![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
182 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Lamellar bodies of type ___ pneumocytes contain ______.
|
Lamellar bodies of type II pneumocytes contain:
phospholipids--major component of surfactant! |
|
|
|
Trypsinogen:
Released from Activated by Cause of deficiency Signs of deficiency |
Released from pancreas
Activated by enterokinase/peptidase Cause of def: low enterokinase/peptidase Signs of deficiency: Diarrhea Growth retardation Hypoproteinemia |
|
|
|
HBsAg:
What does it mean? When does it appear? |
Appears before onset of syx, when patient is most ill, and then becomes undetectable in 3-6 months, unless dz progresses to chronic phase
|
|
|
|
Lipase:
Released from Cause of deficiency Signs of deficiency |
Released from pancreas (digests TGs)
Chronic pancreatitis causes low lipase Leads to steatorrhea (foul smelling bulky stools containing undigested fat) |
|
|
|
HBeAg:
What does it mean? When does it appear? |
Appears after HBsAg first appears; means active viral replication
|
|
|
|
Lactase:
Produced by Signs of deficiency |
Lactase produced by intestinal brush border (converts lactose to glucose and galactose)
Lactose intolerance |
|
|
|
HBV DNA:
What does it mean? When does it appear? |
Appears after HBsAg first appears; means active viral replication
|
|
|
|
Secretin:
Released by Effects |
Released by S cells of duodenum in response to low pH
Stimulates bicarb release from pancreas, gall bladder Reduces acid secretion in stomach by inhibiting gastrin production |
|
|
|
Anti-HBcAg IgM:
When does it appear? |
Appears shortly before symptom onset
|
|
|
|
Huntington Disease:
Presentation Age of Onset |
Movement disorder (chorea)
Aggressiveness, apathy, depression Anemia Onset in 40s-50s 100% penetrance |
|
|
|
Anti-HBcAg IgG:
When does it appear? |
Months after symptom onset
|
|
|
|
Define genetic anticipation.
|
Tendency for clinical symptoms to worsen and/or occur earlier in subsequent generations.
|
|
|
|
What determines whether HBV has high or low infectivity in a patient?
What about high or low replication? |
High infectivity if high HBeAg
Same goes for replication |
|
|
|
Define pleiotropy.
|
One gene mutation leads to multiple phenotypic abnlts
Ex: Huntington's leads to chorea, bhvrl abnlts, anemia (multiple phenotypes) |
|
|
|
Anti-HBsAg IgG:
When does it appear? |
Arises once acute disease resolves and is not detectable until week or months after HBsAg has disappeared.
May persist indefinitely, conferring lifelong immunity. |
|
|
|
CAG repeats
|
Huntington's
Increased number w/spermatogenesis (pts who receive abnl gene from dads develop dz earlier in life) |
|
|
|
What is heteroplasmy?
|
Random distribution of normal and mutated mitochondria between daughter cells leads to some cells having healthy mitochondria while other cells have mutated mitochondria.
Related to mitochondrial disease. |
|
|
|
Define genetic mosaicism.
|
Two populations of cells w/different genotypes; ex: Turner's can exist as 46XX or 45X0
or Klinefelter's as 46XY, 47XXY |
|
|
|
What disease is exclusively inherited from mothers?
|
Mitochondrial disease
|
|
|
|
Define genetic imprinting.
|
Selective inactivation of genes of either maternal or paternal origin. Ex: Prader-Willi and Angelman; both involve deletion of same gene on same chromosome, but if deletion comes from father-->Prader-Willi Syndrome (insatiable hunger, thirst, emotional lability)
Deletions from mom-->Angelman syndrome (happy puppet syndrome-->jerky movements and happy disposition) |
|
|
|
Leber hereditary optic neuropathy:
Disease type Presentation |
Mitochondrial disease (From mom)
B/L vision loss |
|
|
|
Describe stages of menstrual cycle:
Label phases and days Hormones released, effects Histologic changes |
Proliferative (Follicular) Phase - Days 1-14:
Estrogen-->proliferation of striatum functionale; nonbranching, nonbudding uniform glands; glands are tubular, narrow, pseudostratified, elongated Secretory (Luteal) Phase - Days 15-28: PG-->secretory endothelium Glands enlarge, coil, acquire cytoplasmic vacules Glycogen-rich mucus released into glandular lumen |
|
|
|
Myoclonic epilepsy with ragged-reg fibers:
Disease Type Presentation |
Mitochondrial dz (from mom)
Myoclonic seizures and myopathy assocd w/exercise Skeletal muscle bx shows irregularly shaped muscle fibers (ragged red fibers) |
|
|
|
Klinefelter's:
Presentation Karyotype Lab findings |
Klinefelter's: 47XXY
Male hypogonadism Small atrophic testes, small penis No secondary male chars (no deep voice, no bear, no male pattern pubic hair) Lab findings: Inc'd FSH, Inc'd E2, Dec'd Test |
|
|
|
Mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes:
Disease Type Presentation |
Mitochondrial disease (from mom)
Seizures Stroke-like episodes with neurologic deficit Elevated lactate levels post-exercise and at rest |
|
|
|
This determines the extent of feminization in Klinefelter's.
