![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
279 Cards in this Set
- Front
- Back
|
what is the treatment for an MI due to cocaine overdose?
|
Note: don’t use β-blockers! (don’t want to block the β-2 vasodilation, which would lead to ↑ vasoconstriction)
Tx: Lorazepam (Ativan), Ca2+ channel blockers Management: Rule out CAD if pt >35 yrs |
|
|
In which immunodeficiency is there an absence of a thymic shadow on newborn CXR?
|
(1) DiGeorge Syndrome
(2) Severe Combined Immunodeficiency (SCID) (Most commonly due to Adenosine Deaminase (ADA) def) |
|
|
A post-op patient has poor UOP, BUN 85, creatinine of 3, and clear lungs. what is the next step in the management of this pt?
|
anytime you see a BUN:Cr >20, think dehydration or pre-renal azotemia
(azotemia is a term for elevated BUN & Cr, azotemia can become uremia if there are symptoms present) next step = IV fluids |
|
|
Which vaccines should not be given to a HIV (+) pt?
Which vaccines can be given? |
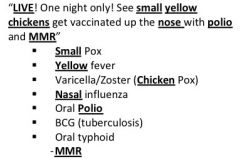
Live virus vaccines = Varicella/ Zoster, Intranasal influenza, Oral polio, Yellow fever, BCG (tuberculosis), Anthrax, Oral typhoid, Small pox
Exception: can give MMR, if: -No evidence of immunity -CD4 ct >200 -No AIDS-defining condition Vaccines that you can give to HIV (+) pts: -IM influenza -Hepatitis B -S. pneumoniae -Hepatitis A (For MSM) |
|
|
When would you suspect thrombocytopenia due to heparin use? What is the most feared complication of heparin-induced thrombocytopenia?
|
Suspect HIT anytime platelets drop by at least 50% in a patient on heparin
Complication of HIT: thrombosis |
|
|
What is the next step in the management of a child with severe asthma exacerbation and persistently low oxygen saturation despite medication?
|
-Give O2
Indications for intubation in children with asthma: - Unable to maintain oxygen saturation despite supplementation -altered mental status -unable to speak due to work of breathing |
|
|
What is the classic presentation of a pt with androgen insensitivity syndrome?
|
Normal appearing female
Rudimentary vagina Absent uterus Absent fallopian tubes Testosterone present High testosterone, estrogen & LH |
|
|
What is the most common foodborne bacterial GI tract infection?
|
salmonella
|
|
|
What is the classic presentation of a pt with hyperprolactinemia?
|
For women, it depends whether they are pre- or post-menopausal:
Premenopausal female: Galactorrhea, Hypogonadism (Infertility, Oligo- or amenorrhea) Post-menopausal: Already hypogonadal, +/- galatorrhea Male: ↓ testosterone: ↓ libido, impotence, ↓ sperm ct, gynecomastia, +/- galactorrhea |
|
|
What lab changes will be seen in a pt with hyperaldosteronemia?
|
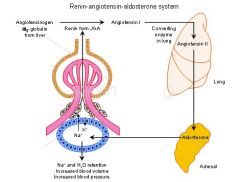
Think of spironolactone side effects (b/c this drug inhibits aldosterone):
Hypokalemia Mildly ↑ Na+ Metabolic alkalosis ↑ 24 hr urine aldosterone |
|
what is the antidote for the following type of overdose?
|
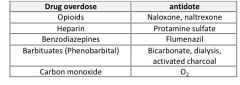
see above
|
|
|
What type of oral contraceptive can be given to lactating women?
|
Progestin-ONLY pills
|
|
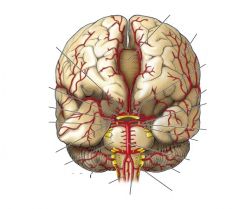
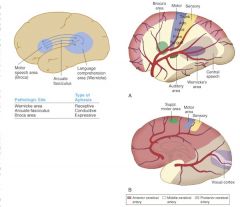
label the arteries & brain structures
|
see above
|
|
|
What is the definition of primary amenorrhea?
|
Absence of menses at age 16 in the presence of normal growth & 2° sex characteristics
Absence of menses by age 13 without 2° sex characteristics |
|

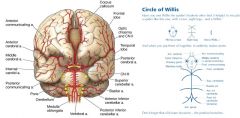
Label the Circle of Willis
|
see above, also pg 170
|
|
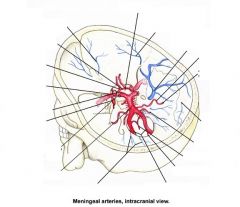
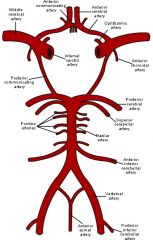
Label the Circle of Willis, intracranial view
|
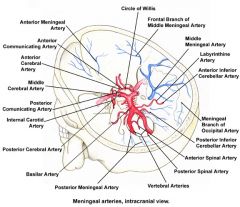
see above, also pg 170
|
|
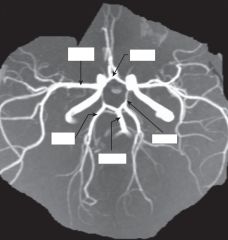
Magnetic resonance arteriography illustrating the circle of Willis and its branches
|
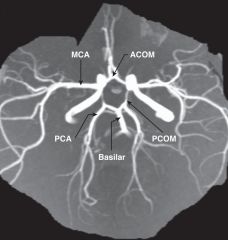
see labels above
|
|

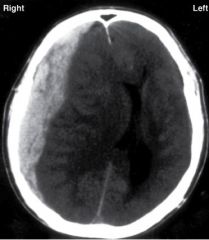
What do you see?
|
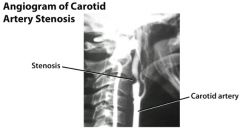
Lateral common carotid arteriogram in a patient with a neck bruit. Note the focal narrowing of the proximal internal carotid artery (arrow). In severe cases, the kink may require carotid artery reconstruction.
DIT says that you need to be able to recognize a stenosis vs aneurysm |
|
What do you see?
|
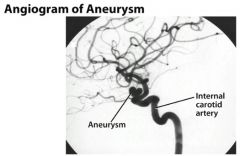
Left oblique cerebral angiogram in a patient with multiple intracranial aneurysms shows an anterior communicating aneurysm and a middle cerebral artery aneurysm. The patient underwent a frontotemporoparietal craniotomy, during which surgical clips were placed in both lesions in one setting.
DIT says that you need to be able to recognize the difference btw an aneurysm and arterial stenosis on an angiogram |
|
what do you see?
|
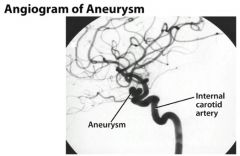
(from Medscape): Left oblique cerebral angiogram in a patient with a proximal intracranial internal carotid artery aneurysm. The surgical approach to this aneurysm requires a craniotomy with an orbitotomy and drilling of the anterior clinoid process; however, this aneurysm has a favorable neck-to-fundus ratio for endovascular coil placement.
DIT says that you need to be able to recognize the difference btw aneurysm & stenosis on angiogram imaging |
|

A 49yo, presents with sudden onset of vertigo, nausea, vomiting, dysphagia, hoarseness, and nystagmus in addition to ipsilateral Horner syndrome, limb ataxia, and impairment of all sensory modalities over the face. There is also impairment of pinprick and temperature appreciation in the contralateral limbs.
|

This case illustrates the development of the lateral medullary syndrome (Wallenberg's syndrome) as a result of occlusion of the posterior inferior cerebellar artery (PICA).
-Loss of pain & temp over contralateral body -Loss of pain & temp over ipsilateral face -Cerebellar defects - Involvement of the sympathetic pathways may lead to Horner's syndrome - Vertigo results from involvement of the vestibular nuclei and hemiataxia from involvement of the inferior cerebellar peduncle. |
|
|
What viruses preferentially infect the ventral horn of spinal cord, leading to a flaccid paralysis?
|
polio & west nile
|
|
|
Which spinal tract carries touch, vibration, and pressure sensation?
|
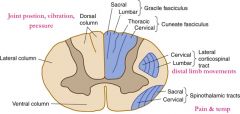
Dorsal columns:
Fasciculus gracilis & cuneatus |
|
|
Which spinal tract carries voluntary motor commands from motor cortex to body?
|

Lateral & ventral corticospinal tracts
|
|
|
Which spinal tract carries voluntary motor commands from motor cortex to head/neck?
|
Corticobulbar tract
|
|
|
Which spinal tract carries pain & temp sensation?
|
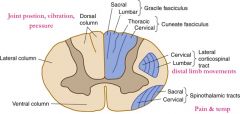
Lateral spinothalamic tract
|
|
|
Which spinal tract is important for postural adjustments & head mvmts?
|

