![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
174 Cards in this Set
- Front
- Back
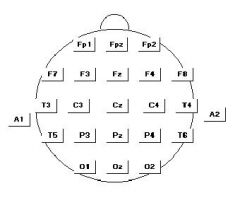
Describe the 10-20 system of electrode placement.
|
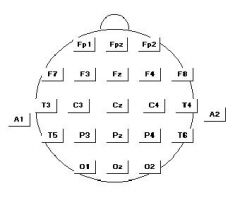
Start by finding the nasion and inion, measure 10% above those distances. Then divide the rest into 20%. Then go from anterior tragus to anterior tragus.
|
|
|
What is the localization principle for bipolar recordings?
|
Localization principal means that in each "channel" for example f8-t4 input 1 and input 2 are compared. If input 1 (in this case f8) is negative compared to input 2 there is a positive deflection and vice versa.
|
|
|
Where is C3/C4 estimated to be intracranially?
|
Rolandic sulcus
|
|
|
Where is f7/f8 estimated to be intracranially?
|
anteiror temporal/orbitofrontal
|
|
|
Where is T1/T2?
|
not a part of 10-20 system but place about 1 inch up and 1/3 of way from distance between anterior tragus and lateral canthus of the eye
|
|
|
Explain the localization principle for referential montage.
|
In referential montage all the scalp electrodes go to input 1 and then the reference (usually) ear electrode will go to input 2. The localization in referential montage is amplitude.
|
|
|
Explain the disadvantage of the bipolar montage.
|
In bipolar montage if the 2 inputs are equipotential to each other then there is no spike at all transmitted.
|
|
|
Explain the disadvantage of referential montage.
|
The ear electrode can have EKG artifact.
|
|
|
What is the standard sensitivity for EEG and when should it be adjusted?
|
7 microvolts per millimeter. Big waveforms sensitivity may need to be decreased
|
|
|
Explain what a low pass high frequency filter is.
|
This resistance/capacitance mechanism attenuates high frequency activity. Settings include 60 HZ or 70 HZ. (An inappropriate setting would be 15 HZ or 35 HZ)
|
|
|
Explain what a high pass low frequency filter is.
|
aka time constant a resistance/capacitative mechanism that filters out low frequencies. Time constant means the time for a potential to attenuate by 37%
|
|
|
What is standard low frequency high pass filter set at?
|
0.3 seconds or 1 second
|
|
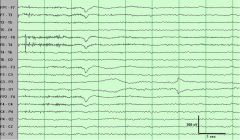
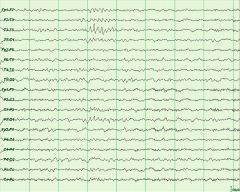
What is the abnormality in this picture?
|
The scalp electrode at P3 is not well applied, abnormal impedance is causing an electrode pop and can also causing variations in rhthym
|
|
|
What are some clues to distinguish muscle artifact and spike potentials?
|
muscle artifact is usually less than 20 msec
|
|
|
Explain what happens during an EEG during eye blinks.
|
The cornea is positive compared to the retina. Eye closure causes Bell's phenomena which leads to a net positive input 1 and a negative deflection on the EEG
|
|
|
Explain what happens during lateral eye movements.
|
The corneo-retinal potential leads to a downward spike towards the side of looking and the upward spike towards the opposite side
|
|
|
What are some other clues to lateral eye movements?
|
lateral rectus spikes
|
|
|
Explain what can happen during chewing, IV, respirators, LVAD, patting, chewing, perspriration, tongue movements, someone walking by
|
chewing-repetitive muscle artifact especially temporal
tongue movement-slow undulating movements without a potential perspiration- slow undulating movements without a potential patting- rhythmic movements walking by- rhythmic movements respirators- rhythmic LVAD- rhythmic, correlate with EKg |
|
|
What is the significance of frontal alpha?
|
considered abnormal depending on the state of patient, if comatose this is poor prognosis
|
|
|
What is the significance if differences in alpha amplitude from side to side?
|
If the difference in ratio of amplitude is less than 2:1 this is acceptable, even if greater than 2:1 could be normal ( depends on how well-organized and the location of it)
|
|
|
What percentage of individuals do not have any alpha?
|
5 %
|
|
|
What is frequency of beta activity?
|
more than 14 hertz
|
|
|
What medications may cause excessive beta?