|
E:T ratio
|
|
|
|
What antibodies prevent reinfection with influenza?
|
Anti-hemagglutinin IgG Abs in circulaiton
Mucosal Anti-hemagglutinin IgA Abs in nasopharynx This goes for influenza type A, B, and C. |
|
|
|
These arteries arise from the root of the aorta.
What are their subdivisions? What regions of the heart do they supply? |
R and L main coronary arteries
L Main coronary--> LAD and Circumflex (anterior/lateral heart) R Main coronary--> posterior descending artery (90% of patients)--inferior wall of LV (diaphragmatic surface) |
|
|
|
DNA methyltransferase:
Role Effect |
Transfers methyl group donors (such as S-adenosyl-methionine) to cytosine residues in DNA molecule
DNA methylation can silence gene expression without affecting genetic sequence (thus altering phenotype) |
|
|
|
This artery supplies to SA and AV nodal arteries.
|
Right coronary a
|
|
|
|
What is genetic imprinting?
|
Offspring's genes expressed in parent-specific manner. Produced by DNA methylation.
|
|
|
|
E. coli:
Gram -/+ Aerobic/Anaerobic Shape |
Gram negative rod (bacillus)
Anaerobe |
|
|
|
Family history suspicious of asthma (triad).
|
Asthma
Allergic rhinitis Atopic dermatitis |
|
|
|
Virulence factor:
E coli causing neonatal meningitis |
K-1 antigen
|
|
|
|
Methacholine:
Drug class Use |
Muscarinic agonist-->bronchoconstriciton, inc'd airway secretions
Use to provoke asthma attack |
|
|
|
Virulence factor:
Enterotoxigenic E coli |
Heat labile enterotoxins (increases intracellular cAMP just like cholera)
Labile like the air--inc'd adenylate cyclase activity-->secretory diarrhea (stable like the ground--inc'd guanylate cyclase activity) |
|
|
|
Asthma:
PFT values |
Dec'd FEV1
Dec'd peak expiratory flow rate Typically reversible w/bronchodilator (albuterol) |
|
|
|
Virulence factor:
E coli causing UTI |
Fimbriae--allows for bacterial adhesion of uroepithelial cells
|
|
|
|
Scopolamine:
Drug Class Use |
Muscarinic antagonist
For motion sickness |
|
|
|
Nucleus ceruleus:
NT Function |
NE
Fight or flight response to physical and emotional stress |
|
|
|
Phenoxybenzamine:
Drug Class Use |
Non-selective alpha-adrenergic antagonist
Pheochromocytoma |
|
|
|
Nucleus Basalis of Meynert:
NT Disease Association |
ACh
Depleted in AD |
|
|
|
Ipratropium bromide:
Drug Class Use |
Muscarinic antagonist
Asthma |
|
|
|
Red Nucleus:
Role |
Motor coordination of upper extremities
|
|
|
|
Which enzymes require lipoic acid to function?
Result if lack of lipoic acid? |
PDH: deficiency-->lactic acidosis
alpha-ketoglutarate DH & branched-chain ketoacid DH: deficiency-->maple syrup urine disease |
|
|
|
Caudate Nucleus:
NT Disease Association |
GABA, ACh
Along with putamen, form striatum Affected in HD |
|
|
|
Which benzodiazepenes have the shortest half-life?
