![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
What is the epidemiology of traumatic brain injuries?
|
- > 5 million people in US with TBI-associated deficits
- ~$40 billion dollars/year - Longterm consequences most concerning - Trimodal distribution -- 0-4 yrs (toddlers have big heads and limited balance) -- 15-25 yrs -- >60 yrs - Men >> women (incidence of TBI 2 times greater in males; incidence of death 3 times greater in males) - Leading causes of TBI: Falls, Motor Vehicle Accidents, “Struck by/against,” and Assault Leading causes of death: Firearms, Motor Vehicle Accidents, and falls - Mortality: <20/100,000 TBI -- Has decreased over the past 30 years -- Social awareness regarding speed limit laws, seat belt laws, and drunk driving laws -- Improved care at the site of injury and hospital through evidence-based treatment at trauma centers and neuro-ICUs |
|
|
What are the basic types of traumatic brain injuries based on time?
|
Primary injury - damage at the time of impact
Secondary injury - damage occurring in the hours-weeks following primary injury |
|
|
What are the components of primary brain injury? (ie, what layers should you consider? what injuries may be present in each of those layers?)
|
Scalp - lacerations, avulsions, hemorrhage, shock (possible)
Skull - Fractures (linear, depressed, closed, open) which are usually listed by location (cranial vault, basal skull) Brain parenchyma - focal injury (hematomas [EDH, SDH, ICH; contusions; look for coup-contracoup lesions], penetrating injury), diffuse injury (concussion, diffuse axonal injury (DAI)) |
|
|
What are the types of skull fractures?
|
Linear (most common):
- Suspicion of epidural hematoma is increased if linear fracture crosses the middle meningeal artery groove - Remember that the middle meningeal artery is epidural (between the dura and the skull) Depressed: - occur when the outer cortex of bone falls inside the inner table of the skull; generally must be surgically removed Basal: - most commonly extensions of linear vault fractures, and usually involve the petrous temporal bone or the orbital frontal bone - Clinical findings may include cranial nerve palsies (because many of them run along the base of the skull and can be transected or stretched following trauma) - “Raccoon eyes” (peri-orbital echymosis) or clear discharge from the nose (CSF rhinorrhea) suggests a frontal basilar skull fracture - “Battle’s sign” (mastoid echymosis) or clear discharge from the ears (CSF otorrhea) suggests a temporal skull base fracture All skull fractures can either be open (under broken skin) or closed (under intact skin). |
|
|
What are "raccoon eyes" and what do they indicate?
|
Also peri-orbital echymosis
Dark circle around eyes, bilateral Indicate frontal basilar skull fracture |
|
|
What is "Battle's sign" and what does it indicate?
|
Also mastoid echymosis
Bruising behind the ear Indicate temporal skull base fracture |
|
|
What is the Monro-Kellie Doctrine?
|
- Skull is fixed space composed of brain parenchyma, CSF and blood
- Brain parenchyma (mass lesions), CSF (hydrocephalus), or blood (edema) expansions lead to intracranial pressure increases - Brain does not like to move! When brainstem is crushed due to movement → herniation - No matter how high the pressure inside the ventricles, the production of CSF will not stop until the pressure is exceptionally high. Therefore, you can have hydrocephalus without a change in CSF production requiring an extraventricular drain to relieve pressure. |
|
|
What is cerebral perfusion pressure?