|
beta in frontocentral regions can be caused by barbiturates, chloral hydrate, benzodiazepines and tca
|
|
|
When does spindle synchrony occur in children?
|
6 months
|
|
|
What age does hypnagoguic hypersynchrony occur?
|
age 1-6
|
|
|
Where are mu waves predominant?
|
C3/C4 central derivation
|
|
|
How are mu waves diminished
|
moving or even thinking of moving the contralateral limb.. C3/C4 motor sulcus
|
|
|
What are lambda waves?
|
positive waves occur in the occipital derivation and occur due to scanning an image in the awake state
|
|
|
What are POSTS?
|
positive occipital sharp transients of sleep occur in light to moderate levels of slee, usually bilaterally synchronous, but can be asymmetrical
|
|
|
When does REM onset occur in a normal patient?
|
90 minutes after sleep onset
|
|
|
What are some changes in the EEG for elderly patients?
|
bifrontal delta activity may occur
|
|
|
What is meant by fundamental, harmonic and subharmonic?
|
Fundamental 1:1 following
Harmonic 2:1 following response Subharmonic 1/2:1 following response |
|
|
What are some clues to slow alpha variant?
|
the posterior dominant rhythm appears theta range but with a notched morphology to the waves
|
|
|
What are some clues to fast alpha variant?
|
The posterior dominant rhythm is twice as much as the usual alpha
|
|
|
What is rhythmic mid-temporal theta activity?
|
Runs of sharply contoured theta waves, occur independently (can be unilateral), younger patients, drowsiness
|
|
|
What is rhythmic mid-temporal theta activity?
|
Runs of sharply contoured theta waves, occur independently (can be unilateral), younger patients, drowsiness
|
|
|
What is rhythmic mid-temporal theta activity?
|
Runs of sharply contoured theta waves, occur independently (can be unilateral), younger patients, drowsiness
|
|
|
What is psychomotor variant?
|
rhythmic mid-temporal theta activity
|
|
|
What is psychomotor variant?
|
rhythmic mid-temporal theta activity
|
|
|
What is psychomotor variant?
|
rhythmic mid-temporal theta activity
|
|
|
What are wicket spikes?
|
sharply contour rhythmic frequency varying from 7 to 11 HZ maximal in mid-temporal derivations
|
|
|
What are wicket spikes?
|
sharply contour rhythmic frequency varying from 7 to 11 HZ maximal in mid-temporal derivations
|
|
|
What are the characteristics of a seizure
|
Evolution with frequency, amplitude and field
|
|
|
What are the characteristics of a seizure
|
Evolution with frequency, amplitude and field
|
|
|
What are wicket spikes?
|
sharply contour rhythmic frequency varying from 7 to 11 HZ maximal in mid-temporal derivations
|
|
|
What are the characteristics of a seizure
|
Evolution with frequency, amplitude and field
|
|
|
What are the features of benign epilepsy with centrotemporal spikes?
|
diphasic, independent (unilateral or bilateral), spikes centered at C3/4 (central) or T3/4 ()mid-temporal) activated by sleep
|
|
|
What is Rolandic epilepsy?
|
specific childhood epilepsy syndrome that usually resolves by 20; sz characterized by vocalization (guttural), hemifacial spasms and characteristically during sleep
|
|
|
What is recommended treatment for Rolandic epilepsy?
|
debatable whether or not to treat, if treating use agents for partial onset epilepsy
|
|
|
What are some etiologies of FIRDA?
|
increased ICP
intoxication deep midline structural abnormality metabolic encephalopathy |
|
|
How can one distinguish between metabolic encephalopathy leading to triphasics and NCSE with triphasics?
|
The NCSE is discontinuous
|
|
|
What criteria need to be met prior to declaring an EEG electrocerebral silence?
|
1. at least 8 scalp electrodes
2. placed at least 10 cm apart 3. Impedance set between 100-10000 ohms 4. HF filter set no less than 30 HZ, LF filter set no more than 1 HZ 5. no reaction to painful, visual or auditory stimuli 6. sensitivity at 2 microvolts 7. at least 30 minute recording 8. integrity of entire system should be tested |
|
|
What are Trieman's stages of status epilepticus?