|
Alprazolam = SHORTEST half-life (less than 12 hours)
Lorazepam: 10-15 hours |
|
|
|
Chediak-Higashi Syndrome:
Presentation Pathophys |
Albinism
Nystagmus Recurrent staph and strep infections Abnl nphil phagosome lysosomefusion-->neuro abnlts |
|
|
|
Acute, painless monocular vision loss
|
Central retinal artery occlusion; often permanent
|
|
|
|
DiGeorge Syndrome:
Presentation Pathophys |
Thymic and parathryoid hypoplasia
Abnl facies Cardiac defects Recurrent viral, fungal, protozoal infections Due to Chrom 22 deletion-->maldevelopment of 3rd and 4th pharyngeal pouches |
|
|
|
Retinal artery occlusion:
Risk factors |
Atrial fibrillaiton
Carotid artery stenosis |
|
|
|
Lanhans Cell:
Formed by Associated disease |
Langhans giant cells seen in caseating granulomas of M. tuberculosis infection
Macs that form activated by CD4+ TH1 lymphocytes |
|
|
|
Cotton wool exudates
|
Diabetic retinopathy
|
|
|
|
Where (anatomically) do the majority of gastric ulcers occur?
Arteries involved? |
Great majority occur at lesser curvature, at border b/t acid-secreting and gastrin-secreting mucosa
Left and Right gastric aa run along lesser curvature and are likely to be damaged |
|
|
|
Injury to medial epicondyle of humerus:
Affected nerve |
Ulnar ("funny bone")
|
|
|
|
These arteries supply the greater curvature of the stomach.
|
Left (proximal) and right (distal) gastroepiploic aa
Note: Short gastric aa also supply prxoimal greater curvature above splenic a |
|
|
|
Injury to supracondylar humerus:
Affected nerve |
Median
|
|
|
|
Why is HCV genetically unstable?
|
Lacks proofreading 3'-->5' exonuclease activity
Thus makes many errors during replication and can readily mutate |
|
|
|
Injury to hook of hamate:
Affected nerve |
Ulnar
|
|
|
|
Concern when initiating ACE inhibitors.
|
First dose hypotension (usually mild but can be dangerous)
Must check if pt is taking thiazide or loop diuretics bc pts may be hypovolemia/hyponatremic. |
|
|
|
Sensation to posterior arm and forearm:
Nerve |
Radial
|
|
|
|
Patient presents with xanthoma.
Father died at 35 of MI. Mother suffers from RA. Concern? |
Hyperlipidemia
|
|
|
|
Sensation to lateral forearm:
Nerve |
Musculocutaneous
|
|
|
|
COPD:
Cause Symptoms Pathophys Lung volume findings |
Cause: heavy smoking
Pathophys: chronic bronchitis and emphysema Lung vol: Dec'd FEV1/FVC due to expiratory airflow obstruction Dec'd FVC Inc'd TLC Inc'd RV due to destruction of intralveolar walls, dec'd lung elastic recoil, distal airspace enlargement |
|
|
|
Flexion of forearm:
Nerve |
Musculocutaneous
|
|
|
|
Patient with 30 pack-year smoking history presents with progressive exertional dyspnea:
Pathophys |
Centriacinar emphysema due to oxidative injury of respiratory bronchioles and activation of resident macs
Nphils recreuited to airspace and release elastase, proteinase, etc (macs do this too) |
|
|
|
Extension of forearm:
Nerve |
Radial
|
|
|
|
Type I vs Type II Pneumocytes:
Abundance Role |
Type I: constitute over 95% of alveolar lining (target of destruction in emphysema)
Type II: Source of surfactant and responsible for repair of epithelium after destruction of type I cells |
|
|
|
E. coli colonies grown on lactose-containing medium up-regulated production of two different enzymes.
Why? |
Bacterial mRNA can be polycistronic, meaning, one mRNA codes for several proteins.