|
cerebral perfusion pressure = mean arterial pressure - intracranial pressure
CPP= MAP-ICP |
|
|
What systemic effects can intracranial pressure cause? (Think CPP equation)
|
Due to the relation between cerebral perfusion pressure, intracranial pressure, and mean arterial pressure, increases in intracranial pressure results in an increase also in mean arterial pressure to compensate and maintain the same cerebral perfusion pressure
However, if the intracranial pressure increases enough, the arterial pressure may not be able to keep up, resulting in hypoperfusion to the brain |
|
|
What can result from brain hypoperfusion? (multiple steps)
|
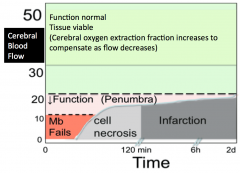
- Ischemia and inadequate oxygen delivery to tissues causes cells to rely on anaerobic glycolysis as a source of ATP
- Decreased ATP from this process causes an increase in Adenosine, Glutamate and Lactate - Glutamate uptake is dependent on the Na+ gradient which is maintained by ATP. Thus a decrease in ATP causes increased extracellular glutamate which can lead to NMDA receptor overactivation and increased Ca2+ uptake - Ca2+ translocates into the mitochondria leading to swelling and disruption of the mitochondrial membranes affecting key metabolic processes such as oxidative phosphorylation - Ca2+ entry can further lead to release of cytochrome c and the activation of caspases which lead to apoptosis - Formation of free radicals can lead to necrosis |
|
|
What is an epidural hematoma?
|
- Localized collection of blood that results from injury to blood vessels outside the brain but within the skull
- Most commonly occur after injury to middle meningeal artery (MMA) - Respect the suture lines (dural attachment points) and therefore are lens-shaped - Can eventually cause midline shift (shift of cerebral hemisphere beyond the central line seen on a CT scan) Typical story: - Short loss of consciousness (typically) followed by a “lucid interval” (brief period of recovery after the initial trauma and before the epidural hematoma has had time to accumulate and shift the brain contents within the skull) and then a sudden deteriorating course as the arterial hemorrhage increases in size - Prognosis is good if patient is brought to the hospital in time even if they deny symptoms during lucid interval |
|
|
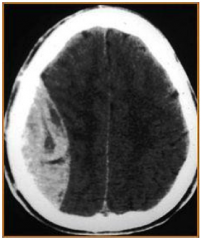
What is a subdural hematoma?
|
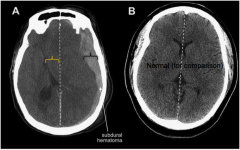
- Venous (rather than arterial in origin) so they are more likely to accumulate slowly
- Results from tearing of the bridging veins or the veins that drain the cerebral cortex crossing the subdural space - Does not respect suture lines - Can also eventually cause a midline shift - Commonly seen in elderly patients as a result of MVAs or falls because atrophy of cerebral cortex in aging causes natural stretching of bridging veins Typical stories: - Mild trauma in elderly patient (fall, small car accident), with increased confusion/ decreased consciousness |
|
|
What are the differences between an epidural and a subdural hematoma?
|
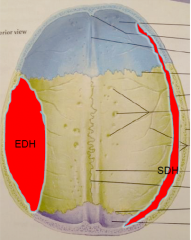
Epi - between dura and skull, sub - between dura and arachnoid
Epi - lens shape, sub - crescent towards periphery Epi - respects the suture lines, sub - does not respect suture lines |
|
|
What are the types of cerebral hemorrhage from traumatic brain injury?
|
![Contusion (left) - bruising of the brain from impact
Coup-contrecoup [it's an e, not an a] (right) - Coup injury at the site of impact, contrecoup injury at the opposite end of the head (front back, left right)](https://images.cram.com/images/upload-flashcards/927467/637459_m.png)
Contusion (left) - bruising of the brain from impact
Coup-contrecoup [it's an e, not an a] (right) - Coup injury at the site of impact, contrecoup injury at the opposite end of the head (front back, left right) |
|
|
What are the general causes of penetrating brain injuries?
|
Nail gun injuries - risk of bacterial infection
Gunshot injuries - bullets are hot and fast -> decreased infection risk, but significant damage from shockwaves from kinetic injury |
|
|
What are the types of diffuse primary injury?
|
Concussion - mild TBI
Chronic traumatic encephalopathy - effects of cumulative TBIs Diffuse axonal injury - diffuse injury from high-acceleration impacts (comatose), but also less severe TBIs |
|
|
What is a concussion and its symptoms? How is it graded?