Vestibulospinal tract
|
|
|
Which CN is responsible for Eyelid opening?
How do you differentiate between benign & serious cause of deficit of this nerve? |
CN 3 (oculomoter)
Benign cause (ie HTN or Diabetes) of CNIII palsy - the pupil will be normal in size & reactive - no treatment is needed Serious causes (ie aneurysm, tumor, or uncal herniation) - pupil will be dilated & nonreactive ("blown") - urgent CT/MRI is needed |
|
|
Which CN is responsible for
Taste from ant 2/3 of tongue? What other sxs would you look for to distinguish whether the damage to this nerve was UMN or LMN? |
CN 7 (Facial)
UMN lesion of Facial nerve = forehead is spared on the affected side, cause is usually stroke or tumor LMN lesion of Facial nerve = forehead is involved, and cause is usually Bell's palsy or tumor |
|
|
Which CN is responsible for
Head turning? How do you know which side the lesion is located? |
CN 11 (spinal accessory)
Patients with CN 11 lesions have trouble turning their head to the side OPPOSITE the lesion & have ipsilateral shoulder droop (due to loss of innervation to SCM & trapezius) |
|
|
Which CN is responsible for
Tongue movement? How do you know which side the lesion is located? |
CN 12 (hypoglossal)
protruded tongue will deviate to the SAME side of the lesion |
|
|
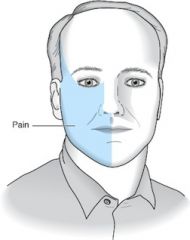
Which CN is responsible for
Muscles of Mastication? What pathological condition of this nerve is provoked by chewing? |
CN 5 (trigeminal) - also innervates facial sensation
Trigeminal Neuralgia ("Tic doulourex") = unilateral shooting pains in the face & often triggered by chewing, brushing the teeth - tx with Carbamazepine |
|
|
Which CN is responsible for balance?
Kids with balance probs - likely cause is? Adults with balance probs - likely cause? |
CN 8 (Vestibulocochlear) - needed for hearing & balance
Lesions of CN 8 can cause deafness, tinnitus, and/or vertigo - in kids, think of meningitis as a cause in adults - think of medications (aspirin, aminoglycosides, loop diuretics, cisplatin), infection (labyrinthitis, tumor, or stroke |
|
|
Which CN is responsible for monitoring carotid body & sinus chemoreceptors & baroreceptors?
|
CN 9 (glossopharyngeal)
|
|
|
What are the 2 most common locations of aneurysms in the Circle of Willis?
|
Anterior communicating artery
Posterior communicating artery |
|
|
Where is the brain lesion if pt presents with:
contralateral hemiballismus |

subthalamic nucleus
|
|
|
Where is the brain lesion if pt presents with:
eyes look toward the side of the lesion |
frontal eye fields (Prefrontal cortex)
|
|
|
Where is the brain lesion if pt presents with:
eyes looking away from the side of the lesion |
PPRF
|
|
|
Where is the brain lesion if pt presents with:
paralysis of upward gaze |
Superior colliculi (Parinaud syndrome)
Also known as dorsal midbrain syndrome, this is a distinct supranuclear vertical gaze disorder caused by damage to the posterior commissure. It is a classic sign of hydrocephalus from aqueductal stenosis. Pineal region tumors, cysticercosis, and stroke also cause Parinaud's syndrome. Features include loss of upgaze (and sometimes downgaze), convergence-retraction nystagmus on attempted upgaze, downward ocular deviation ("setting sun" sign), lid retraction (Collier's sign), skew deviation, pseudoabducens palsy, and light-near dissociation of the pupils. |
|
|
Where is the brain lesion if pt presents with:
hemispatial neglect syndrome |
non-dominant parietal lobe
|
|
|
Where is the brain lesion if pt presents with:
coma |
reticular activating system (RAS) - in the ventral pons
likely a/w Basilar Artery occlusion |
|
|
Where is the brain lesion if pt presents with:
poor repetition |
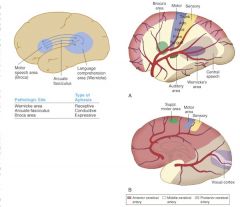
arcuate fasciculus
|
|
|
Where is the brain lesion if pt presents with:
poor comprehension |
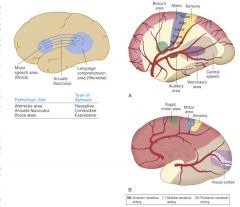
Wernicke's area
|
|
|
Where is the brain lesion if pt presents with:
poor vocal expression |
Broca's area
|
|
|
Where is the brain lesion if pt presents with:
resting tremor - think of the classic "pill rolling" tremor that disappears with movement or sleep What conditions cause a resting tremor? |

basal ganglia (↓ dopamine)- think Parkinson's Disease
Other conditions other than Parkinson's disease that can cause resting tremors: - hyperthyroidism, anxiety - tx with Beta blockers - Drug withdrawal or intoxication (MPTP found in designer drugs) Or Antipsychotics used to treat Schizophrenia - treat this side-effect with anticholinergics (benztropine, trihexyphenidyl) or antihistamines (diphenhydramine) - benign hereditary tremor - usually Aut Dom (look for fam hx) Also beware of: Wilson's disease (hepatolenticular degeneration) - causes chore-like movements Liver failure - causes asterixis (slow, involuntary flapping of outstretched hands |
|
|
Where is the brain lesion if pt presents with:
intention tremor |
cerebellar hemisphere
this is why alcoholics will have INTENTION tremors |
|
|
Where is the brain lesion if pt presents with:
hypororality, hypersexuality, disinhibited behavior |
bilateral amygdala (Kluver-Bucy)
|
|
|
Where is the brain lesion if pt presents with:
Personality changes - apathy, inattention, disinhibition, labile affect |
frontal lobe
|
|
|
Where is the brain lesion if pt presents with:
dysarthria (trouble articulating words - slurred speech) |
cerebellar vermis - this is why alcoholics have slurred speech
|
|
|
Where is the brain lesion if pt presents with:
agraphia & acalculia inability to read, write, name or do math |
dominant (left) parietal lobe
|
|
|
Where do the dorsal columns decussate?
|

medulla
recall the dorsal columns carry touch, vibration, pressure sensation |
|
|
where does the lateral corticospinal tract decussate?
|
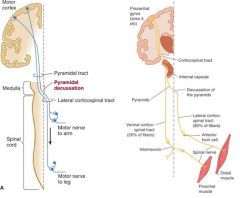
medullary pyramids
|
|
|
Where does the spinothalamic tract decussate (crossover)?
|
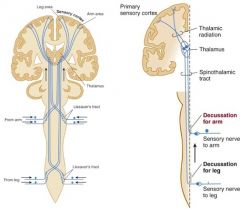
Anterior white commissure at the spinal cord level
spinothalamic carries pain & temperature sensation correlation: syringomyelia, in which there is central cavitation of the spinal cord (usually in cervical or upper thoracic region) presents with loss of pain & temp sensation in a "cape" distribution b/c damage to the lateral spinothalamic tracts MRI is best test to diagnose, tx with surgical creation of a shunt |
|
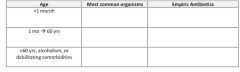
fill out this chart - 4star topic!!
what are the common organisms and empiric IV antibiotic choices for bacterial meningitis based on age of the patient? |

