![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
137 Cards in this Set
- Front
- Back
|
What are the common viruses that cause myocarditis?
|
coxsackie virus, Echovirus, Adenovirus, EBV, CMV, Influenza
|
|
|
A south American immigrant has cardiomegaly and achalasia. What is the organism likely responsible for this patient's disease?
|
Chagas Disease - Trypanosoma Cruzi
|
|
|
What are the major JONES criteria in the diagnosis of rheumatic heart disease?
|
Joints (polyarthritis)
Heart - pancarditis & vallve damage Nodules (subcutaneous) Erythema marginatum (painless rash) Syndenham's Chorea |
|
|
What is the mneumonic to remember the classic physical exam findings of endocarditis?
|
"FROM JANE"
Fever Roth Spots Osler's Nodes Murmur Janeway Lesions Anemia Nail-bed hemorrhages Emboli |
|
|
Tiny septic emboli fly off the infected valve in endocarditis and travel to peripheral vessels, causing tiny hemorrhages. What are the names of some of these sites of micro-hemorrhages?
|
Janeway lesions - peripheral petechiae
Osler's nodes - tender nodules on finger & toe pads Roth's spots - retinal hemorrhages Splinter hemorrhages - sublingual petechiae |
|
|
What is the best study to visualize a vegetation on a heart valve?
|
TransEsophageal Echocardiogram (TEE)
|
|
|
What is the treatment for endocarditis?
|
long-term IV antibiotics (4-6wks)
|
|
|
What blood pressure defines prehypertension? How should prehypertension be managed?
|
PreHTN = SBP 120-139, DBP 80-89
- if pts SBP is >130 or DBP >80 and has DM, Chronic Kidney Disease, end organ damage, or cardiovascular disease then medical management with an antihypertensive agent is indicated -if none of the above comorbidities, then non-pharmacologic management with weight reduction, sodium restriction, increased physical activity, and avoidance of excess alcohol |
|
|
What blood pressure range is considered pre-HTN?
|
SBP 120-139
DBP = 80-89 management: weight loss decrease salt intake decrease alcohol increase exercise |
|
|
How many consecutive abnormally high readings are needed before prescribing BP medications?
|
3
|
|
|
What is the typical first line agent prescribed in treating newly diagnosed HTN?
|
Thiazide diuretics (HCTZ & chlorthalidone)
|
|
|
what is the chemical that increases as a result of ACE inhibitors, and is though to cause the adverse effects of cough & angioedema?
|

bradykinin
|
|
|
Which BP medication should all DM, CHF, and post-MI pts take as part of their BP regimen?
|
ACE inhibitor or ARB
|
|
|
Which antihypertensive can cause first dose orthostatic hypotension?
|
alpha-blockers
|
|
|
Which antihypertensive can cause hypertrichosis?
|
minoxidil (Rogaine)
|
|
|
Which antihypertensive can cause dry mouth, sedation, severe rebound hypertension?
|
Clonidine
|
|
|
Which antihypertensive can cause bradycardia, impotence, asthma exacerbation?
|
non-selective beta-blockers
|
|
|
Which antihypertensive can cause reflex tachycardia?
|
Nitroprusside (vasodilator)
|
|
|
Which antihypertensive can cause cough?
|
ACE Inhibitors
|
|
|
Which antihypertensive should be avoided in pts with sulfa allergies?
|
Thiazide & loop diuretics
|
|
|
Which antihypertensive can cause angioedema?
|
ACE Inhibitors
|
|
|
Which antihypertensive can cause drug-induced lupus?
|
Hydralazine
|
|
|
Which antihypertensive can cause cyanide toxicity?
|
nitroprusside
|
|
|
which antihypertensives can be used in pregnancy?
|
labetalol, methyldopa, hydralazine, nifedipine
|
|
|
What tests can be used to diagnose renal artery stenosis?
|
Renal arteriogram - gold standard, but invasive
MRA of renal arteries - most freq used screening test Renal artery duplex scan - capable of detecting bilateral renal artery stenosis (unlike CT or MRA) but time consuming (2 hrs) and must have well-trained operator Helical CT of renal arteries with IV contrast Captopril renal ultrasound |
|
|
What is the most common cause of secondary HTN?
