![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
What are the 4 basic classes of antiarrythmic drugs?
|
"No Bad Boy Keeps Clean"
Class I: Na+ channel blockers Class II: β-blockers Class III: K+ channel blockers Class IV: Ca2+ channel blocks |
|
|
List examples of Class 1A antiarrythmic agents
|
Class 1A (Na+ channel)
!A= Alters mycocardial cell membrane “Double Quarter Pounder ” Disopyramid, Quinidine, Procainamide |
|
|
List examples of Class 1B antiarrythmic agents
|
IB = Best post-MI, Blocks rapid influx of Na+ ions
“Lettuce, Tomato, Mayo, Pickles” Lidocaine, Tocainide, Mexiletine, Phenytoin |
|
|
List examples of Class 1C antiarrythmic agents
|
Class 1C = Contraindicated post-MI; slows Conduction
“Fries, Please” Flecainide, Propafenone |
|
|
List examples of Class 2 antiarrythmic agents
|
Class 2 [β-blockers]
Propanol, Metoprolol, esmolol |
|
|
List examples of Class 3 antiarrythmic agents
|
Class 3 [K+ channel]
Amiodarone, sotalol |
|
|
List examples of Class 4 antiarrythmic agents
|
Class 4 [CCB]
Diltiazem, verapamil |
|
|
List examples of cardiac glycoside agents
|
Digoxin/digitalis
|
|
|
What are other antiarrythmic agents, that don't below to a particular class?
|
Adenosine
Mg2+ |
|
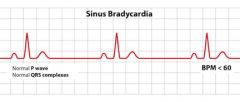
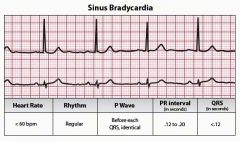
What medications can cause bradycardia?
|
Β-blockers, Ca2+ channel blockers, Digoxin, Amiodarone
|
|
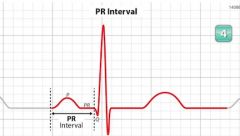
What are the EKG characteristics of 1st degree AV block?
|
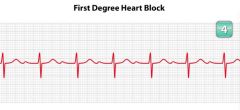
Prolonged PR interval (>200 msec)
|
|
|
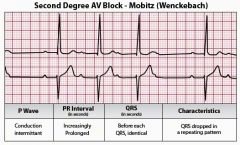
What are the EKG characteristics of Mobitz type I (2nd degree AV block)
|

PR intervals get progressively longer, until P wave is not conducted
|
|
|
What are the EKG characteristics of Mobitz type 2 (2nd degree AV block)
|

No progressive lengthening of PR interval
|
|
|
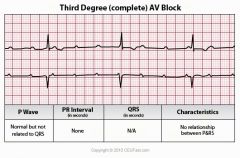
What are the EKG characteristics of 3rd degree AV block?
|
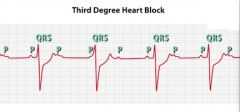
No p waves are conducted; no correlation btw P and QRS complexes
|
|
|
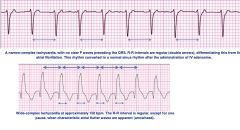
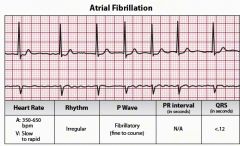
What are the EKG characteristics of atrial fibrillation?
|