Transcription of these proteins is regulated by single promoter, operator, and regulatory elements. |
|
|
|
t(14;18):
Effects |
Causes overexpression of BCL2-->follicular lymphoma
|
|
|
|
Myastenia gravis:
Presentation Pathophys Tx |
Waxing, waning progressive weakness of voluntary muscles (ocular, masticatory, facial, deglutitional, lingual movement)
Weakening during continued activity Rapid restoratino of strength of affected mm w/rest Due to auto-ab's x postsynaptic nicotinic ACh receptors-->REDUCED END-PLATE POTENTIAL Tx: Pyridostigmine--cholinesterase inhibitor |
|
|
|
C-MYC gene:
Associated disease Histologic appearance |
Burkitt's lymphoma
Starry sky |
|
|
|
Scopolamine:
MOA |
Muscarinic antagonist--inhibits effects of ACh agonist at gut and NOT skeletal muscle (skel muscle uses nicotinic receptors)
|
|
|
|
BCL2:
Associated Disease |
Follicular Lymphoma
|
|
|
|
Pilocarpine:
MOA |
Nonselective muscarinic agonist
|
|
|
|
BCR-ABL:
Associated Disease |
CML
Note: BCR-ABL directs synthesis of protein tyrosine kinase that participates in signal transduction regulating cell growth |
|
|
|
Edwards Syndrome:
Chromosomal abnormality Presentation |
Trisomy 18, 47XX
Microcephaly Small jaws Small eyes (microophtlamia) Low-set ears Rocker-bottom feet Clenched hands, overlapping fingers**** |
|
|
|
Fever
Smoker Diarrhea Confusion |
Legionella pneumophila (community acquires pneumonia)
|
|
|
|
Patau Syndrome:
Chromosomal abnormality Presentation |
Trisomy 13
Cleft lip, palate Polydactyly Omphalocele (intestines protrude from navel) |
|
|
|
Legionella:
Gram -/+ Presentation Treatment |
Gram -
Fever, diarrhea, HA, confusion in smokers Tx w/erythromycin |
|
|
|
Patient in tractor accident with severe pain in leg. Leg swells rapidly and radiograph reveals gas in tissues.
Pathophys? |
Gas gangrene due to Clostridium perfringens.
|
|
|
|
Draw and label jugular venous pressure chart.
|
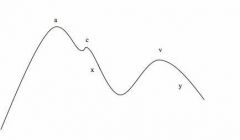
a = right atrial contraction
c = bulging of tricuspid valve into right atrium (early systole) x = right atrial relaxation v = passive increase in pressure and volume y = tricupid valve opens and right atrium passively empties (RV passively fills) |
|
|
|
Clostridium perfringens:
Gram -/+ Aerobic/anaerobic Shape Effects |
Gram +
Anaerobe Rod (bacillus) Causes gas gangrene, late-onset food poisoning characterized by watery diarrhea (when clostridial spores ingested) |
|
|
|
Constrictive pericarditis:
CT scan findings JV pressure findings Causes |
CT: Thickening and calcification of pericardium
JV Pressure: rapid and steep y descent Causes: XRT to chest, cardiac surgery, Tb (especially in pt immigrating from endemic region!!) |
|
|
|
How does glucose cause insulin release from pancreatic beta cells?
|
Glucose enters cell via GLUT-2
Undergoes oxidation-->ATP ATP binds KATP channel (K+)-->channel closes, causes depol-->Ca2+ channel depol-->Insulin release |
|
|
|
Hypertrophic cardiomyopathy:
JV pressure findings |
Prominent a wave
|
|
|
|
Sulfonylureas:
MOA Example |
Bind regulatory subunits of KATP channels and cause them to close
Note: Defect in KATP channel (K+ channel) in beta cells-->never closes, no insulin release Ex: glimepiride |
|
|
|
Eczema
Recurrent infections Thrombocytopenia |
Wiskott-Aldrich Syndrome
|
|
|
|
This hormone stimulates release of pancreatic bicarb.
Origin of hormone? |
Secretin; released by duodenal S cells in response to low pH
|
|
|
|
Wiskott-Aldrich Syndrome:
Presentation Pathophys |
Triad: eczema, thrombocytopenia, recurrent infections; onset ealry in life (within first year--after 6 month period of maternal colustrum IgA/mucosal IgG protection wears off)
Pathophys: B and T cell deficiency-->inability to mount humoral immune response against encapsulated organisms (Neisseria meningititids, H. influenzae, Strep pneumo) Note: WAITER mnemonic--immunodeficiency, thrombocytopenia (purpura), eczema, recurrent pyogenic infections |
|
|
|
Hemoglobin subunits during development.
|
Embryonic (yolk sac): 2 zeta, 2 epsilon chains
Fetal (most of gestation to first few months of life): 2 alpha, 2 gamma Adult (last month of gestation through life): 2 alpha, 2 beta |
|
|
|
T-tubules:
Role |
Invaginations of sarcolemma that transmit depolarization signals to sarcoplasmic reticulum-->trigger release of calcium
Required for coordinated contraction of myofibrils |
|
|
|
When does a beta-thalassemia present?
|
In infancy (around 6 months), bc baby still has gamma subunits in Hgb
|
|
|
|
What are ryanodine receptors?
|
Calcium release channels opened under influence of activated dihydropyridine receptors on T-tubules
|
|
|
|
Draw and label sarcomere
|
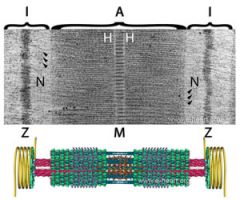
Note: Z to Z = 1 sarcomere
Z = thin, actin; anchor I = unbound actin M = thick, myosin; anchor H = unbound myosin A = overlapping actin and myosin |
|
|
|
Acute onset dyspnea
Calf swelling Prolonged immobility |
Pulmonary embolism
|
|
|
|
What is non-coding RNA?