|
Renal disease (renal artery stenosis, chronic renal disease, end stage renal disease)
|
|
|
What can be offered as an alternative contraceptive to a woman whose current estrogen-containing OCPs are causing HTN?
|
Progestin-only methods (progestin-only pills, DepoProvera, Implanon, Mirena)
|
|
|
Hypoperfusion and resultant tissue ischemia are the concern in shock pts. What is the chemical marker of this?
|
elevated lactic acid level
|
|
|
What is the mechanism behind cardiogenic shock?
|
failure of the pump
|
|
|
What is the mechanism behind extra-cardiogenic shock?
|
compression of the pump (tension pneumothorax, massive hemothorax, cardiac tamponade)
|
|
|
What is the mechanism behind hypovolemic shock?
|
not enough fluid to pump
|
|
|
What is the mechanism behind anaphylactic shock?
|
widespread vasodilation & release of vasodilatory agent in response to allergen
|
|
|
What is the mechanism behind neurogenic shock?
|
widespread vasodilation & loss of autonomic regulated vascular tone
|
|
|
What is the mechanism behind septic shock?
|
widespread vasodilation & massive release of inflammatory mediators
|
|
|
HTN + depression + kidney stones
Dx? |
hyperparathyroidism
|
|
|
What complication can arise from the use of vasopressors such as norepinephrine (NE) in treating shock?
|
peripheral vasoconstriction & ischemia (finers & toes, mesenteric ischemia, renal failure)
|
|
|
What intervention is most effective at reducing blood pressure?
|
weight loss
|
|
|
What is the preferred initial antihypertensive in a pt with no comorbidities?
|
Thiazide diuretic
|
|
|
Which anti-HTN is first line in pts with diabetes
|
ACE inhibitor/ ARB
|
|
|
Which anti-HTN is first line in pts with BPH
|
alpha-blockers
|
|
|
Which anti-HTN is first line in pts with heart failure
|
ACE Inhibitor/ ARB,
beta-blocker Aldosterone Antagonists |
|
|
Which anti-HTN is first line in pts with left ventricular hypertrophy
|
ACE inhibitor/ ARB
|
|
|
Which anti-HTN is first line in pts with hyperthyroidism
|
Propanolol
|
|
|
Which anti-HTN is first line in pts with osteoporosis
|
Thiazide diuretics
|
|
|
Which anti-HTN is first line in pts with benign essential tremor
|
beta-blocker
|
|
|
Which anti-HTN is first line in post-menopausal females?
|
thiazide diuretics
loops lose Calcium, thiazides dont |
|
|
Which anti-HTN is first line in pts with migraines?
|
beta-blockers
|
|
|
HTN measures in arms but low BP in lower extremity
What is the most likely cause of HTN? |
coarctation of aorta
|
|
|
What is the most likely cause of HTN?
pt found to have proteinuria |
renal disease
|
|
|
What is the most likely cause of secondary HTN with the follow finding:
hypokalemia |
hyperaldosteronism
|
|
|
tachycardia + diarrhea + heat intolerance
What is the most likely cause of HTN? |
hyperthyroidism
|
|
|
What is the most likely cause of secondary HTN with the follow finding:
hyperkalemia |
renal failure or renal artery stenosis
|
|
|
pt has episodes of excessive sweating + tachycardia
What is the most likely cause of HTN? |
pheochromocytoma
|
|
|
oompare the vasodilating effects of:
Nitroglycerin Dihydropyridine CCBs Hydralazine Nitroprusside |
Nitroglycerin = venous vasodilator
Dihydropyridine CCBs = dilates both arteries & veins Hydralazine = arterial vasodilator Nitroprusside = dilates both arteries & veins |
|
|
What are the HACEK bacteria?
|
Haemophilus
Actinobacillus Cardiobacterium Eikenella Kingella |
|
|
What are the indications for the repair of AAA to prevent future rupture?
