![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
What 4 procedures warrant IE prophylaxis?
|
1. Dental procedures
2. articifial valves 3. previous IE 4. Procedures which manipulate the airway |
|
|
Describe the shape of the lesions, location on the valve and content for rheumatic verrucae and IE vegetations
|
Shape:
RF - warty, in a regular row IE - large irregular mass Location on valve: RF - along the closure line of the leaflet IE - valve cusps extending into the chordae & endocardium Content: RF - steril, immune complexes IE - bacteria, fibrin, inflam cells |
|
|
Mitral regurg results from structural abnormalities in the annulus, leaflets and chordae tendinae.
What are 2 causes of acute MR, and 4 causes of chronic MR? |
Acute MR:
- MI (dysfunction, scarring or rupture of papillary) - IE (perf of the leaflet or rupture of chordae) Chronic: - R-fever: shortening of chordae & retraction of leaflets - Myxomatous degen of valve: ?etiology but causes leaflet prolapse - Htrophic cardiomyopathy: abnormal motion of anterior leaflet preventing normal valve closure - LV dilatation: distorts normal geometry of sub-valvular apparatus (annulus) |
|
|
When a person has Mitral regurg what are the acute vs chronic symptoms? What is the pathophysiology that causes these symptoms?
|
Acutely - the LA is non-compliant and can't accept the regurgitated blood so it backs up and causes pulmonary edema.
If MR persists the LA will dilate and accept the regurgitated blood. This diminishes CO and subsequent fatigue and symptoms of L-sided heart failure develop. |
|
|
What are the 2 major causes of aortic stensosis?
|
deterioration of a congenitally bicuspid valve or age-dependent calcification.
|
|
|
AS obstructs LV outflow resulting in ↑↑ LV pressure. What effect does this have on the ventricle itself? What 3 symptoms does this produce?
|
When LV outflow is obstructed the pressure rises and this cause concentric Htophy → reduces wall stress but also ↓ compliance = ↑LV diastolic pressure and subsequent LA Htrophy.
Causes: - CHF: LV contractile dysfunction d/t ischemia = ↑LA pressure = pulmonary edema - Angina = concentric Htrophy = more tissue/more deman and ↓ supply d/t ↑ LVEDP which ↓ coronary perfusion - Syncope d/t impaired ability of the LV to increase CO |
|
|
What are the 2 main causes of aortic regurgitation?
What is the effect of the regurgitated blood on the LA and LV? |
Etiology: disease of the aortic leaflets or dilation of the aortic root (dissection, aneurysm).
Pathophysiology: regurgitated blood adds to the LA filling volume = ↑ stroke volume in next round of systole causes volume overload of LV = eccentric dilation and stretch. |
|
|
Whta 3 factors influence the severity of Aortic regurg?
When and why would AR be a surgical emergency? |
1. Size of the regurgitant orifice
2. Pressure gradient across the aortic valve during diastole 3. duration of diastole. Acute AR is a Sx emergency b/c it will substantially ↑LVEDP which ↑↑↑ LAtrial Pressure causing significant pulmonary edema. |
|
|
What is almost always the cause the mitral stenosis?
What are 3 phathologic hallmarks? |
Rheumatic fever (other causes <1%).
1. Fibrous thickening of &calcification of the leaflets, 2. Fusion of the commissures 3. Thickening & shortening of the chordae. |
|
|
What is the effect of mitral stenosis on both sides of the heart?
What is the net effect on the heart? |
Obstructed LA emptying causes pressure in the LA to ↑ and this gets transmitted back thru the pulmonary circuit to ↑ R heart pressures. The ↓ in LV filling also reduced CO.
|
|
|
What type of valve problem can cause AF? How does it do this?
What is the effect of AF on cardiac output? In what 3 ways does it cause this effect? |
Mitral stenosis causes AF because it ↑ LA pressure so much that the LA undergoes hypertrophy which promotes AF.