Examples? |
RNA molecules that carry out functions without first being translated into proteins
Ex: snRNA, rRNA, tRNA |
|
|
|
Pulmonary embolism:
Arterial blood gas values (provide normal values as a reference) |
PE-->hypoxemia-->Acute respiratory alkalosis
Thus: -Inc'd pH (nL7.35-7.45) -Reduced PaO2 (nL 80-95) -Reduced PaCO2 (35-45) Alkalosis because the initial increase in CO2 (post-PE) results in an increased minute ventilation (hyperventilation)-->blow off too much CO2! |
|
|
|
Small nuclear ribonucleoprotein particles (snRNPs):
Function |
Important component of spliceosome--removes introns from pre-mRNA within nucleus
|
|
|
|
What is negative predictive value?
How does it differ from sensitivity? |
Probability of being disease free if test result is negative
NPV varies with pretest probability of dz, for ex: pt with high probability of having disease will have a low NPV with a negative test, whereas pt with low probability of having dz will have high NPV with negative test Note: prevalence of dz directly related to pre-test probability Sensitivity (and specificity) are fixed values! |
|
|
|
Amiodarone:
AEs Precautions |
AEs:
Thyroid dysfn Corneal micro-deposits Blue-gray skin discoloration Hepatitis (drug-related) Pulmonary fibrosis Amiodarone is 40% iodine by weight and can result in thyroid dysfunction (can be treated w/levothyroxine while continuing amiodarone) MUST test patients for TSH levels |
|
|
|
G-protein/adenylate cyclase second messenger system:
Which hormones employ this? What occurs after a hormone binds? |
Glucagon, TSH, PTH
Bind receptor-->GDP swapped for GTP Alpha-subunit (Gs) activates adenylate cyclase-->cAMP cAMP-->activates Protein Kinase A-->physiologic effects Protein Kinase A is essential for this second messenger system! |
|
|
|
Sensitivity vs Specificity
|
Sensitivity: True Pos/Number of subjects w/dz
Specificity: True Neg/Number of subjects without dz |
|
|
|
African-American
Bilateral hilar adenopathy Fever, weight loss Cough |
Sarcoidosis
Would expect to see non-caseating granulomas |
|
|
|
Sensitivity of test is 70%
Specificity of test is 90% 100 patients truly have disease 200 patients truly do not How many false positives in study? |
Make a table:
Horizontal :+UTI, -UTI, Totals Vertical: Test positive, Test negative Values: 70, 20, 90 30, 180, 210 Totals: 100, 200, 300 False positives = 20 |
|
|
|
Biopsy for TB shows ______.
|
CASEATING granuloma with acid fast bacilli
|
|
|
|
Prinzmetal's Angina:
Presentation Diagnostics |
Episodic, transient attacks of coronary vasospasm
Occurs at rest and during nighttime hours (early morning too) Produce temporary transmural MI with ST-segment elevation Dx w/ergonovine (provokes this vasospasm); tx w/nitrates, CCBs |
|
|
|
Hemoglobin electrophoresis results for:
Normal Hgb HgbC HgbS |
Normal Hgb will migrate most towards anode (+)
HgbC will migrate LEAST towards anode (+) bc has lysine (positively charged) where it should have glutamate HgbS will be in between bc valine (neutral) replaces glutamate |
|
|
|
Healthy patient inoculated with clostridium difficile does not develop signs of infection.
Why? |
Intestinal biomass prevents overgrowth of c diff.
Note; gastric acidity dos not destroy c. diff spores |
|
|
|
Hgb C:
Type of mutation What exactly happens? |
Missense mutation that substitutes glutamate with lysine resulting in (+) charge
|
|
|
|
cAMP levels:
Effect on heart activity Which receptor increases cAMP at the heart? Vascular effect of cAMP |
Beta-agonists-->inc'd cAMP-->inc'd conductance of calcium channels-->inc'd contractility
Inc'd cAMP in vasc SM-->vasodilation |
|
|
|
Non-histamine effects of diphenhydramine.