|
Diameter > 5.5cm
↑ in diameter by more than .5cm in a 6mo interval (should be receiving abd sono q 6mos) symptomatic (ie tenderness, pain in abdomen or back) |
|
|
What is the w/u for a pt with peripheral artery disease (PAD) considering surgical corrections?
|
Generally the steps of surgical evaluation for PVD are as follows: physical exam → ankle-brachial index (ABI) (to confirm diagnosis) → segmental pressures and/or LE duplex/Doppler (to determine lesion location, morphology) → lower extremity arteriogram (to map the disease extent and locations in order to determine the best tx option) → surgery
Cardiac stress test prior to surgery b/c pts are likely to also have CAD needing intervention prior to PAD surgery |
|
|
What are the components of medical, conservative management of peripheral artery disease (PAD)?
|
Smoking cessation; Glucose & BP control
Daily exercise to ↑ collateral flow Cilostazol (pletal) 100mg BID to improve flow to LE and ↓claudication. It is better than pentoxifylline (Trental) 400mg tid. Contraindicated if any heart failure due to ↑mortality. Aspirin or Plavix qd to ↓ cardiovascular events Statin therapy to ↓ cardio events and ↑ pain-free walking distance Other possibly effective therapies: Trental (2nd line to Pletal) Ginko biloba Not Effective: Vit E |
|
|
What options are available to treat varicose veins?
|
Weight reduction, avoidance of prolonged stockings, leg elevation
Compression stockings: OTC support stockings, Class I stockings (20-30mmHg), or Class II stockings (30-40mmHg) Sclerotherapy: injection of substance directly into the vein that causes injury & thrombosis Surgery: involving ligation of the long sphenous vein or short saphenous vein |
|
|
What is an Unna boot, and when is its used indication?
|
Inelastic banadage that is impregnanted with zinc oxide paste + calamine lotion + glycerine + gelatin
Indicated for ulcer arising from chronic venous insufficiency Pts preder to use hydrocolloid dressing that can be changed at home q5-7 days instead of the Unna boot which must be placed by trained personnel q1-3wks. The effectiveness in ulcer healing is the same for both |
|
|
What are the different methods available for the primary prevention of DVT?
|

|
|
|
What is the treatment for superficial thrombophlebitis?
|

|
|
|
What study should be ordered for a pt suspected of having an Abdominal aortic aneurysm (AAA)?
|
Ultrasound of the abdomen
|
|
|
What are recommendations for screening for AAA with u/s?
|
All males btw the ages of 65-75yrs with any h/o smoking & men ages 65-75 yrs who have never smoked but who have a 1st degree relative who required repair of AAA or died from ruptured AAA
|
|
|
What are the first recommendations to pts with claudication besides medication optimization?
|
Stop smoking, ↑ exercise/walking
If these fail, consider surgical option |
|
|
What are several methods to prevent DVTs in hospitalized pts?
|
Place SCDs
Ambulate Anticoagulate – Enoxaparin/ Heparin or warfarin |
|
|
What should be ordered in a pt suspected of having a DVT?
|
D-dimer (good for ruling out)
Bilateral lower extremity duplex U/S |
|
|
A pt comes to the ER following a MVC and CXR reveals a widened mediastinum. What imaging would confirm dx?
|
Contrast CT scan of the chest
|
|
|
How is Kawasaki’s disease diagnosed?
|
“CRASH & burn”
Conjunctivitis – bilateral, nonexudative, painless Rash - truncal Adenopathy- of the cervical lymph nodes Strawberry tongue – and diffuse mucus membrane erythema Hands & feet have edema with induration, erythema & desquamation Fever > 5 days (>40C or 104°F) Note: coronary artery aneurysms can occur w/in weeks of the illness onset, but are not indicated in diagnostic criteria |
|
|
How is Kawasaki’s disease treated?
|
IVIG (2g/kg over 8-12 hrs) – ideally w/in the first 10 days
High-dose aspirin (80-100mg/kg/day in 4 divided doses) in the acute phase of the illness continued until 48hrs after fever resolution, followed by low-dose aspirin (3-5 mg/kg/day) until inflammatory markers (ESR, platelets) return to normal (usually 6 weeks) (steroids are not indicated and are of no proven benefit) Echocardiogram in the acute phase & 6-8 wks later |
|
|
A 55yo F presents with c/o new headache, jaw claudication, and tenderness of the temporal artery. What test will reveal dx? What is the treatment?