see above
|
|
|
What is the rational for dosing dexamethasone prior to or along with the first dose of antibiotics for empiric treatment of bacterial meningitis?
|
Dexamethasone when given with or prior to the first dose of antibiotic reduces the risk of neurologic sequelae (ie hearing loss) in children with meningitis, esp in the cases of H. influenza Type B or Tuberculosis (TB) meningitis
In adults with bacterial mengingitis, dexamethasone reduces both morbidity and mortality esp in the case of pneumococcal meningitis |
|
|
Do you always need to get a CT scan (prior to an LP) if you suspect meningitis?
|
No – you do not have to get a CT scan in a patient you suspect of having meningitis
|
|
|
In which situations do you need to get a CT scan prior to an LP?
|
Focal neurologic defects
Papilledema Pupil asymmetry Suspect hematoma Suspect brain tumor |
|
|
What is the treatment for viral meningitis?
|
Acetominophen for pain
IV fluids as needed Empiric antibiotics until bacterial meningitis can be excluded if younger than 3 yrs, severely ill, or immunocompromised, continue empiric antibiotics until bacterial culture results confirm nonbacterial etiology *** Give empiric Acyclovir if suspicion of HSV or signs of encephalitis such as focal neurologic findings d/c if HSV PCR and cultures are negative or alternative diagnosis is made |
|
|
An infant is brought to the ER. The parents say that over the last day the infant has developed a fever, refused to eat, vomited, and is lethargic. The PE reveals petechiae and confirms the fever. WBC is elevated, and CSF results show a ↓ glucose and ↑ neutrophils. On which medications should this patient be started?
|
Cover: E. coli, Listeria, Group B Strep (GBS)
Tx: Ampicillin + cefotaxime Ampicillin + gentamicin |
|
|
What other drug should be given just before or along with the first dose of antibiotics in a pt suspected of having bacterial meningitis?
|
Dexamethasone
|
|
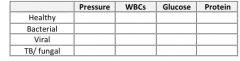
Fill in the table of CSF findings in cases of meningitis caused by different types of pathogens:
|
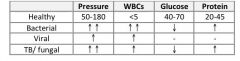
Think: Bacterial eat sugar, viruses increase protein a little but noting else, TB/fungis same as bacteria
|
|
|
When should a CT scan be performed as a next step instead of an LP in a pt suspected of having meningitis?
|
When there are signs of ↑ ICP or other comorbidity
Focal neurologic defect Papilledema Focal seizure Suspicion of mass effect Soft tissue infection at site of LP Bleeding diathesis Cardiopulmonary instability |
|
|
You suspect an AIDS pt may have meningitis. What specific CSF preparation should be ordered in addition to the usual CSF analysis, gram stain, and culture?
|
India Ink stain to look for Cryptococcus meningitis
|
|
|
When would you suspect West Nile Viral infection? How would you make the dx? what's the tx?
|
Birds are the resevoir, and mosquitoes are the vectors. Human, horses, and dogs are incidental hosts
S/S: usually only headache, malaise, back pain, myalgia, and anorexia for 3-6 days (“flu like”) Severe S/S in 1/150: meningitis +/- encephalitis including muscle weakness and flaccid paralysis (via anterior-horn involvement), alteration in consciousness, possibly death Dx: serology – check for IgM Abs against West Nile Virus Tx: supportive |
|
|
What is the treatment for Reye's syndrome?
|
d/c salicyclate (ie Aspirin)
Hospitalization (usually ICU) for cardiorespiratory monitoring (+/- mechanical ventilation), supportive care, fluid & electrolyte management Maintain euglycemia: accuchecks, IV dextrose or insulin as needed Maintain isovolemia: IVF or Lasix as needed, Foley catheter for strict I/Os Reduce brain swelling: avoid hypo-osmotic fluids, elevate head of bed, +/- corticosteroids, +/- ICP monitor If seizures: phenytoin |
|
|
How should you treat a pt that has been bitten by an animal suspected of having rabies, or an animal that cannot be observed for 10 days?
|
Clean the wound with iodine
Administer rabies immunoglobulin & rabies vaccine Tetanus prophylaxis |
|
|
A pt is brought into the ED with progressive muscle weakness, intact sensation, headache, vomiting, neck pain, and fever. CSF analysis shows ↑ lymphocytes and normal glucose and protein. What life-threatening complication can result in this disease process?
|
Dx: Polio (muscle weakness is key to dx)
Complication: respiratory muscle paralysis |
|
|
What other term should you remember when considering Reye’s syndrome?
|
Hepatoencephalitis
|
|
|
A pt is recovering in the ICU after suffering a subdural hematoma that occurred b/c of a MVC. The neurosurgery team performed a craniotomy and drain placement to evacuate the clot. For the past few days the drainage in the collection bulb was serous. Now however, the drainage is thick and yellow. Along with this, the pt’s neurological exam has deteriorated. What is the likely cause of this clinical picture?
|
Dx: abscess within subdural space
Likely etiology: Staph aureus Tx: cover for MRSA, gram (+) and Gram negs with Vancomycin and Ceftazidime |
|
|
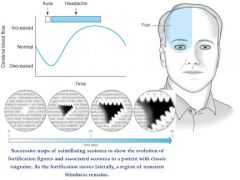
What are the differences in the acute treatment of tension headaches, cluster headaches, and migraine headaches?
|
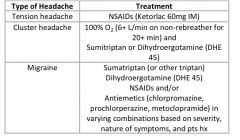
see above
|
|
|
What agents can be used for prophylaxis of migraine headaches?
|
Ca2+ channel blockers: verapamil (often first-line b/c safe and well tolerated)
β-blockers: propanolol, metoprolol (good choice if comorbid HTN) Tricyclic antidepressants (TCA): amitriptyline, nortriptyline (good choice if comorbid depression, incsomnia, pain syndrome) Note – nortriptyline has fewer side effects NSAIDs: naproxen (good choice if menstrual migraine or comorbid osteoarthritis or other pain that could benefit from NSAIDs) Anticonvulsants: valproic acid (good if h/o Bipolar disorder), topiramate, gabapentin |
|
|
What is the most likely cause of a pt's headache if:
Made worse by foods containing tyramine |
migraine
|
|
|
What is the most likely cause of a pt's headache if:
Obese female with papilledema |
pseudotumor cerebri
|
|
|
What is the most likely cause of a pt's headache if:
Jaw muscle pain when chewing |
Giant cell (temporal) arteritis
|
|

What is the most likely cause of a pt's headache if:
Periorbital pain with ptosis and miosis |
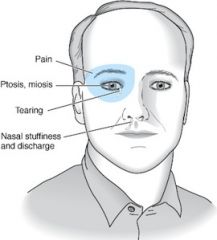
cluster headache
|
|
|
What is the most likely cause of a pt's headache if:
Photophobia, Phonophobia |
migraine
|
|
|
What is the most likely cause of a pt's headache if:
Bilateral frontal/ occipital pressure |
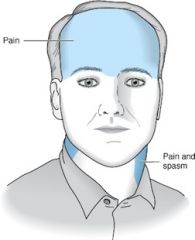
tension headache
|
|
|
What is the most likely cause of a pt's headache if:
Lacrimation and/or rhinorrhea |
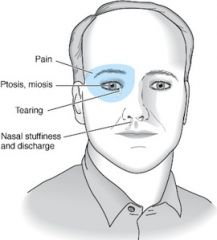
cluster headache
|
|
|
What is the most likely cause of a pt's headache if:
Elevated ESR |
Giant cell (temporal) arteritis
|
|
|
What is the most likely cause of a pt's headache if pt states:
“Worst headache of my life” |
Subarachnoid hemorrhage
|
|
|
What is the most likely cause of a pt's headache if:
Headache + extraocular muscle palsies |
Cavernous sinus thrombosis
|
|
|
What is the most likely cause of a pt's headache if:
Scintillating scotomas prior to headache |
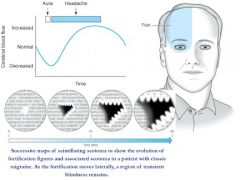
Migraine with aura
|
|
|
What is the most likely cause of a pt's headache if:
Headache occurring either before or after orgasm |
Post-coital cephalgia
|
|
|
What is the most likely cause of a pt's headache if:
Responsive to 100% Oxygen supplementation |
cluster headache
|
|
|
What is the most likely cause of a pt's headache if:
Trauma to the head → headache begins days after the event, persists for over a week and does not go away |
Subdural hematoma
|
|
|
What headache symptoms would lead you to suspect a brain tumor as a cause of a headache?
|
mild headache which progressively worsens over days to weeks
new onset after age 50 Papilledema: worsened by a bending, lifting, cough, or Valsalva maneuver (= ↑ in ICP) Associated seizures, confusion, altered mental status (AMS) Abnormal neurologic signs and symptoms (ie focal numbness or weakness) Disturbs sleep or present immediately upon awakening Vomiting precedes headache Known systemic illness (ie cancer, HIV, or collagen-vascular disorder) |
|
|
What are the characteristic features of pseudotumor cerebri?
|
Young, obese female
Headaches – daily (worse in the morning), pulsatile, possible nausea/vomiting, possible retroocular pain worsened by eye movement Papilledema Most worrisome sequela is vision loss CT Scan: (normal) no ventricular dilation, no mass CSF pressure elevated > 200 mmH2O in non-obese, >250 in obese pt) |
|
|
What treatment options are available for managing pseudotumor cerebri?
|
Confirm absence of other pathology with CT and MRI of the head (r/o central venous thrombosis)
d/c any inciting agents (ie Vit A excess, tetracyclines, withdrawal from corticosteroids) Weight loss in obese pts Acetozolamide – first line (start 250mg qid or 00mg bid → increase to 500mg qid to 1000mg qid) Invasive treament options: Serial lumbar punctures Optic nerve sheath decompression Lumboperitoneal shunting (CSF shunt) |
|
|
A 25 yo M is seen in the ER with a severe headache. He tells you that the headache always occurs at around the same time of day, and that the pain is localized around the right eye. On exam his pupils are unequal and his right eye is tearing. While he waits for a CT scan of the head, what treatment should he receive?
|
Dx: cluster headache
Tx: 100% O2, Sumitriptan or IV ergotamines |
|
|
30 yo F is in the office with a complaint of facial pain. She describes that whenever her face is lightly touches that she experiences incredible electricity-like pain. What is the 1st line therapy for this condition?
|
Dx: Trigeminal neuralgia
Tx: Carbamazepine or Baclofen |
|
|
27 yo M comes to the clinic b/c of progressively worsening headache. He denies a prior h/o headaches. He adds that this one was easy to ignore at first, but over the last few weeks has never let up and is increasing in severity. What should be next for this pt?
|
next step: MRI of brain (if it’s getting worse, be worried!)
|
|
|
What are the demographic characteristics of a typical pseudotumor cerebri patient?
|
obese female in 20's-30's
|
|
|
A pt with longstanding poorly-controlled diabetes has tension headaches. What should you check before recommending pharmacologic treatment?
|
Kidney function (Creatinine, BUN, GFR) – because NSAIDs are treatment for Tension Headaches
|
|
|
Which spinal cord lesion matches the following description?
Fasciculations but also spastic paralysis |
ALS
|
|
|
Which spinal cord lesion matches the following description?
Impaired proprioception + pupils do not react to light |
Syphilis (Tabes Dorsalis & Argyll Robinson pupils)
|
|
|
Which spinal cord lesion matches the following description?
Bilateral loss of pain and temp below lesion + hand weakness |

