitude of the AP?
|
Low extracellular calcium or presence of calcium channel antagonists
|
|
|
What are the differences b/e the slow and fast response APs?
|
1. unstable phase 4 (early and late diastolic phase)
2. slower upstroke in phase 0 b/c inward ion is Ca 3. Absent phase 1: no early repolarization 4. Absent phase 2: no plateau due to early activation of Kv channels => early repolarization leading to an AP of shorter duration |
|
|
Why is there no plateau in slow response APs?
|
B/c of early activation of Kv channels
|
|
|
What effect does binding of epinephrine/norepinephrine to beta-1 adrenergic receptors have?
|
Increases the heart rate by activating adenylyl cyclase and increasing intracellular [cAMP]
|
|
|
What does cAMP do?
|
Phosphorylates cAMP dependent protein kinase which phosphorylates HCN and voltage-gated calcium channels, increasing their "open probability"
|
|
|
What is the effect of phosphorylation of HCN and Cav channels?
|
1. Increases sodium influx through HCN channels (I-f), increasing the steepness of the phase 4 pacemaker potential
2. Increases Calcium influx through Cav channels, which steepens phase 4 pacemaker potential |
|
|
What is the effect of ACh binding to M2 cholinergic receptors?
|
Decreases HR by inhibiting adenylyl cyclase/cAMP
1. Decreased sodium influx through HCN channels, which reduces steepness of phase 4 2. Decreased calcium influx through voltage-gated Ca channels |
|
|
What opens the GIRK channel?
|
ACh opens the G-protein activated inwardly rectifying potassium channel
|
|
|
What effect does opening of the GIRK channel have?
|
Increases potassium efflux during phase 3 and 4 of the AP => hyperpolarization of phase 4 pacemaker potential => increases time required to reach threshold
|
|
|
What are the two effects of catecholamine stimulation of beta-1 adrenergic receptors on fast-response APs?
|
1. Inotropic effect
2. Lusitropic effect |
|
|
What is the inotropic effect of catecholamine stimulation of beta-1 adrenergic receptors?
|
"increased cardiac contractility"
1. Increased calcium influx through L-type Cav channels (greater CICR) 2. Increased sensitivity of SR calcium release channels to cytoplasmic calcium -> more calcium is released by the SR making more Ca available for binding of troponin 3. Enhanced SR Ca ATPase activity => increased Calcium stores for later release |
|
|
What is the lusitropic effect of catecholamine stimulation of beta-1 adrenergic receptors?
|
"Accelerated speed of ventricular and atrial muscle relaxation"
1. cAMP and PKA phosphorylate (inhibit) phospholambam 2. PKA phosphorylates Troponin I, destabilizing actin-myosin cross-bridges |
|
|
What is the function of phospholambam?
|
Inhibits SR Ca ATPase, the SR pump that returns Ca back into SR
|
|
|
What is the effect of phosphorylation of phospholambam?
|
Removes the inhibitory effects of phospholambam => pumping activity of SR Ca ATPase increases => Ca removed from intracellular space more rapidly => this accelerates the speed of cardiac muscle relaxation
|
|
|
What are the effects of beta-1 adrenergic receptor activation in the SA and AV node? atrial muscle? ventricular muscle?
|
SA/AV node: inc. conduction velocity, inc. pacemaker rate
Atrial muscle: inc. contractility Ventricular muscle: inc. contractility |
|
|
What is the effect of M2, cholinergic, receptor activation on the SA and AV node? Atrial muscle? Ventricular muscle?
|
SA/AV node: dec. conduction velocity, dec. pacemaker rate
Atrial muscle: little effect Ventricular muscle: little effect |
|
|
What causes the P wave of the EKG? how long does it last?
|
Caused by sequential activation (depolarization) of the right and left atria; lasts ~0.08s
|
|
|
What is the PR interval of the EKG?
|
The time from the beginning of the P wave to the start of the QRS complex, represents the amount of time the AP takes to travel from the SA node to the AV node
|
|
|
How will an inhibition of conduction through the AV node be reflected in a EKG?
|
A lengthening of the PR interval
|
|
|
Why is atrial repolarization not seen on an EKG?
|
B/c atrial repolarization is too slow and too diffused to register
|
|
|
Why is SA and AV node depolarization not seen on an EKG?
|
B/c of decreased nodal mass
|
|
|
What causes the QRS complex? how long does it last?
|
Right and left ventricular depolarization, ~0.1s or less
|
|
|
How will a longer QRS complex be reflected in the EKG?
|
By a longer QRS complex
|
|
|
What is the ST segment? what causes it?
|
An isoelectric segment that coincides w/ the plateau of the fast response ventricular AP and the rapid ejection phase of the cardiac cycle
|
|
|
Why is the ST segment isoelectric?
|
B/c the ventricles are uniformly depolarized
|
|
|
If a part of the myocardium is damaged how will that be reflected in an EKG?
|
A shift on the level of the ST segment
|
|
|
What does the T wave mark? why is it upright?
|
Ventricular repolarization
Upright b/c repolarization occurs in reverse sequence to depolarization |
|
|
What is the QT interval?
|
The duration of ventricular depolarization and repolarization
|
|
|
What happens to the QT interval if ventricular repolarization is delayed?
|
The QT interval is prolonged
|