What other drug exhibits these effects? |
Diphenhydramine and chlorpheniramine are first-generation antihistamines.
Have following effects: Antimuscarinic (blurry vision secondary to pupillary dilation/failure of accommodation; dry mouth, urinary retention, constipation) Anti-alpha adrenergic (NE): hypotn, postural dizziness Anti-serotonergic: appetite stimulation, weight gain |
|
|
|
How does nitroglycerin relieve angina pectoris?
|
Venodilation-->retention of blood in venous system
-->Dec'd cardiac preload/work/myocardial oxygen demand and thus, dec in LV volume |
|
|
|
Changes in viral host range (organisms it can infect) is likely due to _______.
|
Mutations in surface glycoproteins (mediates virion attachment to target host cell plasmalemma receptors)
|
|
|
|
Preload =
|
LV fill volume
|
|
|
|
Methylmalonic acidemia:
Pathophys (include carboxylation) |
Catabolism of isoleucine, valine, odd-chain Fas, cholesterol (etc.)-->propionic acid-->methylmalonic acid via biotin-dependent carboxylation
Isomerization of methylmalonyl Coa-->Succinyl CoA-->TCA cycle If have defect in isomerization-->methylmalonic acidemia |
|
|
|
Which drugs are P450 inducers?
|
Barbiturates
Phenytoin Rifampin Carbamazepine Griseofulvin Chronic EtOH Barb takes Phen-Phen and Rifuses to take GRISy CARBs and Alcohol. |
|
|
|
Beta-hemolytic gram-positive cocci in chains
Bacitracin resistant |
Streptococcus (staph forms clusters)
Bacitracin resistant excludes S pyogenes (GAS) and indicates S agalactiae (GBS) |
B
|
|
|
Which drugs are P450 inhibitors?
|
PICK EGS
Protease Inhibitors!!! Isoniazid Cimetidine Ketoconazole (other azoles) Erythromycin (other macrolides) Grapefruit Juice Sulfonamides |
|
|
|
How would you prevent fetal infection with vaginal GBS during childbirth?
|
Intrapartum ampicillin
|
|
|
|
Which drug classes are shown to slow progression of diabetic nephropathy?
Class suffixes? |
ACE inhibitors (pril)--Angiotensin Converting Enzyme Inhibitor
Angiotensin Receptor Blockers (sartan) |
|
|
|
Prophylaxis for definitive exposure to N. meningitidis.
|
Rifampin. Note: this is a monotherapy!
|
|
|
|
Microalbuminuria vs Macroalbuminuria:
Cutoffs Which can dipstick identify? |
Microalbuminuria: 30-300mg albumin/day
Macroalbuminuria: 300+mg albumin/day Dip stick can only ID macroalbuminuria |
|
|
|
Diuretic of choice for someone with HTN/CHF and osteoporosis.
Why? |
HCTZ
HCTZ is not only a diuretic, but also increases absorption of calcium from DCTs. Applies to all thiazides! Note: HCTZ also induces hypocalciuria (since Ca2+ is absorbed) which mhelps prevent renal stones in some pts. |
|
|
|
MAO Inhibitors:
Indication |
ATYPICAL depression
Not a first-line tx for depression |
|
|
|
Describe and identify murmur.
|
Decrescendo Diastolic
Aortic Regurgitation |
|
|
|
Phenelzine:
Drug Class |
MAO-I
|
|
|
|
Describe and identify murmur.
|
Crescendo/Decrescendo Systolic Murmur
Aortic Stenosis |
|
|
|
Tranylcypromine:
Drug Class |
MAO-I
|
|
|
|
Describe and identify murmur.
|
Holosytolic Murmur
Mitral Regurgitation |
|
|
|
Atypical Depression:
Presentation |
Mood reactivity
Leaden Fatigue (arms and legs feel heavy) Inc'd sleep and appetite Rejection sensitivity (overly sensitive to slight criticism) |
|
|
|
Describe and identify murmur.
|
Decrescendo Diastolic with Opening Snap
Mitral Stenosis |
|
|
|
Recurrent pulmonary infections
Exocrine gland fibrotic atrophy |
Cystic Fibrosis
|
|
|
|
Describe and identify murmur.
|
S3 Ventricular Gallop (protodiastolic)
|
|
|
|
Vitamin deficiencies seen in cystic fibrosis?