No p waves
Flat or chaotic baseline Irregularly irregular narrow QRS complexes |
|
|
What tests should always be performed when looking for underlying causes of new-onset atrial fib?
|
Echocardiogram – looking for structural heart problems
TSH – hyperthyroidism can cause A-fib |
|
|
What classes of drugs are typically used for rate control in atrial fibrillation?
|
β- blocker (metoprolol)
Ca2+ channel blocker (diltiazem or verapamil) |
|
|
What are the two main concerns in the chronic treatment of atrial fibrillation?
|
Rate control vs rhythm control – isn’t clear if pts do better in sinus rhythm vs a-fib
Stroke risk – when atria aren’t contracting normally, blood tends to pool – can development a thrombus that can embolize and cause a stroke |
|
|
What is the risk of stroke associated with atrial fibrillation?
|
3-5% a yr
|
|
|
What drug is used to reduce the risk of stroke in patients with atrial fibrillation?
|
Lifelong anticoagulation with Warfarin (Coumadin)
|
|
|
What are the EKG characteristics of atrial flutter?
|
Regular, rapid atrial contractions (“saw tooth” baseline)
Atrial rate around 300bpm Ventricular rate of 300, 150, or 100 bpm |
|
|
What drugs are most commonly used to control the heart rate in acute atrial fibrillation with rapid ventricular response?
|
IV diltiazem
- 0.25mg/kg IV load (usually 15-20mg) - infusion of 5-10mg/hr - titrate to keep HR <100 Metoprolol - 5mg IV q 5 min x 3doses - 50-100mg PO BID |
|
|
A 66-year-old man with a history of hypertension and diabetes presents to your office with a complaint of palpitations for 1 week. EKG reveals atrial fibrillation with a resting HR of 72. After discussing treatment options, he decides that he would prefer a trial of electrical cardioversion in order to avoid lifelong anticoagulation. What preliminary steps would need to be undertaken before cardioversion?
|
Anticoagulate with Warfarin for 3-4wks
Transesophageal echo (TEE) to look for atrial thrombus Cardioversion Continue warfarin for 4 more weeks |
|
|
Amiodarone is sometimes used to help maintain sinus rhythm in patients with atrial fibrillation. What studies are commonly followed in patients taking amiodarone, to monitor for toxicity?
|
Check the “Ts”
LFTs (liver function tests) TfTs (thyroid function tests) PFTs (pulmonary function tests) |
|
|
What are the two most common causes of paroxysmal supraventricular tachycardia (SVT)?
|
SVT occurs when the sinoatrial node rhythm is superseded by a faster rhythm, usually originating in the AV node.
(1) AV nodal re-entry tachycardia (AVNRT) (2) Wolff-Parkinson White Syndrome |
|
|
What drug can be used to break or slow SVT?
|
IV Adenosine
|
|
|
What does a premature ventricular contraction (PVC) look like?
|
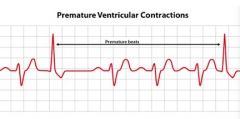
Large, wide QRS not associated with a P wave
|
|
|
What do we call >3 PVCs in a row?
|
Ventricular tachycardia (VTach)
|
|
|
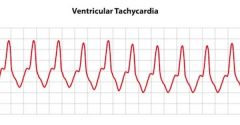
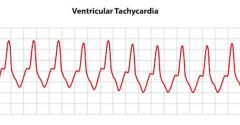
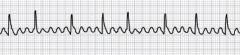
What are the EKG characteristics of ventricular tachycardia (VTach)?
|
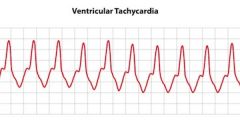
Wide-complex tachycardia, arising from the ventricle
Rate is usually 150-250 bpm |
|
|
If untreated, into what rhythm will VTach often degenerate?
|
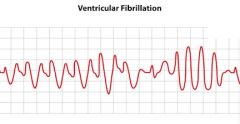
Ventricular fibrillation – can lead to death
|
|
How is VTach managed?
|
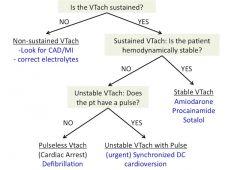
see above
|
|
|
What is the tx of Torsades de Pointes?
|
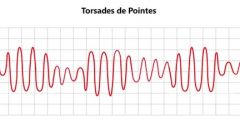
What it is: Type of VTach with special pattern on EKG
Specially assoc with prolonged QT intervals & can assoc with hypomagnesemia Tx: Defibrillation IV Magnesium Possibly amiodarone |
|
|
Wolff-Parkinson-White (WPW) syndrome is caused by an abnormal connection between atria and ventricles through an accessory bypass tract. What is the most common accessory bypass tract causing WPW syndrome?
|
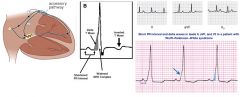
Bundle of Kent
|
|
|
What rhythm is classically described as being “irregularly irregular”?
|