Syringomyelia
|
|
|
Which spinal cord lesion matches the following description?
Bilateral loss of vibration sense + spastic paralysis of legs then arms |
Vit B12 Deficiency
|
|
|
Which spinal cord lesion matches the following description?
Bilateral loss of pain/temp below lesion + bilateral spastic paralysis below lesion + bilateral flaccid paralysis at level of lesion |

Occlusion of Anterior Spinal Artery
|
|
|
What are the characteristic features of Brown-Sequard syndrome?
|
Ipsilateral vibration & discrimination below lesion
Ipsilateral spastic paralysis (below lesion) Ipsilateral flaccid paralysis (level of lesion) Contralateral pain & temp (below lesion) |
|
|
HYQ: most likely cause of headache in a 40yo woman with frontal headache that is made worse by bending over?
|
Sinus headache
|
|
|
HYQ: What would be the preferred antihypertensive in a pt with chronic hypertension and recurrent migraines?
|
β-blockers or Ca2+ channel blockers
|
|
|
HYQ: What medication should be given to close contacts of those with either meningococcal or HIB meningitis?
|
Rifampin or Ciprofloxacin
|
|
|
HYQ: What are the four most common sequelae of meningitis in children?
|
Hearing loss
Mental retardation Seizure disorder Spastic paralysis |
|
|
What is the treatment for fungal meningitis?
|
Amphotericin B
|
|
|
What medications are used in combination in the treatment of TB meningitis?
|
RIPE – Rifampin, Isoniazid, Pyrazinamide, Ethambutol
|
|
|
What cerebral artery infarct can cause aphasia?
|
MCA infarction
|
|
|
What organism is responsible for bacterial meningitis given the following findings on CSF examination?
Gram (+) diplococci |
Streptococcus pneumoniae
|
|
|
What organism is responsible for bacterial meningitis given the following findings on CSF examination?
Gram neg diplococci |
Neisseria meningitis
|
|
|
What organism is responsible for bacterial meningitis given the following findings on CSF examination?
Small pleomorphic gram neg coccobacilli |
Haemophilus influenza
|
|
|
What organism is responsible for bacterial meningitis given the following findings on CSF examination?
Gram (+) rods and coccobacilli |
Listeria
|
|
|
What is the anticoagulant of choice in a pt with a h/o stroke or TIA?
|
First TIA ➔ Aspirin
TIA/stroke due to Atrial Fibrillation ➔ Warfarin TIA/Stroke + coronary artery disease ➔ Clopidogrel (Plavix) Repeat TIA/stroke while on aspirin ➔ Clopidogrel (Plavix) |
|
|
What are the classic signs and symptoms of carotid artery stenosis?
|
Carotid bruit
Transient ischemic attacks (TIAs) Reversible ischemic neurologic deficits lasting up to 3 days Amaurosis fugax (transient unilateral blindness) Cerebrovascular accidents (CVAs) (Vertigo & Syncope are NOT caused by carotid artery stenosis) |
|
|
What are the surgical indications for carotid endarterectomy?
|
Symptomatic carotid stenosis 70-99%: strong benefit
Symptomatic carotid stenosis 50-69%: marginal benefit (more benefit in men and if performed w/in 2 wks of stroke/TIA) Asymptomatic pts with 80-99% stenosis who are expected to live longer than 5 yrs by a surgeon with a perioperative complication rate of less than 3% (some books will mention a blanket >60% and asymptomatic rule, but this varies by surgeon and patient) |
|
|
What are the important nonsurgical treatments for carotid artery stenosis?
|
HTN control to < 140/90
Dyslipidemia control to LDL < 100mg/dL, HDL >35, TGs <200 Lipid control with statin reduces stroke while other lipid lowering drugs do not Niacin reduces carotid artery intima thickness ADA diet DM control to fasting glucose <126 and HgA1c <7% Smoking avoidance, consider varenicline (Chantix) ↑ physical activity to at least 30-60 minutes 4x weekly alcohol consumption up to 2 drinks daily is beneficial. Avoidance of heavy drinking Evaluation for CAD and PAD Aspirin Anticoagulation if history of TIA/stroke while on aspirin → use Aggrenox or clopidogrel instead |
|
|
What are some major signs and symptoms of a TIA?
|
Amaurosis fugax (brief unilateral blindness)
Weakness Slurred speech Impaired coordination Impaired sensation/ paresthesias |
|
|
What anticoagulant would you give a pt who has just had their first TIA? What if the pt had another TIA while on ASA, what would you add?
|
First TIA: Aspirin
Second TIA, while on Aspirin: add Clopidogrel (Plavix) or combination of Aspirin + dipyridamole |
|
|
What is the maximum amt of time a TIA may last?
|
24 hrs or less
|
|
|
What medication should be taken by a pt with atherosclerotic disease and risk of stroke?
|
Statin & Aspirin
|
|
|
What are the indications for carotid endarterectomy?
|
Asymptomatic men with narrowing of 80-99%
Symptomatic men with narrowing of 50-69% Symptomatic women with narrowing of 70-99% |
|
|
What are the 5 main lacunar syndromes that may arise from a lacunar infarct?
|
1) Pure motor hemiparesis: (most common, about 50% of lacunar strokes) – weakness of the face, arm, and leg on one side of the body + absent sensory or cortical signs (aphasia, neglect, apraxia, hemianopsia)
2) Pure sensory: sensory defect (numbness) of the face, arm, and leg on one side of the body + absent motor or cortical signs 3) Ataxic hemiparesis: ipsilateral weakness and limb ataxia out of proportion to the motor defect, possible gait deviation to the affected side + absent cortical signs 4) Sensory motor stroke: weakness and numbness of the face, arm, and leg on one side of the body + absent cortical signs 5) Dysarthria – Clumsy Hand Syndrome: (least common) – facial weakness, dysarthria, dysphagia, and slight weakness and clumsiness of one hand + absent sensory or cortical signs |
|
|
A stroke, by definition, must last how long?
|
> 24 hrs
|
|
|
What thrombolytics are used in the treatment of an acute ischemic stroke?
|
tPA, streptokinase (streptase)
|
|
|
What long-term medications should be started within 2-3 days of ischemic stroke?
|
Antiplatelet (aspirin) + statin
|
|
|
What would be the most likely initial imaging for a pt suspected to have a stroke?
|
Noncontrast CT scan
then, If the above study did not yield useful information, then what study might you get? MRI of the head |
|
|
What is the next step in management of a pt with ischemic stroke symptoms after a hemorrhagic stroke has been ruled out by noncontrast CT?
|
Thrombolytic therapy
|
|
|
To maintain cerebral perfusion during the acute treatment of ischemic stroke, hypertension is generally not actively treated. At what blood pressure does treatment become necessary?
|
BP > 220/120
|
|
|
Hemorrhagic stroke requires the following treatment:
|
Reversal of any anticoagulation
Control of intracranial pressure (ICP) Control of blood pressure Surgical decompression may be needed |
|
|
What is the treatment for a subarachnoid hemorrhage?
|
d/c all anticoagulants and reverse and anticoagulation