|
stage 1: electrographic ictal discharges with rapid recruitment, another sz occurs prior to recovery
stage 2: "merging" stage; spike-waves plus different frequency runs stage 3: electrographic ictal discharges stage 4: flat periods stage 5: PEDs |
|
|
What is mu rhythm?
|
Characterized by arch shaped waveform at frequency of 7-11 HZ over C3/C4 can be unilateral, independent, awake state
|
|
|
What stages of sleep do vertex waves occur?
|
drowsiness and stage 2 sleep
|
|
|
What happens on EEG when a patient looks to the left?
|
The eyes are closest to F7/F8 electrodes (orbitofrontal/anterior temporal) therefore looking to left, positive to F7 which causes a downward deflection when F7 is input 2 and an upward deflection when F7 is input 1
|
|
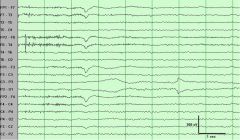
What is the abnormality in this 18 year old drowsy patient?
|
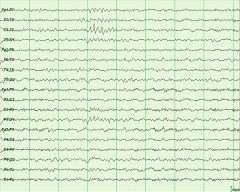
wicket temporal spikes, morphology symmetric up-going and down-going, frequency would be 7-11 hz, not aftergoing slow-wave or disruption of background to suggest sz
|
|
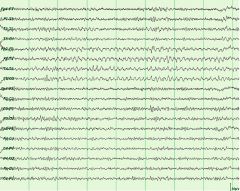
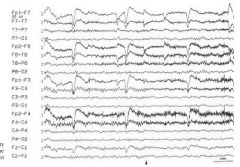
what is the abnormality in this drowsy 15 year old patient?
|
rhythmic mid-temporal theta (drowsiness/sleep) unilateral, bilateral, independent, lasts up to 10 seconds, notched, flat top or sharp appearance
|
|
|
What is the morphology of rhythmic mid-temporal theta?
|
notched, flat-top or sharp
|
|
|
When do wicket spikes occur?
|
drowsiness
|
|
|
What age does rhythmic mid-temporal theta tend to occur?
|
young adults
|
|
|
What is the usual frequency of wicket spikes?
|
7 to 11 hertz
|
|
|
What is the morphology of rhythmic mid-temporal theta?
|
notched, flat-top or sharp
|
|
|
When do wicket spikes occur?
|
drowsiness
|
|
|
What age does rhythmic mid-temporal theta tend to occur?
|
young adults
|
|
|
What is the usual frequency of wicket spikes?
|
7 to 11 hertz
|
|
|
What is the morphology of rhythmic mid-temporal theta?
|
notched, flat-top or sharp
|
|
|
When do wicket spikes occur?
|
drowsiness
|
|
|
What age does rhythmic mid-temporal theta tend to occur?
|
young adults
|
|
|
What is the usual frequency of wicket spikes?
|
7 to 11 hertz
|
|
|
What is the morphology of rhythmic mid-temporal theta?
|
notched, flat-top or sharp
|
|
|
When do wicket spikes occur?
|
drowsiness
|
|
|
What age does rhythmic mid-temporal theta tend to occur?
|
young adults
|
|
|
What is the usual frequency of wicket spikes?
|
7 to 11 hertz
|
|
What is the abnormality in this 16 year old drowsy patient's EEG?
|
Small sharp spikes, less than 50 mA, less than 50 msec duration, does nto disrupt the background
|
|
|
Would it be possible for a small sharp spike to have an aftergoing slow wave?
|
yes, which makes it a subjective call, but if it doesn't disrupt the background would not call it epileptiform
|
|
|
What are the rules that need to be broken to consider a discharge epileptiform?
|
1. Disrupt the background
2. Evolution of morphology or is it monomorphic (psychomotor) 3. Evolution of frequency 4. After-going slow wave 5. High amplitude 6. Rhythmicity |
|
|
What are some normal variants that may occur independently or asynchronously?
|
RMT theta (psychomotor)
wicket spikes mu rhythm small sharp spikes |
|
|
What are some normal variants that usually occur synchronous, asynchronous would be abnormal?
|
POSTS, sleep spindles
|
|
|
What is the photomyogenic response?
|
forehead twitching that occurs after photic stimulus
|
|
|
What age do wicket spikes occur?
|
0.9% in people over 30 years
|
|
|
Can POSTS occur independently?