|
Dx: Temporal artery biopsy
Tx: steroids & aspirin |
|
|
Why should steroids be started immediately in pts in which you have a high suspicion of temporal arteritis?
|
Prevent vision loss
|
|
|
35 yo Japanese-American F has fever, malaise, and ↓ carotid & limb pulses. What will be seen on radiology? Biopsy?
|
Radiology: defects along the aorta & its branches
Biopsy: fibrosis, giant cells, plasma cells & lymphocytes w/in the media & adventitia of affected vessels |
|
|
A known asthmatic develops ↑ fatigue, fever & rash. What vasculitis might she have? What might be seen on blood tests?
|
Dx: Churgg-Strauss
Blood tests: ↑ serum eosinophils, ↑ ESR, (+) pANCA |
|
|
What are the signs & symptoms of Kawasaki disease?
|
“CRASH & burn”
Conjunctivitis, Rash, Adenopathy, Strawberry tongue Hands & feet have edema with induration, erythema & desquamation Fever > 5 days |
|
|
What is the tx for Kawasaki disease? What complication is the treatment trying to prevent?
|
Tx: Aspirin + IVIG, trying to prevent aneurysms
|
|
|
What is the treatment for ventricular septal defects?
|

|
|
|
What are the characteristics of Ebstein’s Anomaly?
|
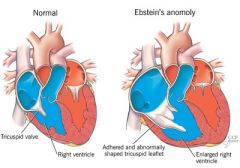
a/w maternal Lithium use
Tricuspid Leaflets are displaced into right ventricle, hypoplastic right ventricle, tricuspid regurg or stenosis 80% have a patent foramen ovale with R → L shunt Dilated right atrium = ↑ risk of SVT & WPW Exam: widely split S2, tricuspid regurgitation Tx: PGE, digoxin, diuresis, propanolol for SVT |
|
|
What are the unique structures of the fetal circulation that close after birth?
|
Umbilical vein, umbilical arteries (2)
Ductus arteriosus, ductus venosus Foramen ovale |
|
|
HYQ: What medication is used to close a PDA?
|
Indomethacin
Note: Prostaglandin E keeps it open think: to open the door, you gotta "push it, push it real good" (Push/Prost) |
|
|
A newbown is found to have a congenital heart disease that causes early cyanosis. What drug does this newborn need?
|
Prostaglandin E
|
|
|
What is the most common congenital heart defect?
|
VSD
|
|
|
Describe briefly the sequence of events in Eisenmenger’s syndrome:
|
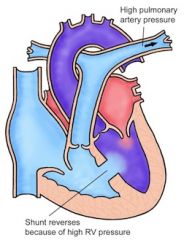
L to R shunt → ↑ blood in pulmonary vasculature, ↑ resistance → shunt reverses R to L
|
|
|
What are the abnormalities a/w Tetrology of Fallot?
|
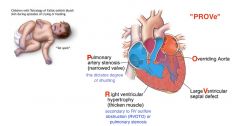
VSD, overriding aorta, RVH, RV outflow obstruction/stenosis of pulmonary artery
|
|
|
What heart defect are Down syndrome pts at higher risk for?
|
Endocardial cushion defect
|
|
|
HYQ: 6wk old infant presents to the pediatric ER for irritability & is found to have signs of left-sided heart failure. An EKG is interpreted as a left-sided MI. What is the most likely dx?
|
Anomalous origin of the left coronary artery
Arises from the pulmonary artery rather than the aorta & carries deoxygenated blood |
|
|
HYQ: What class of medications is indicated in pts with a hereditary prolongation of the QT interval in order to prevent episode of ventricular fibrillation?