systolic BP < 150 only if cognitive function is intact (adequate cerebral perfusion pressure) until the aneursm is clipped or coiled to prevent rebleeding. If the cerebral perfusion pressure is not adequate then lowering the BP will increase the risk of infarction Labetalol preferred Avoid Nitroprusside & Nitroglycerin which can ↑ ICP Nimodipine (a CCB) to prevent vasospasm Prevent physiologic derangements that may worsen brain injury Avoid hypoxia and hyperglycemia Maintain a normal pH, euvolemia, and normothermia (Phenytoin for seizure prophylaxis is controversial and generally avoided due to poorer outcomes) Ventriculostomy to monitor ICP in select patients Surgical clipping or metal coil into aneurysm |
|
|
Are patients with parenchymal hemorrhage at an increased risk of seizures?
|
yes
|
|
|
In which scenario is seizure prophylaxis with anticonvulsants recommended? Parenchymal hemorrhage or subarachnoid hemorrhage (SAH)?
|
Parenchymal → always start prophylaxis
SAH → only if seizures develop |
|
|
How can AVMs and/or aneurysms be treated?
|
Coil or clip
|
|
|
What diseases are associated with berry aneurysms?
|
Polycystic Kidney Disease
Marfan’s Syndrome |
|
|
What are 3 feared complications of parenchymal hemorrhage?
|
Uncal herniation
CSF flow obstruction Death |
|
|
How may a pt describe the symptom of a subarachnoid hemorrhage?
|
"worst headache of my life"
|
|
|
What 2 studies must be performed to rule out SAH?
|
Noncontrast CT scan of the head
Lumbar puncture |
|
|
How does one differentiate between SAH and a traumatic LP as a cause of bloody CSF?
|
collect several tubes of CSF, if blood decreases then more likely due to traumatic LP than SAH
|
|
|
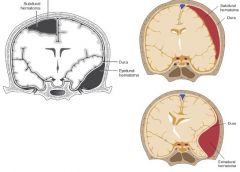
What are the most common causes of an epidural hematoma and subdural hematoma?
|
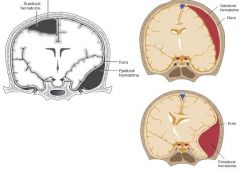
Epidural hematoma: rupture of middle meningeal artery
Subdural hematoma: rupture of bridging veins |
|
|
Commonly a pt with an epidural hematoma will have the typical three part history of:
|
(1) head trauma with brief LOC
(2) Lucid interval (3) Deterioration (expansion of epidural hematoma) |
|
|
What is the definitive treatment of an epidural hematoma?
|
Evacuation of hematoma
|
|
|
Where is the bleeding in a subdural hematoma? What shape would be expected on a head CT of a pt with subdural hematoma?
|
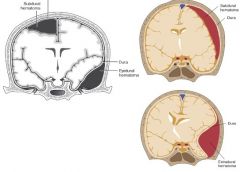
Bleeding is btw dura & arachnoid
Classic finding: crescent shape on CT scan |
|
|
If you suspect a pt has an epidural or subdural hematoma, should you perform a LP to confirm the diagnosis?
|
NO! can ↑ risk of brain herniation
|
|
|
Describe the differences between Broca’s aphasia and Wernicke’s aphasia?
|
Broca’s: expressive
Wernicke’s: receptive |
|
|
What are the three Ws that help diagnose normal pressure hydrocephalus?
|
Wacky – cognitive impairment
Wet – incontinence Wobbly – gait disturbance |
|
|
Which medications or medication withdrawal are known for causing seizures?
|
Medications that ↓ seizure threshold:
Buproprione Buspirone Enflurane Medication withdrawals that can cause seizures: Barbiturates Alcohol Anticonvulsants Benzodiazepines - choose the short acting (Alprazolam, Lorazepam) if given more than one to choose from |
|
|
What medications are used for prevention of grand mal (tonic-clonic) seizures?
|
Valproate, carbamazepine, phenytoin, lamotrigine, topiramate
|
|
|
What medications are used for prevention of partial seizures?
|
(same as prevention of grand mal seizures)
Carbamazepine, Phenytoin, Lamotrigine > Valproate, Topiramate |
|
|
What medications are used for prevention of absence seizures?
|
Ethosuximide
|
|
|
What seizure medications are used for prevention of myoclonic seizures?
|
Valproic Acid
|
|
|
Which seizure medication matches the following description?
Gingival hyperplasia |
phenytoin (Dilantin)
|
|
|
Which seizure medication matches the following description?
DOC for absence seizures |
Ethosuximide (Zarontin)
|
|
|
Which seizure medication matches the following description?
2nd choice for absence seizures |
Valproic Acid (Depakene)
|
|
|
Which seizure medication matches the following description?
DOC for Trigeminal Neuralgia |
carbamazepine
|
|
|
Which drugs are known for causing Stevens-Johnson syndrome?
|
“sulfa, -cillin & seizure”
most commonly lamotrigine (lamictal) |
|
|
Which drugs are known for inducing the cytochrome P450 system thereby speeding up the metabolism of other drugs such as OCPs and warfarin?
|
“BCG PQRS”
Barbiturates Carbamazepine Griseofulvin Phenytoin Quinidine Rifampin St John’s Wort |
|
|
what is Arnold-Chiari Malformation?
|
Downward displacement of the cerebellar tonsils and medulla thru the foramen magnum
Type I is the most common type and is often asymptomatic. Manifestations may include headaches and/or cerebellar symptoms Type II (of IV severity) is usually accompanied by other neurologic anomalies |
|
|
What other neurologic anomalies are associated with an Arnold-Chiari malformation?
|
Hydrocephalus
Syringomyelia Myelomeningocele |
|
|
What are some of the possible presenting features of cerebral palsy?
|
Spastic features: spastic paresis of any or all limbs, clonus present
Athetosis features: slow, writhing movements in distal muscles Chorea features: rapid, irregular, unpredictable contractions of muscles in face or extremities Dystonic features: uncontrollable jerking, writhing, or posturing Infants have persistence of primitive reflexes, involuntary grimacing, tendency to drool, and delayed psychomotor development Ataxia: difficulty coordinating purposeful movements Atonic features: severe hypotonia present at birth with no future ability to stand or walk Neonates: may show signs of encephalopathy including lethargy, ↓ spontaneous movement, hypotonia, and suppressed primitive reflexes Associated disorders: mental retardation, epilepsy, sensory impairment (speech, hearing, vision) |
|
|
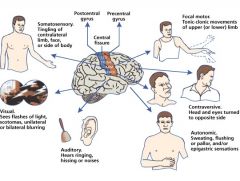
What type of seizure fits each description?
Focal sensory or motor deficit with no loss of consciousness |
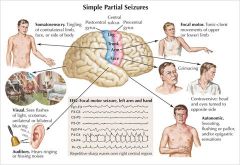
simple partial
|
|
|
What type of seizure fits each description?
Focal sensory or motor deficit, with impaired consciousness (commonly localized to temporal lobe on EEG) |
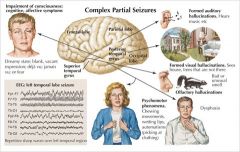
Complex partial
|
|
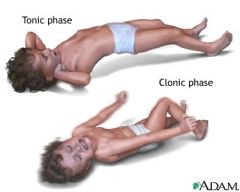
What type of seizure fits each description?
Involves both hemispheres of brain with a pattern of neuromuscular activation: tonic, clonic, toni-clonic, myoclonic, or atonic. Loss of consciousness present with postictal period |
Generalized
|
|
|
What type of seizure fits each description?
Characterized by a brief (few second) impairment of consciousness often with automatisms such as blinking or picking at shirt. No postictal period. Spike and wave pattern on EEG |
Absence
|
|
|
What is status epilepticus?
|
Uninterrupted seizure > 20min
|
|
|
What is the initial treatment for a pt in status epilepticus?
|
Monitor ABCs
|
|
|
Once ABCs are under control, what is the treatment for a pt in status epilepticus?
|
IV Benzos - Lorazepam
|
|
|
What is the DOC for absence seizures?
|
Ethosuximide
|
|
|
A 45yo M is brought to the ER for new-onset status epilepticus. What are some of the components of the workup to determine epilepsy?
|
Hx & PE (ask about trauma, drugs, illness)
CBC Fasting blood glucose BMP & LFTs Toxic drug screen CT head (if not actively seizing… ) LP for CSF infection (r/o meningitis) |