|
usually synchronous
|
|
|
How can one distinguish psychomotor variant or rhythmic mid-temporal theta from seizures?
|
monomophic and monorhythmic (also morphology would be flat, notched or sharp)
|
|
|
What is sublinical rhythmic electrographic discharge of adults?
|
occurs abruptly, parietal-posterior temporal, see backgrounda ctivity, awake or hyperventiliation, symm/asymm, older adults >50 no aftergoing slowing usually theta range or mix of delta-theta; asymptomatic
|
|
|
What age are 14 and 6 positive bursts usually seen?
|
age 12-20
|
|
|
What are the features of 14 and 6 HZ positive bursts?
|
occur in posterior temporal region, during light sleep, occur independently
|
|
|
Can small sharp spikes occur as doublets or repetitive trains?
|
rarely as doublets, never as repetitive trains
|
|
|
What ge do 6 HZ spike and wave usually occur?
|
young adult
|
|
|
What are the features of 6 HZ spike and wave?
|
brief 1-2 seconds, low amplitude, brief duration spike, diffuse distribution, drowsy state, young adult, usually synchronous and symmetric without clinical correlate
|
|
|
What are F waves?
|
frontally dominant V waves
|
|
|
What side do wicket spikes occur more often on?
|
left side
|
|
|
What state do 14 and 6 positive bursts tend to occur in?
|
light sleep or drowsiness
|
|
|
What are 14 and 6 positive bursts most prominent?
|
posterior temporal
|
|
|
What percentage of patients with anterior temporal spikes have seizures?
|
90%
|
|
|
What percentage of patients with frontal spikes have seizures?
|
70%
|
|
|
What percentage of occipital spikes are associated with seizures?
|
30-50%
|
|
|
What age do Rolandic seizures usually occur?
|
4-12
|
|
|
What percentage of patients with centrotemporal spikes have seizures?
|
80%
|
|
|
What is temporal intermittent rhythmic delta activity?
|
uncommon, 0.3% of all EEGS, during drowsiness or ligjht sleep, high predictive value for TLE
|
|
|
What happens to the EEG after a stroke?
|
In first few days delta activity, After a few days either a return to normal, slowing, asymmetry or sometimes PLEDs
|
|
|
What type of tumors are more likely to produce epileptiform abnormalities on EEG?
|
slower growng tumors
|
|
|
What age does trace discontinu occur?
|
Occurs in newborns up until 30 weeks
|
|
|
What age do children get continuity during REM sleep
|
>30 weeks
|
|
|
What age do children get continuity during awake state
|
>34 weeks
|
|
|
What age do children get continuity during NREM?
|
>38 weeks
|
|
|
What age do children have trace alternans patterns?
|
38 weeks up to 6-8 weeks post-term, usually during NREM
|
|
|
What age do beta delta complexes occur?
|
26 weeks to 38 weeks, occur only in prematurity
|
|
|
How can one distinguish between different age groups based on beta delta complex activity?
|
central 26-27 weeks
29-33 weeks occipitotemporal, REM 33-38 wks NREM |
|
|
What age do temporal theta bursts appear?
|
26-33 weeks
|
|
|
When do neonates get a clear distinction between awake and asleep state?
|
36 weeks, beta delta will change to polyfrequency
|
|
|
When does reactivity occur in neonates?
|
33-34 weeks
|
|
|
When does attenuation to loud stimuli occur?
|
clear at 36 weeks, can last 8-10 seconds
|
|
|
When do frontal sharp wave transients occur?
|
34 weeks to 6-8 weeks post term, symmetric an dsynchronous
|
|
|
When is rhythmic theta or alpha considered abnormal?
|
continuous as predominant activity
|
|
|
When does 8 hertz rhthym appear in children?
|
80% of 3 year olds have 8 hertz activity
|
|
|
What frequency is posterior dominant rhthym at 1 year?
|
70% of children have at least 6 Hertz acctvity
|
|
|
What age do posterior slow waves of youth start?
|
age 2 up to 8-14 rare after 21
|
|
|
What are 6 criteria that can help distinguish posterior slow waves of youth from abnormal occipital slowing?
|
1. does not disrupt alpha
2. voltage less than 1.5 times alpha 3. not focal 4. asymmetry less than 50% 5. blocks with eye opening and drowsiness 6. random and scattered rather than rhythmic serial or continuous |
|
|
What are lambda waves?