Why? |
CF-->pancreatic insufficiency (inspissated mucus)-->fat malabsorption
Deficiency of Vits A, D, E, K |
|
|
|
Describe and identify murmur.
|
S4 Atrial Gallop (Presystolic)
|
|
|
|
Lack of vitamin A results in ______.
|
Vitamin A maintains dx/dy of specialized epithelia (columnar epithelia of ocular conjunctiva, respiratory and urinary tracts, panreatic and other exocrine ducts)
Lack of vitamin A-->squamous metaplasia of such epithelia-->keratinizing epithelium |
|
|
|
Holosystolic, blowing murmur
|
Mitral regurgitation
|
|
|
|
Lack of vitamin E results in ______.
|
Infertility
|
|
|
|
23-year old immigrant from developing nation
Mitral regurgitation Dyspnea on exertion |
Rheumatic heart dz
|
|
|
|
Mesolimbic-Mesocortical System:
NT Released Function Disease Association |
DA released
Regulates behavior Assocd w/Schizophrenia |
|
|
|
Systolic ejection murmur
|
Atrial septal defect
|
|
|
|
Nigrostriatal System:
NT Released Function Disease Association |
DA release
Coordination of voluntary movements Assocd w/PD |
|
|
|
Mid-systolic ejection murmur over right second intercostal space, radiation to neck
|
Bicuspid aortic valve
|
|
|
|
Tuberoinfundibular System:
NT Released Function Disease Association |
DA
Controls PL secretion Assocd w/hyperprolactinemia |
|
|
|
Opening snap murmur
|
Mitral stenosis
|
|
|
|
Male pattern baldness:
Describe pattern Treatment |
Hair loss from anterior scalp and vertex
Possible to treat with finasteride--5-alpha reductase inhibitors to inhibit production of DHT |
|
|
|
Interrupted migration of neural crest cells to intestine:
Associated disease Region affected |
NCC's form submucosal (Meissner) and myenteric (Auerbach_ plexi
This is Hirschprung's Dz; affects rectum because NCCs migrate caudally! |
|
|
|
Paramesonephric ducts become _______.
|
uterine tubes
uterus cervix superior 1/3 of vagina |
|
|
|
Thiazolidinediones:
MOA AEs |
Activate PPAR-gamma (peroxisome proliferator activated receptor gamma), which alters transcription of genes responsible for glucose and lipid metabolism.
Overall effect: inc'd insulin sensitivity. Does not cause hypoglycemia! AEs: fluid retention, weight gain, precipitation of CHF from fluid retention |
|
|
|
Failure of paramesonephric ducts to fuse results in ______.
|
uterus didelphys--two separate vaginas, cercies, uterine horns
|
|
|
|
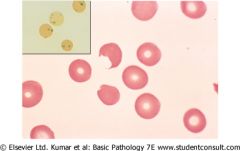
G6PD Deficiency Anemia:
Hallmark sign Causes |
Bite cells, Heinz bodies
Causes: Oxidative stress from: -Infection -Drugs: DAPSONE, antimalarials, TMP-SMX -DKA -Favism (FRESH FAVA BEANS) |
|
|
|
Mesonephric ducts become ______.
|
Males: epidydmis, ductus deferens, SVs, Ejaculatory Ducts
Females: Gartner's ducts |
|
|
|
Bite cells, Heinz bodies-->G6PD deficiency
|
|
|
|
Mesonephric tubules become ______.
|
Males: efferent ductules (carries sperm from testis to epididymis)
|
|
|
|
Respiratory Syncytial Virus:
Effects Presentation Treatment |
Viral bronchiolitis in children (usually self-limiting though)
Presents as wheezing, rales, prolonged expiration If severe and no comorbidities: warmed humidified oxygen and IV fluids If severe RSV in child w/immunodeficiency, prematurity, or cardiopulmonary dz-->RIBAVIRIN |
|
|
|
Involution of the _________ only occurs in males.
|
Paramesonephric ducts
|
|
|
|
Ganciclovir:
Use |
Herpes
|
|
|
|
Incomplete fusion of the urethral folds results in _______.
|
Hypospadias--uretrha opens at ventral surface of penis rather than distal end of glans
|
|
|
|
Acute obstruction of small airways in infant
|
RSV
|
|
|
|
____ positivity in breast cancer indicates sensitivity to tamoxifen treatment.
|
Estrogen Receptor (ER)
Progesterone Receptor (PR) |
|
|
|
What is a latent period (epidemiology)?