|
|
How long must a focal neurologic deficit last to qualify as a stroke?
|
> 24 hrs
|
|
|
In what timeframe must thrombolytic therapy be instituted in cases of ischemic stroke?
|
Within 3 hrs
|
|
|
HYQ: What is the treatment for an epidural hematoma or subdural hematoma?
|
Evacuation of the hematoma via surgical drainage
|
|
|
HYQ: Most common predisposing consition for an intracranial hemorrhage?
|
hypertension
|
|
|
HYQ: What is the principle cause of a lacunar infarct?
|
hypertension
|
|
HYQ: CT Scan of the head shows a cresent shaped lesion. What event most likely caused this lesion?
|
Subdural hematoma → blunt head trauma, rupture of bridging veins
|
|
|
HYQ: What is the preferred treatment for febrile seizures?
|
Acetominophen or ibuprofen (No Aspirin)
Reassure parents |
|
|
HYQ: A patient with a DVT develops a stroke. What study would most would most likely identify the underlying etiology of the stroke?
|
Transesophageal echocardiogram (TEE)
|
|
|
What neurologic defects would be seen with an infarction of anterior cerebral artery
|
Contralateral loss of sensory and/or motor information
Legs, feet, trunk |
|
|
What neurologic defects would be seen with an infarction of middle cerebral artery (MCA)
|
Loss of sensory and/or motor info in hands, face, arms
Aphasia: Broca’s, Wernicke’s, Conduction, global |
|
|
What neurologic defects would be seen with an infarction of posterior cerebral artery
|
Visual defects: unilateral hemaniopia, macular sparing
|
|
|
What neurologic defects would be seen with an infarction of lacunar arteries?
|
one of the lacunar syndromes:
Pure motor hemiparesis Pure sensory stroke Ataxic hemiparesis Sensorimotor stroke Dysarthria – Clumsy hand syndrome |
|
|
What neurologic defects would be seen with an infarction of the basilar artery?
|
Cranial nerve abnormalities
|
|
|
What are the 5 main lacunar syndromes that may arise from a lacunar infarct?
|
Pure motor hemiparesis
Pure sensory stroke Ataxic hemiparesis Sensorimotor stroke Dysarthria – Clumsy hand syndrome |
|
|
An aphasic patient has great trouble producing words but understands everything you say. What type of aphasia does he most likely have?
|
Broca’s aphasia
|
|
|
Although benzodiazepines are used to end a seizure in status epilepticus, what is of more concern in the initial treatment?
|
Monitor ABCs
|
|
|
What is the treatment for subarachnoid hemorrhage?
|
Stop anticoagulants
BP < 150 (Labetalol) Avoid nitroprusside/ nitroglycerin etc |
|
|
What neurotransitter changes do you see with anxiety disorders?
|
↑ NE ↓ 5-HT ↓ GABA
think - aNxiety due to excess Norepinephrine |
|
|
What neurotransitter changes do you see with depression?
|
↓ NE ↓ Dopamine ↓ Serotonin
think: Depression = all Down (plus, this is why SSRIs, SNRI & MOAIs all work in treating depression) |
|
|
What neurotransitter changes do you see with mania?
|
↑ NE ↑ 5-HT
|
|
|
What neurotransitter changes do you see with Alzheimer's?
|
↓ ACh
|
|
|
What neurotransitter changes do you see with Huntington's Disease?
|
↓ ACh ↓ GABA
|
|
|
What neurotransitter changes do you see with Schizophrenia?
|
↑ Dopamine
|
|
|
What neurotransitter changes do you see with Parkinson's Disease?
|
↓ Dopa ↑ ACh
|
|
|
At what point does grief/bereavement become pathological?
|
Grief becomes pathological when any of the following present:
● Depression criteria met for at least 2 weeks after the first 2 months following the loss ● Generalized feelings of hopelessness, helplessness, worthlessness ● Guilt ● Distressed feelings do not diminish in intensity by suicidal ideation ● Inability to move-on, trust others, and reengage in life by 6 months |
|
|
What medical conditions can cause severe depression?
|
hypOthyroidism
hyperparathyroidism Parkinson’s disease Stroke, CNS tumors Pancreatic cancer |
|
|
What medications are known for causing symptoms of depression in patients?
|
● Sedatives: alcohol, benzos, antihistamines
● Stimulant withdrawal ● ** Methyldopa (Aldomet) – antihypertensive often used for HTN in pregnancy ● 1st Gen antipsychotics (ie Haloperidol) ● anti-nausea drugs including metoclopramide (Reglan) and prochlorperazine (compazine) ● ** Glucocorticoids ● Insufficient thyroid replacement → hypothyroidism ● ** α-interferon – used in viral hepatitis treatment |
|
|
What scale can be used to determine a pt’s risk of suicide?
|
SAD-PERSONS Scale
(S)ex - men are 3x more likely to complete suicide, Give 1 pt for being male (A)ge: suicide is more likely if <!9 or >45. Give 1 pt if age not btw 19-45 yr old (D)epression: depression greatly increases risk. Give 1 pt if mood is significantly depressed. (P)rior attempts: Give 1 pt for one of more prior attempts (E)tOH: intoxication ↑ risk. Give 1 pt for alcohol or drug dependent (R)ational thought process: give 1 pt for significant psychotic symptoms (S)upport lacking: give 1 pt if pt does not have significant sources of emotional & social support (O)rganized plan: give 1 pt if pt articulates an organized plan for suicide (more than simple ideation or impulses) (N)o spouse: Give 1 pt if family support unavailable (can be family members other than spouse (S)ickness: give 1 pt for other medical problems that are not well controlled and that are a source of distress Guidelines for Action: - 0-2 pts → outpt f/u, assist with arrangements - 3-4 pts → supervised/ supported outpt f/u; consider admission for some pts - 5-6 pts → consider hospitalization unless safe alternative can be arranged and verified - 7-10 pts → generally will require hospitalization. May need commitment involuntary |
|
|
What are some symptoms of atypical depression? What medications work well for atypical depression?
|
S/S: Hypersomnia (↑ sleep), Leaden paralysis/ psychomotor retardation, hyperphagia (weight gain), hypersensitivity to rejection
Tx: MAOIs better than TCAs |
|
|
What is the first line treatment for seasonal affective disorder?
|
Phototherapy
Drugs – SSRIs, bupropion |
|
|
Depression has what neurotransmitter derangements?
|
↓ NE ↓ Dopamine ↓ Serotonin
|
|
|
List the symptoms of depression:
|
“SIG E CAPS”
Sleep disturbance Interest/pleasure reduction Guilt feelings or thoughts of worthlessness Energy changes/fatigue Concentration/attention impairment Appetite change Psychomotor disturbances Suicidal thoughts |
|
|
Diagnosis of major depressive disorder (MDD) requires 5 of the above symptoms including depressed mood or anhedonia that must last how long?
|
> 2 weeks
|
|
|
What is the diagnosis of a pt that has periods of mood disturbances while psychotic as well as periods of psychosis with normal affect?
|
Schizoaffective disorder
|
|
|
What medical conditions can cause severe depression?
|
hypOthyroidism, hyperparathyroidism, Parkinson’s Disease
Stroke, CNS neoplasm, Pancreatic cancer |
|
|
List the Selective Serotonin Reuptake Inhibitors (SSRIs)
|
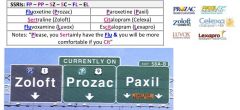
Fluoxetine (Prozac), Sertraline (Zoloft)
Paroxetine (Paxil) Citalopram (Celexa) Fluvoxamine (Luvox, Lescol) Escitalopram (Lexapro) |
|
|
List the Tricyclic Antidepressants (TCAs)
|