|
asymmetric sharp, di or triphasic in occipital region, awake, attenuates with eye closure
|
|
|
What age do lambda waves occur?
|
2-13 years
|
|
|
What age do vertex transients appear in stage 1 sleep?
|
6-8 weeks, bilaterally synchronous and symmetrical when they appear
|
|
|
What are some major differences in neonatal EEG?
|
1. occipital dominant slow waves, broad high amplitude, shifting
2. spindle delta brush pattern 3. random multifocal sharp transients or focal sharp waveforms 4. anterior slow waves 5. bursts or trains of sharp-contoured theta over temporal/central vertex |
|
|
What is true about the interpretation of sharp transients in nenonates?
|
They can often be transient and non-specific when babies are stressed
|
|
|
What type of abnormality is seen in infants with intraventricular hemorrhage?
|
rolandic positive sharp waves in the EEG
|
|
|
What is the posterior dominant rhthym at age 3 months?
|
3 hertz
|
|
|
What is the posterior dominant rhthym at 1 year?
|
6 hertz
|
|
|
What is the posterior dominant rhthym at 3 years?
|
8 hertz
|
|
|
How does hyperventilation differ in older vs. younger children?
|
older children anterior head region
younger children posterior head region |
|
|
What age do sleep spindles become well-developed and bisynchronous? `
|
1-2 years of age
|
|
|
What are slow lambdas of childhood or "shut-eye waves"?
|
singkle broad and monophasic or diphasic waveforms, bilaterally over occipital head regions after eye blinks or movements
|
|
|
What is hypsarrhythmia?
|
pattern of high amplitude, multifocal spikes, sharp waves and slow waves associated with infantile spasm
|
|
|
What is charge?
|
Charge is somethign that generates an electric field around the surrounding space, charges will exert force on another charge
|
|
|
What is the relationship of force and charge?
|
F = q E
force = charge X electric field |
|
|
What is electric potential?
|
electric potential is the energy per unit charge
V(voltage)=U(energy)/q(charge) |
|
|
How is electric potential related to distance?
|
Electric potential increases when the distance the charge is being moved increases, therefore V(voltage, electric potential)=E(electric field)l(distance)
|
|
|
What is current?
|
current is numberically equal to the rte of flow of charge q, measured in amperes
|
|
|
What is the difference between conductors and insulators?
|
this is an intrinsic property of the metal or plastic and whether or nto it permits movement of positive chargs (Metal is a cnudctor, plastic is an insulator)
|
|
|
What is current density?
|
current flowing in a conductor-like a piece of wire, divided by the CSA(cross sectional area) A of that conductor J=i/A
|
|
|
What is Ohm's law?
|
Resistance is equal to rate of potential difference/current flow i (resistance is measured in ohms)
|
|
|
At what age is trace alternans considered abnormal?
|
Normal in NREM sleep from 36 to 48 weeks CA
|
|
|
What state becomes continuous first; REM, wake, NREM?
|
REM: 30 weeks
Wake: 34 weeks NREM:38 weeks |
|
|
At what age are Beta Delta complexes considered abnormal?
|
Beta delta occurs from 26 weeks to 40 weeks (term infants can have beta delta during NREM)
|
|
|
When are frontal sharp transients considered abnormal?
|
32 to 48 weeks
|
|
|
How do temporal alpha bursts date the patient?
|
32-34 weeks
|
|
|
What age would be considered abnormal not to have an ODR?
|
ODR starts at 3 months and should have by 3.5 months
|
|
|
How do the distribution and state that beta delta occurs in help date the patient?
|
Beta delta central 26-29 weeks
Beta delta occipitotemporal 29-33 weeks and during REM <33 weeks occipitotemporal during NREM |
|
|
What age do temporal theta bursts occur?
|
26 to 32 weeks
|
|
|
What is the significance of reactivity in babies?
|
There is a general attenuation that occurs due to a loud stimuli or noise at the age of 36-37 weeks
|
|
|
What is the significance of low voltage activity in a term/newborn?
|
This depends on what else is going on in the record. In and of itself, it does not necessarily signifiy an abnormality (less than 20 microvolts)
|
|
|
When is rhythmic activity considered abnormal in newborns?