|
Mild TBI, with or without loss of consciousness
Common injury: 20% of contact sports players per season; 15% of soldiers, and does not have to be associated with a blow to the head itself (think of blast injury). Frequently observed symptoms: - Vacant stare - Delayed responses (verbal or motor) - Confusion, inability to focus attention (slow to answer questions or follow instruction) - Disorientation (walking on the wrong direction, unaware of time, date, place) - Slurred or incoherent speech (making disjointed or incomprehensible statements) - Gross observable incoordination - Emotions out of proportion to circumstances (like irritability) - Memory deficits - Any period of loss of consciousness Pathogenesis may include axonal disruption and secondary injury Imaging abnormalities may be seen in 5-30% of MILD TBI on CT/MRI (although they’re much more common in severe TBI) Glasgow Coma Scale (used to measure eye, verbal and motor responses) score of 13-15 (scale ranges from 3-15). This indicates a “very good to normal” score. Evaluation: - Any athlete with a suspected concussion is to be removed from play until evaluated by a medical professional with training in the evaluation of concussion - Any loss of consciousness (automatic grade 3 concussion) requires Emergency Department evaluation. - No athlete suffering concussion symptoms should be allowed to resume play—the exam has to be at baseline. Premature return of a concussed athlete can increase the risk of “Second Impact Syndrome” (rapidly progressing cerebral edema leading to secondary injury) and re-concussion Grading: - GRADE 1: Transient confusion, no loss of consciousness, concussive symptoms or mental status abnormalities that resolve in < 15 min. -- Can return to play if normal sideline assessment (by medical professional or certified athletic trainer) while at rest and with exertion, including detailed mental status examination - GRADE 2: Transient confusion, no loss of consciousness, concussive symptoms or mental status abnormalities that resolve in > 15 min. CANNOT return to play. - GRADE 3: Any loss of consciousness, either brief (secs) or prolonged (mins). CANNOT return to play. |
|
|
What is chronic traumatic encephalopathy?
|
Deleterious effect of cumulative TBIs causing cognitive impairments, lower scores on neuropsychological testing, personality changes, depression, parkinsonian features among football players, boxers, soccer/hockey players, etc.
Athletes subjected to numerous TBIs have shown degenerative changes and an increased association with Alzheimer Dementia |
|
|
What is diffuse axonal injury?
|
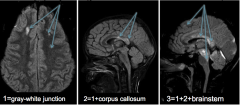
- Primary diffuse injury that is common in high-acceleration impacts (typically with a comatose patient) but also seen among less severe TBI
- CT may be normal/small hemorrhage - Twisting force (skull is curved) produces shear force - MRI may show restricted diffusion (decreased movement of water) with or without punctate hemorrhage Graded as shown above (3 is the worst) |
|
|
What is a secondary injury from TBI?
|
Damage occurring in the hours to weeks following a primary injury
- A target for prevention or amelioration - Examples: edema, ischemia, oxidative injury, neurochemical disruption, toxicity - Original TBI definitions emphasized primary injury while secondary injury focused on edema and ischemia - Gennarelli said that TBI is a process, not an event (brain damage due to TBI is an ongoing event) - A great deal of cellular damage occurs after the initial mechanical insult - The definition of secondary injury has changed significantly in the last few decades |
|
|
What are treatment and management methods for secondary injury in TBI?
|
Treatment:
- Current research aimed at preventing secondary injury in TBI patients by targeting different points in the injury cascade including decreased neurotransmitter regulation, increased intracellular calcium, mitochondrial dysfunction, free-radical production, lipid peroxidation, inflammation and apoptosis have all be unsuccessful so far (including steroids which actually harmed people!) -- For now best intervention is to prevent the trauma in the first place (ie. take the beer out of the kid’s hand before he hurts himself) Avoidance: - Countering decreased delivery of oxygen and nutrients -- Ensure adequate consistent O2 and nutrient delivery. -- Avoid hypermetabolism in brain (ensure fever control, seizure control, & adequate sedation) - Countering decreased blood flow (edema/ischemia/infarction) -- Avoid hypotension and hypovolemia -- Control Intracranial Pressure (ICP) as much as possible (osmotic agents/ventilator/sedation) -- Ensure Mean Arterial Pressure (MAP) is enough for adequate cerebral perfusion and measure continuous ICP if poor neuro exam -- If further increased ICP, may need further imaging/neurosurgical consultation |