Amitriptyline (Elavil), Imipramine (Tofranil)
Desipramine (Norpramin) Nortriptyline (Aventyl) Clomipramine (Anafranil) Doxepin (Silenor, Sinequan) |
|
|
List the Monoamine
|
Phenelzine (Nardil)
Tranylcypromine (Parnate) Selegiline (Eldepryl, Emsam, Zelapar) |
|
|
List the dopamine-norepinephrine reuptake inhibitors (NDRIs)
|

Buproprion (wellbutrin)
|
|
|
List the selective serotonin-norepinephrine reuptake inhibitors (SNRIs)
|

Venlafaxine (Effexor, Pristiq)
Duloxetine (Cymbalta) Milnacipran (Savella) Nefazodone (Serzone) |
|
|
List the tetracyclic antidepressants (dual mode of action by enhancing both serotonergic & noradrenergic neurotransmission but not a reuptake inhibitor, plus histaminergic & alpha-adrenergic antagonist)
note: don't really need to know how they work, just that these drugs don't fit with any other group |
Mirtazapine (Remeron)
Trazodone (Desyrel, Oleptro) |
|
|
What drugs, when combined with SSRIs are known for causing Serotonin syndrome?
|
SSRIs, SNRIs, MAOIs
LSD, St. John’s wort, Levodopa, Meperidine, Lithium Amphetamines, cocaine, ectasy |
|
|
What are the characteristic features of serotonin syndrome?
|
● Mental status changes: anxiety, agitation, delirium, restlessness, disorientation
● Autonomic excitation: diaphoresis, tachycardia, hyperthermia, hypertension, vomiting, diarrhea ● Neuromuscular: tremor, muscle rigidity, myoclonus, hyperreflexia → Ocular clonus: slow, continuous, horizontal eye mvmts → Spontaneous or inducible clonus → Babinski signs bilaterally |
|
|
What is the treatment for serotonin syndrome?
|
(1) d/c serotonergic agents: symptoms usually resolve in 24hrs
(2) supportive care to normalize vital signs - oxygen, IVF, cardiac monitoring - if medical treatment for tachycardia or hypertension is needed, use short acting agents ie esmolol, nitroprusside - sedation with benzodiazepines - if temp > 41.1°C → sedation, paralysis, and ET tube → mechanical COOLING (ie ice, cooling blankets, misting fans) - PARALYSIS should relieve the hyperthermia which is caused by muscle activity - there’s no benefit in using antipyretics in this case - if AGITATION despite benzos → Serotonin antagonist - after resolution of symptoms, assess need to resume serotonergic agent |
|
|
What evaluation should take place prior to the initiation of TCAs in children?
|
b/c TCAs can cause arrhythmias, the following is needed:
● Screen the pt's family history for heart disease, palpitations, syncope, near syncope ● Screen family history for SUDDEN DEATH prior to age 40, long QT syndrome, arrhythmias, and hypertrophic cardiomyopathy ● EKG prior to initiation and again when medication is optimized |
|
|
What are the symptoms of overdose with tricyclic antidepressants (TCAs)?
Amitriptyline (Elavil), Imipramine (Tofranil) Desipramine (Norpramin) Nortriptyline (Aventyl) Clomipramine (Anafranil) Doxepin (Silenor, Sinequan) |

● Cardiotoxicity: tachycardia, hypotension, conduction abnormalities
● CNS toxicity: sedation, obtundation, coma, seizures ● Anticholinergic symptoms: mydriasis, xerostomia, ileus, urinary retention |
|
|
How is TCA overdose managed?
|
● ABCs – Airway, Breathing, Circulation
● Activated charcoal 1g/kg up to 50kg (unless ileus is present) ● Continuous cardiac monitoring for at least 6 hrs → if no problems, then clear for psych eval ● Frequent neuro checks ● Lab/Studies: TCA level, Chem 7, EKG ● If ingestion < 2 hrs → gastric lavage ● If hypotension → IVF (LR or NS) → if ineffective, then norepinephrine ● If QRS > 100msec → trial Bicarb then infusion if effective ● If seizures → Benzos, barbiturates, and/or propofol (but not phenytoin which is ineffective against toxin-induced seizures) |
|
|
What food substances should be avoided when taking MAOIs in order to avoid a tyramine induced hypertensive crisis?
Phenelzine (Nardil) Tranylcypromine (Parnate) Selegiline (Eldepryl, Emsam, Zelapar) |
Foods that are spoiled, pickled, aged, smoked, fermented or marinated contain tyramine. The following foods should be avoided b/c of sufficient quantities of tyramine to be problematic while on MAOIs:
● Fermented cheeses (cream cheese & cottage cheese OK) ● Smoked or aged meats (sausage, bologna, pepperoni, salami, smoked or pickled fish) ● Chianti, most beers and wines (esp over 120mL) ● Soy sauce, shrimp paste, miso soup ● Sauerkraut, avocados ● Brewer’s yeast and yeast extracts (yeast used in baking is ok) |
|
|
In what group of pts is bupropion (Wellbutrin) contraindicated?
|
b/c of an ↑ risk of lowering the seizure threshold, bupropion should be avoided in pts with:
(1) seizure disorder (2) eating disorder (3) Benzo or alcohol withdrawal |
|
|
What are the indications for electroconvulsive therapy (ECT)?
|
Severe debilitating depression refractory to antidepressants
Psychotic depression Severe suicidality Depression with catatonic stupor Depression with food refusal leading to nutritional compromise Situations where a rapid antidepressant response is required (ie pregnancy) Previous good response to ECT Medical condition preventing the use of antidepressants (ie elderly patients) Bipolar disorder/mania Schizophrenia/psychosis (esp catatonic) |
|
|
How long must a pt expect to take an SSRI before they see improvement in their depression?
|
3-4weeks (maybe up to 6 wks)
|
|
|
In TCA overdose, what can be used to correct the prolonged QRS interval and possible seizures?
|
IV Bicarb for prolonged QRS interval
IV Benzodiazepines to end seizure |
|
|
Consumption of tyramine rich food in conjunction with MAOI treatment can result in what dangerous condition?
|
Hypertensive crisis
MOAIs = Phenelzine (Nardil) Tranylcypromine (Parnate) Selegiline (Eldepryl, Emsam, Zelapar) |
|
|
What food are known to be rich in tyramine?
|
“aged food” – cheese, wine, pizza
|
|
|
Trazodone’s side effect of sedation makes it useful in what population of pts who have difficulty sleeping?
|
Elderly
|
|
|
Which commonly used antidepressant should be avoided in pts at risk for seizure?
|
Buproprion
Contraindications: seizure disorder, eating disorder, Benzo or alcohol withdrawal |
|
|
Which antidepressant is preferred in the treatment of depression with comorbid neuropathic pain?
|

SNRIs – Duloxetine (Cymbalta)
|
|
|
What are the potential side effects of lithium use in the treatment of bipolar disorder?
|
(1) CNS depression, tremor, cognitive dulling
(2) Thyroid changes – hyper- or hypothyroidism, or euthyroid goiter (3) Nephrogenic diabetes insipidus – reversible on discontinuation → thirst, polydipsia, polyuria (4) GI side effects – nausea, vomiting, diarrhea, metallic taste changes, weight gain |
|
|
What is the treatment for nephrogenic diabetes insipidus caused by lithium toxicity?
|
Amiloride + hydrochlorothiazide
|
|
|
How is depression managed in pts with bipolar disorder?
|
● Mild depression → lithium or lamotrigine
● Moderate depression → add a second mood stabilizer (lamotrigine) or add an atypical antipsychotic (olanzapine, quetiapine, or risperidone) ● Lamotrigine has significant drug interactions with valproate and carbamazepine ● Adding an antidepressant to a mood stabilizer does not have proven effectiveness (NEJM 2007;356;1711) ● Severe depression → consider ECT |
|
|
What are the diagnostic criteria for adjustment disorder?
|
● Clinically significant emotional or behavioral reaction causing marked distress or impairment in social or occupational functioning
● Symptoms develop in response to an identifiable psychosocial stressor (ie divorce, failure at school, peer problems) other than bereavement ● Symptoms begin WITHIN 3 MONTHS of the stressor ● s/s disappear w/in 6mos of disappearance of the stressor ● If the stressor is chronic (ie ongoing parental conflict) then the disorder may last > 6mos and is termed chronic |
|
|
Concern about Benzos → What are the 7 D’s?:
|
(1) Depression of CNS
(2) Dependence (3) Disinhibition (4) Deficits in memory (5) Dizziness (6) Drug interactions (7) Dangerous |
|
|
Manic – “DIGFAST” stand for:
|
(D)istractibility
(I)nsomnia (G)randiosity (F)light of ideas (A)ctivity (S)peech (T)aking risks |
|
|
How is acute stress disorder different than posttraumatic stress disorder?
|
Acute stress: < 30days (1 month)
PTSD: > 30 days |
|
|
What are the treatment options for PTSD?
|
(1) Psychotherapy including behavioral (exposure) therapy and cognitive therapy
(2) SSRIs – first line (3) α-blockers (prazosin) improves nightmares & sleep disturbance Other antidepressants: TCAs (imipramine/amitriptyline), MAOIs (Benzodiazepines should be avoided in PTSD due to lack of efficacy and potential for abuse) Mood stabilizers (carbamazepine or valproate) improve impulsive behavior, arousal, and flashbacks atypical antipsychotics if refractory to other therapies |
|
|
What are 3 important distinctions of dysthymic disorder that distinguish it from MDD in making a diagnosis?
|
(1) Symptoms cannot include suicidal ideation
(2) Symptomatic for more than 2 yrs (3) No history of major depressive disorder (MDD) |
|
|
What is an imp diff btw manic episode & hypomanic one?
|
Manic episode: will significantly impair pts ability to function
|
|
|
What is the 1st line treatment for bipolar disorder?
|
Lithium
|
|
|
Should a bipolar pt who is treated with a mood stabilizer & has concurrent depression be started on an antidepressant?
|
No proven effectiveness in adding an antidepressant
|
|
|
Bereavement & adjustment disorder share similar time tables in a pt’s symptomatology. What are the key diff btw them?
|
Adjustment disorder impairs ability to function normally, bereavement does NOT
Adjustment d/o may be tied to stressors other than death |
|
|
What should be used for the long-term tx of Panic attacks?
|
SSRI
|
|
|
What is the antidote for benzodiazepine overdose?
|
Flumazenil
|
|
|
What are the diagnostic criteria for schizophrenia?
|
At least 2 of the following during 1 month period:
● Delusions (irrational belief that cannot be changed by rational argument) ● Hallucinations (most common type is auditory) ● Disorganized speech (ie freq derailment or incoherence) ● Grossly disorganized or catatonic behavior ● Negative symptoms (ie flat affect, poverty of speech, lack of emotional reactivity) (Only one of the above if required if delusions are bizarre or hallucinations consist of a voice keeping a running commentary on the person’s behavior or thoughts, or 2+ voices conversing with each other) Social / occupational dysfunction Duration of at least 6 months |
|
|
What is the difference btw the following disorders?
Schizotypal Schizophrenia Schizoaffective Schizoid Schizophreniform Brief psychotic d/o |
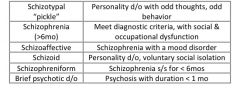
see above
|
|
|
What can you see on neuroimaging of a pt with schizophrenia?
|
Enlargement of ventricles & reduction in cortical volume
|
|
|
What is the difference btw schizophrenia & delusional d/o?
|
Delusional disorder → non-bizarre delusions, disorganized behavior, no hallucinations, no disorganized speech
|
|
|
What drugs are known to cause psychosis in pts?
|
LSD, PCP, Cocaine, amphetamines, steroids
Withdrawal from alcohol, benzos, barbiturates |
|
|
What are the high potency typical neuroleptics?
|
Haloperidol (Haldol)
Fluphenazine (Prolixin) Thiothixene (Navane) |
|
|
What are the low potency typical neuroleptics?
|
Chlorpromazine (Thorazine)
Thioridazine (Mellaril) Droperidol (Inapsine) |
|
|
What are the moderate potency typical neuroleptics?
|
Molindone, Loxapine,
Trifluoperazine, Perphenazine |
|
|
What are the atypical antipsychotics (second generation)
|