|
β-blockers (propanolol)
|
|
|
What type of vasculitis:
Weak pulses in upper extremity |
Takayasu’s
|
|
|
Necrotizing granulomas of lung & necrotizing glomerulonephritis
|

Wegener's
|
|
|
Necrotizing immune complex inflammation of visceral/ renal vessels in young male smokers
|
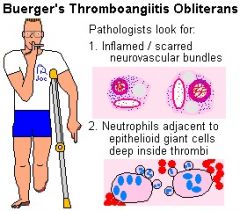
Buerger’s
|
|
|
What type of vasculitis is seen with young asthmatics?
|
Churg-Strauss
|
|
|
What type of vasculitis is seen in Infants & young children; involves coronary arteries
|
Kawasaki
|
|
|
Most common vasculitis
|
Temporal (Giant cell) arteritis
|
|
|
what type of vasculitis is assoc with hep B infection
|
Polyarteritis nodosa
|
|
|
In which type of vasculitis can you see occlusion of ophthalmic artery that can lead to blindness?
|
Temporal (giant cell) arteritis
|
|
|
Perforation of nasal septum
|

Wegener's
|
|
|
Unilateral headache, jaw claudication
|
Temporal (giant cell) arteritis
|
|
|
What is the next step in the management of a pt with a DVT that has a high likelihood of falling?
|
IVC filter
|
|
|
What are the components of the medical management of peripheral artery disease (PAD)?
|
Smoking cessation
↑ exercise glucose control diet BP control Cilostazol |
|
|
What are the indications for operating on an AAA?
|
Size >5.5 cm
Rate of increase > 0.5cm in 6 mos Symptomatic |
|
|
Who should be screened for an abdominal aortic aneurysm?
|
All males btw the ages of 65-75yrs with any h/o smoking & men ages 65-75 yrs who have never smoked but who have a 1st degree relative who required repair of AAA or died from ruptured AAA
|
|
|
What are some of the complications/ reactions that can arise from blood transfusions?
|

|
|
|
In a Swan-Ganz catheter (pulmonary artery catheter), the wedge pressure is equal to what?
|
Left atrial pressure
|
|
|
Which blood products replace clotting factors?
|
FFP, Cryoprecipitate, Whole blood
Clotting factors from donors Recombinant factors, Autologus blood |
|
|
A pt is brought to the ER s/p MVA. It appears he has sustained blunt trauma & is hypOtensive. You immediately order a type & cross and start IVF. The pt is found to be type O neg so the lab sends up 6units of AB+ pRBCs. What is the next step?
|
Send it back! He needs O neg blood
|
|

For what indications would you use the following?
|
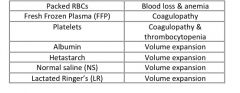
|
|
|
What is the cause of acute hemolytic transfusion reaction? Anaphylactic reaction?
|
Acute hemorlytic: ABO incompatibility
Anaphylactic: anti-IgA IgG Abs react in IgA deficient pts |
|
|
What are some agents used to treat shock due to a weakly beating heart?
|
Dopamine, Dobutamine, Epinephrine, Isoproterenol, Norepinephrine
|
|
|
What commonly used agents cause peripheral vasoconstriction?
|
Norepinephrine, Vasopressin, Epinephrine, Phenylephrine
|
|
|
What medications are used to treat febrile & urticarial transfusion reactions?
|
Acetominophen & Diphenhydramine
|
|
|
What is the typical ER lab work-up for a pt with acute abdominal pain?
|
CBC with differential
Chem 14 β-hCG if female urinalysis amylase, lipase stool guaiac |
|
|
What are the signs & symptoms of acute mesenteric ischemia?
|
Sudden onset of severe abdominal pain (periumbilical) that is OUT OF PROPORTION TO THE EXAM
Vomiting & diarrhea Condition that could cause emboli formation (ie atrial fibrillation) Early exam: mostly normal, abdominal distention +/- occult blood on stool Late exam (bowel infarction): abdominal distention, absent bowel sounds, peritoneal signs, feculent odor to the breath |
|
|
What is the treatment for acute mesenteric ischemia?
|

|
|
|
What are the classic signs/symptoms of chronic mesenteric ischemia?
|
Aka intestinal angina
Dull, crampy, postprandial epigastric pain within the first hour after eating then subsiding over 2 hrs Weight loss (due to food aversion to avoid postprandial pain) Possibly nausea, vomiting, and early satiety Abdominal bruit (50%) |
|
|
What are the treatment option for chronic mesenteric ischemia?