Atrial fibrillation
|
|
|
What rhythm is classically described as having a “saw tooth” pattern on the baseline?
|
atrial flutter
|
|
|
A 68-year-old man with a history of coronary artery disease (CAD) presents to the ER with a complaint of chest pain and is subsequently admitted to telemetry unit for monitoring. Overnight, the nurse calls you to the bedside because of tachycardia. His heart rate has been 160 beats per minute for the last 3 minutes. You race to the bedside, only to find the patient sitting up comfortably. He denies any pain or dyspnea, and says he feels fine. His BP is 114/72, but the telemetry monitor shows a wide-complex rhythm with a rate of 156, and you diagnose ventricular tachycardia. What are your next steps?
|
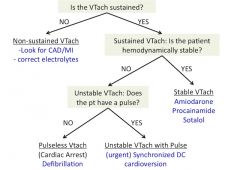
First ask, “is the pt hemodynamically stable?” yes
amiodarone, procainamide, or sotalol check 12-lead EKG and electrolytes |
|
|
While you are waiting for your orders from the previous question to be carried out, the patient begins to complain of feeling “woozy”. You check his blood pressure, and discover that it has fallen to 82/60. The tele monitor still shows ventricular tachycardia with a rate in the 150s-160s. What are your next steps?
|
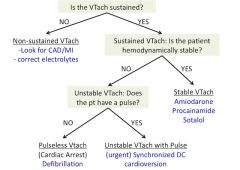
Now unstable, check for a pulse!
|
|
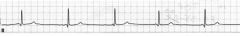
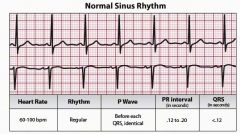
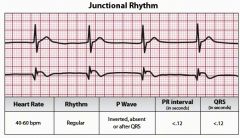
Narrow QRS associated with P waves, rate 60
|
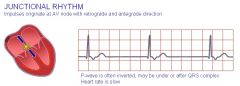
Junctional rhythm
|
|
|
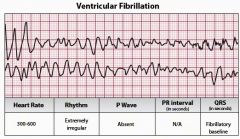
Chaotic, erratic, wide QRS
|
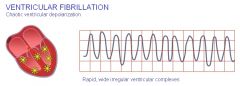
Ventricular fibrillation
|
|
|
Wide QRS, not associated with P waves, rate 20-40
|
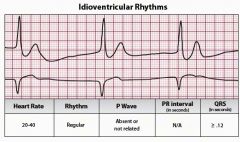
Ventricular Rhythm = Ventricular impulses come from the ventricles.
Inherent rate of ventricles is: 15 -40 beats per minute Idioventricular Rhythm (IVR) or Ventricular Escape Rhythm May be due to: MI, metabolic imbalances, or severe hypoxia. Treatment includes activation of code, CPR given if patient is pulseless. Lidocaine is contraindicated since it may knock out the last available pacemaker. |
|
|
Wide QRS, not associated with P waves, rate >100
|
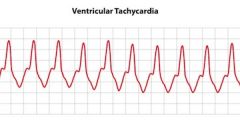
V-Tach
|
|
|
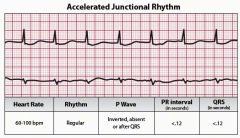
Narrow QRS not associated with P waves, rate >60 but <100
|
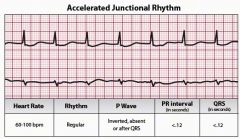
Accelerated junctional rhythm
|
|
|
Wide QRS tachycardia with variable amplitude in a repeating pattern
|
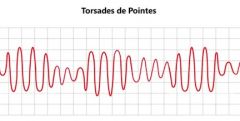
Torsades de Pointes
|
|
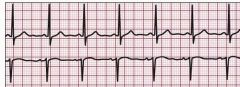
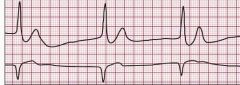
Interpret
|
see above
|
|
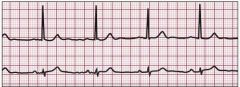
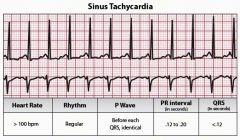
interpret
|
see above
|
|
interpret
|
see above
|
|
interpret
|
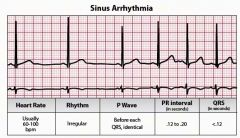
see above
|
|
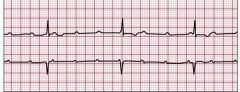
interpret
|
see above
|
|
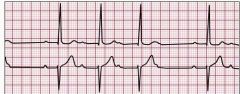
interpret
|
see above
|
|
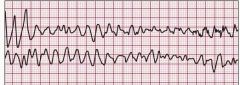
interpret
|
see above
|
|
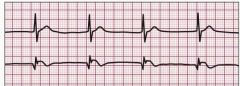
interpret
|
see above
|
|
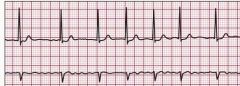
interpret
|
see above
|
|
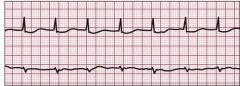
interpret
|
see above
|
|
interpret
|
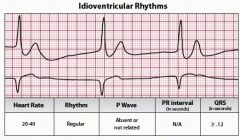
Ventricular Rhythms = Ventricular impulses come from the ventricles.
Inherent rate of ventricles is: 15 -40 bpm Idioventricular Rhythm (IVR) or Ventricular Escape Rhythm |
|