Olanzapine (Zyprexa),
Quetiapine (Seroquel) Risperidone (Risperdal) Clozapine (Clozaril) Aripiprazole (Abilify) Paliperidone (Invega) |
|
|
HYQ: A pt previously diagnosed with schizophrenia arrives at the Psych EF with a severe neck spasm that forces his head to be maintained in an unusual position. What’s the tx?
|
Dx: acute dystonia (torticollis in this case) due to antipsychotics
Tx: diphenhydramine (Benadryl) – anticholinergic |
|
|
What features characterize tardive dyskinesia that may develop from the use of high potency typical neuroleptics?
|
Choreoathetosis mvmts of tongue, face, neck, trunk or limbs
|
|
|
In what time frame would you expect to see Parkinsonian symptom side-effects in a pt taking antipsychotics?
|
4 days → 4 mos
|
|
|
What are the signs & symptoms of neuroleptic malignant syndrome (NMS)?
|
(1) Mental status change – initial symptom in most pts (agitated delirium with confusion rather than psychosis
(2) Muscular rigidity +/- tremor (3) Hyperthermia greater than 38-40°C (4) Autonomic instability – tachycardia, labile, or high BP, tachypnea, diaphoresis (5) Rhabdomyolysis appearing over 1-3 days |
|
|
What is the treatment for NMS?
|
● Stop the offending medication
● Supportive care in the ICU → IVF, lower fever with cooling blankets, ice packs in the axilla, Tylenol - Reduce HTN with clonidiine and/or nitroprusside ( → cutaneous vasodilation can facilitate cooling) - DVT prevention with heparin or lovenox - For agitation use benzos (clonazepam, lorazepam) ● Dantrolene → prevents rigidity & hyperpyrexia by inhibiting calcium release ● Other possible therapies: Bromocriptine, Amantidine (↑ Dopamine) |
|
|
What is the treatment for tardive dyskinesia?
|
Discontinue or decrease dose of neuroleptic
Consider switching to neuroleptic with less extrapyramidal side effects |
|
|
What is the treatment for Parkinsonian symptoms that have developed from neuroleptic administration?
|
Anticholinergics or Dopamine agonists (Bromocriptine, Amantidine)
|
|
|
Give examples of negative symptoms of schizophrenia
|
Social withdrawal, Flat affect, Apathy, Anhedonia, Avolition
|
|
|
By what mechanism do antipsychotic meds work?
|
Dopamine D2 receptors
|
|
|
What are some examples of extrapyramidal side effects?
|
Dystonia/ Parkinsonism
Tardive dyskinesia Neuroleptic Malignant syndrome |
|
|
What differentiates delusional disorder from schizophrenia or schizophreniform disorder?
|
In delusional disorder the delusions are plausible/ NON-bizarre
|
|
|
What is the tx of neuroleptic malignant syndrome (NMS)?
|
Stop the offending medication
Give Dantrolene Benzodiazepines |
|
|
What 2 side effects should a physician be aware of when using atypical antipsychotics?
|
Weight gain
New onset diabetes |
|
|
What side effects would you expect to develop with administration of thioridazine (Mellaril)?
|
Anticholinergic side effects (dry mouth… etc)
|
|
|
HYQ: what is the drug category of choice for the treatment of the negative symptoms of schizophrenia?
|
(+) symptoms → typicals
neg symptoms → atypicals |
|
|
HYQ: What is the DOC for bipolar disorder in a pt with renal failure?
|
Valproic acid or carbamazepine
|
|
|
HYQ: What is the treatment of choice for OCD?
|
1st line → SSRI
2nd line → clomipramine |
|
|
HYQ: A pt on haloperidol develops fever, muscle rigidity, confusion and diaphoresis. What is the DOC in the treatment of this pt’s condition?
|
Dx: Neuroleptic malignant syndrome (NMS)
Tx: Dantrolene |
|
|
HYQ: What is the most problematic congenital malformation a/w maternal lithium use?
|
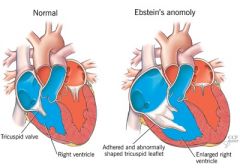
Ebstein’s anomaly
|
|
|
HYQ: What is the most common AE of olanzapine (zyprexa)?
|
weight gain
|
|
|
What are the symptoms of TCA overdose?
|
Cardiotoxicity, CNS toxicity, Anticholinergic symptoms
|
|
|
What drug has SE of priapism?
|
Trazodone
|
|
|
What drug lowers the seizure threshold & can be used for smoking cessation
|
Buproprion
|
|
|
What drug is an appetite stimulant that is likely to result in weight gain
|
Mirtazapine (Remeron)
|
|
|
What drug works well with SSRIs and ↑ REM sleep
|
Trazodone (Desyrel)
|
|
|
what drug can be used for bedwetting in children ?
|
imipramine (Tofranil)
|
|
|
What are the different treatments for acute dystonia, tardive dyskinesia, and neuroleptic malignant syndrome (NMS)?
|
(1) Acute dystonia → anticholingeric drug
(2) Tardive dyskinesia → discontinue drug & switch to one with fewer exptrapyrimidal effects (3) NMS → dantrolene |
|
|
HYQ: What is the DOC for mania with psychosis?
|

Atypicals
|
|
|
What are the symptoms of serotonin syndrome?
|
(1) Mental status changes: anxiety, agitation, delirium, restlessness, disorientation
(2) Autonomic excitation: diaphoresis, tachycardia, hyperthermia, hypertension, vomiting, diarrhea (3) Neuromuscular: tremor, muscle rigidity, myoclonus, hyperreflexia - Ocular clonus: slow, continuous, horizontal eye mvmts - Spontaneous or inducible clonus - Babinski signs bilaterally |
|
|
Which neuroleptics are known for their extrapyramidal side effects?
|
High potency typical neuroleptics
|
|
|
What are the tx options for generalized anxiety disorder?
|
SSRIs, Buspirone, Venlafaxine, β-blockers
|
|
|
How does adjustment disorder with depressed mood differ from major depressive disorder (MDD)?
|
Adjustment disorder: arises w/in 3 months of a stressor & resolves w/in 6 mos of when the stressor is removed
Stressor has to be something other than bereavement Does NOT meet criteria for MDD |