|
Time elapsed from initial exposure (treatment) to clinically apparent disease
|
|
|
|
____ positivity in breast cancer indicates an aggressive tumor that should respond to _________.
|
ERB-B2 (HER2/NEU) positivity = aggressive tumor-->treat with MAB trastuzumab
|
|
|
|
When does selection bias occur?
|
Inappropriate (non-random) selection methods or through selective attrition of study participants
|
|
|
|
Positive VDRL
Pleocytosis |
Neurosyphilis
VDRL = venereal disease research laboratory |
|
|
|
When does lead time baias occurs?
|
Note: Lead time = time between initial detection of dz and specific outcome or measured endpoint
Lead time bias can occur when comparing 2 different tests for same dz when one of tests can accurately detect dz at earlier stage. May erroneously conclude that earlier-detection test prolongs survival, when increased survival time is due solely to earlier detection of disease. |
|
|
|
4 stages of syphilis and findings of each
|
Primary: painless ulceration with raised borders = CHANCRE
Secondary syphilis: bacteremia; diffuse macular rash of palms, soles; CONDYLOMA LATA (wart-like growths on genital/perineum) Latent Syphilis: asyx Tertiary: many years after infection in untx'd individuals; neurosyphilis (positive VDRL and pleocytosis); GUMMAS--benign, painless, indurated granulomatous lzns |
|
|
|
Short upper and lower extremities compared to axial skeleton
|
Achondroplastic dwarfiwm
|
|
|
|
What are keloids?
|
Keloids result from excessive collagen formation during tissue repair
Present as soft or firm nodules that grow beyond borders of wounds |
|
|
|
Achondroplasia:
Most common defect Pathophys |
Mutation in fibroblast growth factor receptor 3 at epiphyseal growth plate-->inhibits growth and results in short, thick long bones; but normal axial skeleton
|
|
|
|
3 phases of wound healing and time (days) after infection.
|
Inflammatory phase: nphils--first 24 hours; macs (2-3 days)
Proliferative phase: 3-5 days--fibroblasts, endothelial vascular cells proliferate Maturation: fibrosis (scar formation); by 6-8 week initial scar is complete |
|
|
|
Short stature
Axial and appendicular skeleton are proportionate |
GH/IGF-1 deficiency
|
|
|
|
These organisms form spores and are resistant to high temperatures, desiccation, and chemical agents.
|
Bacillus and Clostridium
Both found in soil |
|
|
|
Deficiency of what vitamin in premature neonate can be life threatening in first week of life?
Why? |
Vitamin K deficiency.
Infants have immature liver, sterile GI tract, and breast milk has little vitamin K. Vitamin K deficiency puts infant at risk of hemorrhagic disease of newborn (leads to intracranial bleeding!) |
|
|
|
Brain section with extensive atherosclerosis in vascular beds reveals ischemic lesion.
Describe healing process. |
Ischemia-->Neurons die
Macs phagocytize neuronal fragments and debris, stay for a few months. Astrocytes enlarge and proliferate (gliosis) to form a wall around cystic cavity. |
|
|
|
Cancer stage vs grade (general)
|
Stage = how much tumor spreads to adjacent tissues/distant organs
Grade = degree of tumor differentiation; well-diff = low grade (likely benign) Large number of cells in S phase-->high grade tumor; poor prognosis |
|
|
|
Definitive diagnosis of acute calculous cholecystitis.
|
Radionuclide biliary scan (HIDA) failing to show gallbladder is definitive dx
Nonobstructing biliary stones seen on u/s are suggestive but not diagnostic. |
|
|
|
Nitroprusside:
MOA Use AE |
Mixed arterial and venous vasodilation
Use in hypertensive emergency AE: Nitroprusside initially metabolized to cyanide Can result in cyanide toxicity |
|
|
|
Cyanide toxicity:
Cause Treatment |
Cyanide (duh)
Nitroprusside (initially metabolized to cyanide) Treat with sodium thiosulfate (SULFUR); enables liver's ability to convert cyanide to thiocyanate |
|
|
|
Neuroleptic Malignant Syndrome:
Cause Presentation |
Haloperidol = most common cause
Due to anti-DA activity of antipsychotics (esp of D2 receptor) Presentation: Hyperthermia Generalized rigidity Autonomic instability Altered mental status Agitation |
|
|
|
Serotonin Syndrome:
Cause Presentation |
Combined use of SSRIs and MAOIs associated with serotonin syndrome (increases serotoninergic tone)
Presents with myoclonus (muscle twitching) Overactive reflexes Hyperthermia Agitation |
|
|

Label GU structures
|

|
|