General structure of an EKG tracing:
What does the P wave represent? PR interval? QRS complex? ST segment? T wave? U wave? |
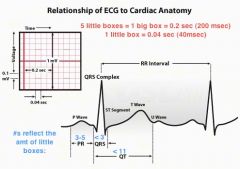
P wave = atrial depolarization
PR interval = conduction thru AV node (less than 0.2 sec, or 3-5 small squares) - measure from start of P to start of QRS complex QRS complex = ventricular depolarization (< 0.12 sec, or 3 little boxes) ST segment = isoelectric ventricular contraction T wave = ventricular repolarization U wave = hypokalemia |
|
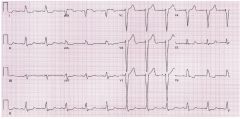
Diagnosis?
|
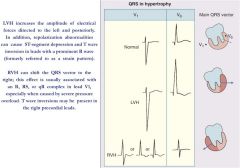
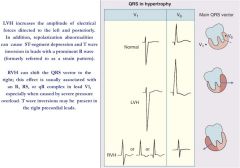
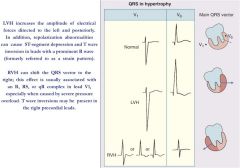
Left Ventricular Hypertrophy:
Marked LVH pattern with prominent precordial lead QRS voltages. ST depression and T wave inversion can be seen with severe LVH in leads with a predominant R wave. Left atrial abnormality is also present. |
|
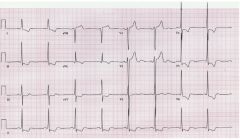
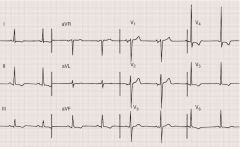
Diagnosis?
|
Left ventricular hypertrophy. Note the striking S wave amplitude in the right precordial leads and R wave amplitude in the left precordial leads. Repolarization abnormalities are present in the left precordial leads, as well as the limb leads. The S wave amplitude in V3 (2.4 mV) plus the R wave amplitude in aVL (1.0 mV) total 3.4 mV, easily satisfying the Cornell voltage criteria in this 76-year-old hypertensive man. Sinus bradycardia (50 beats per minute) is present as well.
|
|
diagnosis?
|
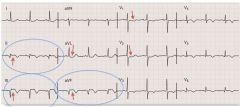
Evolving inferoposterolateral infarction.
Note the prominent Q waves in II, III, and aVF, along with ST-segment elevation and T wave inversion in these leads, as well as V3 through V6. ST depression in I, aVL, V1, and V2 is consistent with a reciprocal change. Relatively tall R waves are also present in V1 and V2. |
|
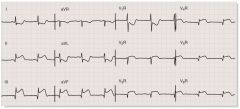
Diagnosis?
|
Acute right ventricular infarction with acute inferior wall infarction. Note the ST-segment elevation in the right precordial leads, as well as in leads II, III, and aVF, with reciprocal changes in leads I and aVL. ST-segment elevation in lead III greater than in lead II and right precordial ST-segment elevation are consistent with proximal to middle occlusion of the right coronary artery. The combination of ST-segment elevation in conventional lead V1 (V2R here) and ST-segment depression in lead V2 (lead V1R here) has also been reported with acute right ventricular ischemia or infarction.
|
|
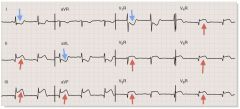
Diagnosis?
|

Complete LBBB with acute inferior myocardial infarction. Note the prominent ST-segment elevation in leads II, III, and aVF, with reciprocal ST-segment depression in leads I and aVL superimposed on secondary ST-T changes. The underlying rhythm is atrial fibrillation.
|
|
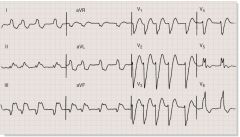
Diagnosis?
|

Left bundle branch block (LBBB). The QRS is widened, with a broad, notched complex in leads I, aVL, and the left precordial leads. Small r waves and broad, deep S waves are present in the right precordial leads. With LBBB, the axis is usually normal or deviated to the left. ST segments and T waves are discordant with the QRS complex throughout the precordium.
|
|
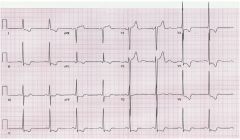
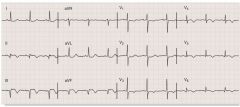
Diagnosis?
|
Left ventricular hypertrophy. Note the striking S wave amplitude in the right precordial leads and R wave amplitude in the left precordial leads. Repolarization abnormalities are present in the left precordial leads, as well as the limb leads. The S wave amplitude in V3 (2.4 mV) plus the R wave amplitude in aVL (1.0 mV) total 3.4 mV, easily satisfying the Cornell voltage crite- ria in this 76-year-old hypertensive man. Sinus bradycardia (50 beats per minute) is present as well.
|