AF causes ↓ CO b/c the ↑HR shorten diastolic filling time and the fibrillation removes the atrial kick so less blood fills the LV (also less blood can get through the stenotic Mitral valve!!) |
|
|
What are the 3 main causes of dilated cardiomyopathy?
|
1. Genetics: mutations in sarcomere, cytoskeleton or nuclear envelope.
2. EtOH: rare but reversible (? d/t impaired mitochondrl oxid phos & fatty acid Plation) 3. Viral endocarditis (usually from coxsackie B infection, which is usually self-limiting but can progress to DCM) |
|
|
What are the 2 acute mechanisms that compensate for DCM?
As the heart dilates, contractility ↓ and this lowers CO. What is the kiney's response and what affect does this have on the heart? What are 2 subsequent consequences? |
1. Frank-starling & Neurohumoral
When renal perfusion ↓ they activate the RAAS system. The aldo ↑es blood volume worsening the pulmonary & systemic congestion, while the AngII ↑systemic resistance which ↓ LV ejection. This worsens the chamber dilation which can lead to M & T valve regurgitation = further atrial dilation (↑ A-fib risk) and ↓ SV/CO |
|
|
Hypertrophic Cardiomyopathy is a common genetic condition affecting 1/500 individuals. The clinical presentation can be highly variable. What is the main goal of dx?
What is the rationale for gene-testing? When ppl have a + mutation, how are they screened & treated? |
Goal: catch ppl with HCM early & find those at risk of severe/life-threatening events.
Rationale for gene testing: identifying a mutation lets you screen for other mutation carriers in the family. Screening: holter ECG and Exercise Tolerance Test Tx: Internal Cardioverter Defibrillator (ICD) |
|
|
How does Hypertrophic Cardiomyopathy cause outflow tract obstruction?
Although this can produce an impressive murmur and mitral valve regurgiation, what are the symptoms primarily d/t? |
Thickened septum alters the hemodynamics such that the anterior leaflet of mitral valve transiently blocks blood from entering the aorta.
Symptoms primarily d/y LV stiff ness and diastolic dyfunction (in addition to potential Pedema. |
|
|
In HCM without obstruction, what is the effect of the hypertrophy? What symptom(s) will this produce and why/how?
|
HCM w/o obstruction:
↑ stiffness impairs diastolic filling (causes it to occur @ higher pressure) This ↑ in pressure is transmitted backwards = ↑ P in Latria, pulmonary veins/capillaries, producing dyspnea |
|
|
What are the two main causes of the less common restrictive cardiomyopathy?
These causes will reduce the compliance of the ventricles leading to an ↑ in what? What 2 things does this ↑ cause? |
1. Fibrosis of the endocardium
2. Infiltration of myocardium by an abnormal substance (such as amyloid) ↓ compliance of the ventricles causes an ↑ in diastolic filling pressures leading to: 1. ↑ systemic & pulmonary venous pressures = R + L congestion 2. ↓ ventricular cavity size w/↓ SV and thus ↓ CO |
|
|
What depends on afterload but is independant of the stretch in the myocardial fibers prior to contraction? (2things) (ie what is unaffected by frank-starling forces?)
|
The pressure generated by the ventricle & the EDV are both independant of F-S stretch
|
|
|
The force of contraction of the heart depends on what single factor? What 2 things is it independant of?
|
The force of contraction of the heart depends on inotropy (contractility) only. It is independant of afterload & preload.
|
|
|
Inotropy depends on what 2 factors?
|
Inotropy is dependent on chemical & hormonal influences
|
|
|
What 3 things will influence stroke volume?
|
1. Contractility
2. Preload 3. Afterload |
|
|
In the pressure-volume curve, how does heart failure shift the curve?
|
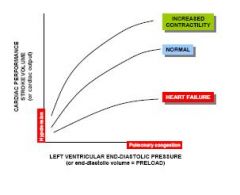
Shifts it to the right and down
|
|
|
What is the effect of changes in preload and afterload on stroke volume?
|
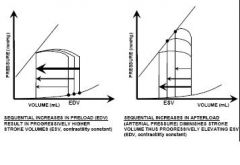
Preload & SV are directly proportional. An increase in one causes an increase in the other. Afterload however is inversely related. An increase in afterload will decrease SV.
|
|
|
Changes in preload will change what end volume? What about changes in afterload?
|
Changes(↑) in preload will increase EDV but won't change ESV.