|
>8-10 seconds
recurrent runs continuous voltage should be higher than the background |
|
|
What 7 features help to distinguish between an abnormal temporal sharp wave and a normal temporal sharp wave in infants?
|
1. amplitude < 75 microvolts
2. Duration > 150 msec 3. Frequency: several times per minute 4. Manner of occurence: runs, continuous 5. morphology: polyphasic 6. polarity surface positive or negative 7. state: awake, NREM and rem |
|
|
What drugs may slow the alpha rhthym without other changes on the EEG?
|
phenytoin and CBZ
|
|
|
What is considered abnormal for asymmetry in voltage side to side for children?
|
the lower voltage side is 80% of the higher voltage side in 95% of children. It should never be more than 2:1
|
|
|
What side is usually the higher voltage side on EEG?
|
Usually the right side, because for some reason the left side of the skull is thicker
|
|
|
What ages would be abnormal to have posterior slow waves of youth?
|
Less than 2 and older than 21
|
|
|
What are some features 4 that help distinguish posterior slow waves of youth from pathologic occipital slowing?
|
1. Morphology: Should not disrupt alpha
2. Amplitde: Should not be more than 1.5 times the normal alpha 3. Reactivity: Should block with eye opening or drowsiness 4: Should be symmetric or asymmetric never focal |
|
|
What are 2 features that do not help in distinguishing posterior slow waves of youth from occipital slowing?
|
Can be symmetric or asymmetric. Can be synchronous or asynchronous
|
|
|
How can one distinguish between lambda waves and pathologic occipital spikes?
|
Closing the eyes would make lambda waves disappear
|
|
|
What age does hypnagoguic hypersynchrony occur?
|
From age 3 months to 12 or 13 years (Only 10% of children after 11 have hypnagoguic hypersynchrony)
|
|
|
What age do vertex transients appear?
|
6 to 8 weeks
|
|
|
What age do vertex transients become synchronous and symmetric?
|
They should be symmetric and synchronous as soon as they appear
|
|
|
What age do sleep spindles appear in children?
|
6 to 8 weeks
|
|
|
What age do sleep spindles become symmetric?
|
6 to 8 weeks when they appear
|
|
|
What age do sleep spindles become synchronous?
|
shoul be synchronous by 1-2 years
|
|
|
When do POSTS usually appear?
|
usually 3-4 but younger <1 has been reported and maximal in mid-adolescence
|
|
|
What are some features that help distinguish POSTS from focal discharges?
|
POSTS should be synchronous, but can be asymmetric with the ratio being 40%
|
|
|
What are the features of 14 and 6 positive bursts?
|
Bursts of 14 hz or 6 hz (independent, unilateral) positive polarity activity in the posterior occipito or temporal regions during drowsiness. May occur in up to 1/2 of the population
|
|
|
What is Bancaud's phenomenon?
|
Unilateral failure of the alpha to attenuate with eye opening
|
|
|
What are the 7 classes of medications that cause beta activity?
|
1. benzodiazepines
2. barbiturates 3. chloral hydrate 4. antipsychotics 5. antihistamines 6. antidepressants 7. stimulants |
|
|
What are the features of 14 and 6 positive bursts?
|
Bursts of 14 hz or 6 hz (independent, unilateral) positive polarity activity in the posterior occipito or temporal regions during drowsiness. May occur in up to 1/2 of the population
|
|
|
When do POSTS usually appear?
|
usually 3-4 but younger <1 has been reported and maximal in mid-adolescence
|
|
|
What are some features that help distinguish POSTS from focal discharges?
|
POSTS should be synchronous, but can be asymmetric with the ratio being 40%
|
|
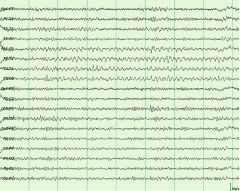
What is the significance of the right central activity seen in this tracing?
|
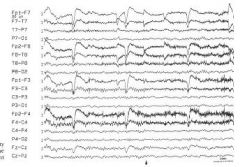
Mu (rhthym en arceau, com, wicket) occurs unilatera/asymm/asynch wakefulness attenuates with thought of moving contralateral limb, archiform, 7-12 HZ
|
|

What is the significance of the positive polarity activity seen in the posterior regions in this tracing?
|

Lambda waves, present during wakefulness (can be asynchronous,asymmetric) and attenuate with eye closure
|