|
Bypass, endarterectomy, angioplasty
|
|
|
Which oral hypoglycemia medicine should NOT be given when a pt is to have a radiologic procedure in which he will need IV contrast?
|
Metformin
Note: metformin + contrast dye → lactic acidosis |
|
|
A patient taking warfarin chronically for a h/o thromboembolism requires surgery. What can be given in the perioperative period to keep the patient anticoagulated?
|
Heparin or LMWH
|
|
|
What are the 5 W’s of post-operative fever? To what do they refer?
|
Wind – atelectasis / pneumonia
Water – UTI (foley catheter) Walking – DVT / PE Wound – wound infection Wonder drugs – drug reaction “Wein” (Vein) – thrombophlebitis, DVT also think sinusitis if NG tube in place |
|
|
What studies are ordered to evaluate the cause of a fever in a postop patient?
|
CXR, UA, urine culture, blood cultures
Sputum culture, wound culture |
|
|
What is used to evaluate patients that may have a lower extremity DVT?
|
D-dimer and/or bilateral lower extremity ultrasound
|
|
|
What should be prescribed to abdominal post-op patients to help reduce atelectasis?
|
Incentive spirometry
Deep breathing exercises Physical therapy +/- bronchodilators & inhaled steroids |
|
|
Other notes:
|
LMWH should NOT be restarted until at least 2 hrs after removal of epidural catheter to avoid epidural hematoma
Renal protective measures: Hydration, IV bicarb, NAC (n-acetylcysteine) |
|
|
Clean-contaminated wounds involve an incision through disinfected skin & would involve one or more of the following structures?
|
GI tract, respiratory tract, vagina
|
|
|
What is seen on abdominal x-ray or CT scan that indicates a ruptured viscus?
|
Free air (radiolucent/ black)
|
|
|
What is the classic finding in the abdominal exam of a patient with mesenteric ischemia?
|
Pain out of proportion to the exam
|
|
|
During a surgical procedure, the anesthesiologist notices that the patient’s temperature has climbed quickly and her muscles are rigid. Recognizing this feared complication, the doctor should administer which medicine?
|
Dantrolene (think malignant hyperthermia)
|
|
|
What are a few contraindications to the transplant of the following organs?
|
Heart – smoking, pulmonary hypertension
Lung – smoking, poor cardiac/liver/renal failure Liver – alcoholism, multiple suicide attempts |
|
|
What is the type of rejection that is treatable with immunosuppressive agents? What is the mechanism of this rejection? Within what time frame may it show up?
|
Acute rejection
|
|
|
What is the usual lab panel ordered in a pt presenting to the ER with generalized abdominal pain?
|
CBC with differential, Chem 8 / BMP, LFTs, Urine analysis
β-hCG (if female) stool guaiac amylase, lipase EKG & cardiac enzymes if > 45 yrs old |
|
|
What is the usual time frame for stopping warfarin prior to surgery?
|
3 – 4 days prior to surgery
|
|
|
What interventions are helpful in optimizing lung function in the post-op period in patients with pre-existing lung disease?
|
Incentive spirometry
Pain control Deep breathing Physical therapy Bronchodilators Inhaled steroids |
|
|
What type of immunodeficiency increases the risk of anaphylactic transfusion reaction?
|
IgA deficiency
|
|
|
What lab findings suggest hepatic disease during a pre-op work-up?
|
↑ PT/PTT
↓ platelets ↑ bilirubin ↑ or ↓ transaminases ↓ albumin |
|
|
What are the preferred vessels in the placement of a Swan-Ganz catheter?
|
Right IJ or Left Subclavian
|
|
|
When is the greatest risk for a post-operative MI? What is recommended perioperatively for pts with known CAD?
|
With in first 48 hrs
Telemetry monitoring |
|
|
Which vasopressor matches the following statement?
|
you forgot to fill this in
|
|
|
Which blood product is most appropriate in the following scenarios?
|
you forgot to fill this in
|