Changes(↑) in afterload will increase ESV but won't change EDV. |
|
|
Draw the PV graph for both diastolic and systolic dysfunction
|
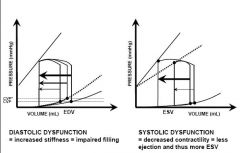
Diastolic dysfuntion shifts venous pressure line up where as systolic dysfunction shifts the volume line down.
|
|

What are the key findings indicating heart failure on a CXR?
|
1. Pleural effusion
2. Vascular redistribution 3. Peribronchial cuffing 4. Cardiomegaly 5. Kerley-B lines (1-2cm horizontal lines caused by ++ fluid in lyphatics/interstitium) 6. Batwing pattern of vessels at hilum |
|
|
What hemodynamic change would make the heart prone to R-sided heart failure? What are 3 causes of this change?
What is the commonest cause of R-heart failure? |
When there is a sudden increase in the R ventricular afterload the heart is ++ prone to R-sided heart failure. ↑ afterload can be caused by: PE, lung parenchymal disease and/or pulmonary HTN)
The commonest cause of R-sided heart failure is actually L-sided heart failure that gets transmitted back |
|
|
How does R ventricular failure lead to a fall in CO?
|
RV failure causes a back-up of pressures to be transmitted to the RA, this causes congestion & back-up in the veins which lowers preload & LV filling resulting in a fall in forward CO
|
|
|
What are the 2 major compensatory mechanisms for heart failure?
(excluding neurohumoral) |
1. Frank-starling: when chambers have incomplete emptying during systole, the ESV begins to accumulate and this will initally ↑SV. But as heart fails this achieves only a small amount of ↑SV b/c the filling gets transmitted backwards & causes p edema.
2. Hypertrophy: in the ventricular myocardium to ↑contractile force and ↓wall stress. Again, starts off good but then causes diastolic dysfunction b/c it impedes filling (↑ EDP which transmits to lung vessels). |
|
|
In response to heart failure and ↓CO, the body activates the adrenergic system. How is the system signalled? What are the 3 physiologic effects of activation?
In what way is this strategic (on the bodies part?) |
Falling BP detected by barroreceptors that send signals along CN IX & X to the medulla = ↑symptathetic outflow.
Effects: ↑ HR; ↑Contractility; and a stimulation causing Vcon in the arteries & veins Strategic b/c the Vcon in the veins increases venous return which ↑es preload. the a-receptors are strategically distributed such that blood is diverted to vital organs & away from skin, GI and kidneys. |
|
|
What are the 3 main stimuli for the RAAS system in heart failure?
What are the 3 main effects of Ag II? |
1. Low circulating volume
2. Less Na being delivered to the macula densa 3. direct stimulation of B2-receptors by adrenergic nervous system Renin --> Ag II - causes Vcon to ↑PVR and thus ↑BP - stimulates thirst at Hothalamus - stimulates adrenal cortex to release Aldo (aldo ↑es NaCl absorption) |
|
|
How are the neurohumoral compensatory mechanisms detrimental for the heart (in long term)?
(4 ways) |
1. ↑es circulating volume = pulmonary congestion
2. ↑ arterial resistance = ↑afterload which worsens LV failure 3. ↑HR = ↑metabolic demands 4. Sympathetics = ↓-regulation of B-receptors ... adverse cardiac remodeling |

