![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
Set 1
|
Set 1
|
|
|
5α-‐reductase deficiency leads
to what physical findings (internal and external) in a male? |
External Genitalia: "Penis @ 12'
Ambiguous external Genitalia until puberty. @ puberty, testosterone Increases --> masculinization and growth of external genialia. Internal Genitalia: Normal |
|
|
You start a pt on a Rx that has been on the market for 5 yrs. It has excellent efficacy. However, your pt begins to have an annoying side effect one month after initiation of this Rx. She contacts the manufacturer about it; and they, in turn, contact you to gather data on her course while on the Rx. In what phase of the clinical trial would this example fall?
|
Phase IV:
Study Sample: Post-marketing surveillance trial of pts after approval Purpose: Detects rare or Long term AEs |
|
|
A 12 y/o male is taken to the ER for confusion aassociated w/ vomiting and ABD pain. On exam you not a fruity breath odor and that the pt is experiencing rapid deep breathing. The pts random blood glucose is 522 mg/dL.
1) What cond'n is the pt experiencing? 2) What are the rapid, deep breaths called? 3) what ketone body is the cause of the pt's fruity breath odor? 4) Which Ketone body is detected by a urine test in diabetic ketoacidosis? Which will not? ***Own Ques: BL of Ketoacidosis?*** |
1) Diabetic Ketoacidosis
2) Kussmaul Respirations 3) Acetone 4) Acetone and Acetoacetate, NOT beta-hydroxybutyrate! ***Diabetes --> No Insulin or Insulin Resistance --> No uptake of Glucose into cells --> Body breaks down fat (TGs) for energy --> Fatty Acids converted to Acetyl-CoA --> Acetyl CoA goes to TCA OR converted to Ketones (beta-hydroxybutyrate > acetoacetate) |
|
|
Aztreonam and penicillins both bind to penicillin-binding PROs.
1) Can aztreonam be used in pts w/ a penicillin allergy? 2) In which pt populations is aztreonam a good choice? 3) Against which organisms is Aztreonam effective? ***1) What is the purpose of PBPs (Penicillin Binding PROs)? 2) TF, what is the MOA aztreonam? 3) So, can you name 7 Antimicrobials (including aztreonam) whose MOA is to inhib peptidoglycan cross-linking and TF cell wall synthesis? 4) Can you name 2 antimicrobials whose MOA is to inhibit peptidoglycan synthesis and TF cell wall synthesis? |
ANSWER
1) Yes, no cross-sensitivity w/ penicillins or cephalosporins 2) PCN-Allergic pts Pts w/ renal insufficiency who can't tolerate amino-glycosides 3) ONLY GRAM NEG RODS!!! ***1) PBPs are req'd for cross-linking of peptidoglycan in bacteria 2) Inhibs Cell wall Synthesis by inhib peptidoglycan cross-linking 3) Penicillin, Methicillin, Ampicillin, Piperacillin, Cephalosporins, Aztreonam, Imipenem 4) Bacitracin. Vancomycin |
|
|
32 y/o man brought to hospital for minor vehicle crash. Overnight you are called by the nurse bc the pt's blood pressure went from 125/80 to 201/111, and he is now tachycardic. Pt is diaphoretic, and reports feeling anxious.
Though, he says that this happens once or twice per week. Suspecting the diagnosis, you check his abdominal CT scan, which does, in fact, show an adrenal mass. What 2 alpha-adrenergic antagonist should be used to tx this pt? ***Own Ques: 1. What is the Dx? 2. MOA of Phenoxybenzamine? 3. Should you administer Phenoxybenzamine before or after removing the tumor? 4. 2 AEs of Phenoxybenzamine? 5. MOA of Phentolamine? A) Another CU of phentolamine? 6. Can you name 3 alpha-1 selective antags? (aka: the -zosins) 7. Can you name 1 alpha-2 selective antags? 8) Now, Phenoxybenzamine and Phentolamine will dec the pt's HTN, but what Rx class do you want to use to tx the tachycardia? A) Why? |
Phenoxybenzamine
Phentolamine ***Own Ques 1. Pheochromocytoma secreting catecholamines 2. IRREVERSIBLE, Non-selective (binds all!) alpha-receptor antag 3. Before 4. Orthostatic Hypotension; Reflex Tachycardia 5. Reversible, non-selective alpha receptor antag A) Pts on MAO inhibs who eat tyramin-containing foods 6. Prazosin, Terazosin, Doxazosin 7. Mirtazapine 8. beta blockers A) BC the heart does NOT has beta-receptors, not alpha receptors. TF Phenoxybenzamine and Phentolamine will have no effect. |
|
|
1) How do primary and secondary hyperaldosteronism differ in their effect on plasma renin levels?
2) How to treat primary hyperaldosteronism? (2) ***Own Ques 1. Give Pathogenesis for Primary Hyperaldosteronism? 2. Give Pathogenesis for Secondary Hyperaldosteronism? |
1) Primary Hyperaldosteronism --> Dec Plasma Renin
Secondary Hyperaldosteronism --> Inc Plasma Renin 2) Surgical Removal of Tumor K+ Sparing Diuretic / Aldosterone Recept Antag: Spirinolactone ***Own Ques: 1. Adrenal Hyperplasia or Aldosterone secreting tumor --> Inc Aldosterone --> A. Negative Feedback on Rening @ Kidney --> IN RENIN B. HTN & HYPOKALEMIC METABOLIC ALKALOSIS 2. CHF, Chronic Renal Failure, Cirrhosis, Nephrotic Syndrome, Renal Art Stenosis --> Kidney sees a dec volume of blood --> Stim RAA System to Inc Blood Vol --> INC RENIN |
|
|
35 y/o G1P0 has been hospitalized for observation of vaginal bleeding from a placental abruption. Her most recent labs represent an increase in BT (bleeding time), PT (prothrombin time), PTT (Partial Thromboplastin Time). You are concerned that this patient might be at risk for DIC (Disseminated Intravascular Coagulation.
1. What is this pt's risk factor for having DIC? 2. What additional RFs are assoc w/ DIC? 3. What additional lab findings are assoc w/ DIC? (8) ***Own Ques: 1. Define DIC? 2. PC (PLT Count) Checks what? 3. PT / INR Checks What? 4. PTT Checkw What? 5. BT Checks what? |
1. Obstetric Complications (Placental Abruption)
2. STOP Making New Thrombi: Sepsis (gram neg); Trauma; Obstetric complications; Pancreatitis; Malignancy; Nephrotic syndrome; Transfusion 3. Schistocytes; Thrombocytopenia; Inc Fibrin Split Products (D-Dimers); Dec Fibrinogen; Dec Factor V & VIII; Inc BT; Inc PT; Inc PTT *Own Ques: 1. Widespread activation of clotting --> A deficiency in clotting factors --> Bleeding 2. NUMBER of PLTs only! 3. VII; X, V, II, I and TF Integrity of Extrinsic Pathway --> Clot 4. XII, XI, IX, VIII; X, V, II, I and TF Integrity of Intrinsic Path --> Clot 5. Integrity of PLTs only |
|
|
A 43 y/o male complains of Right Sided facial drooping. When you examine the pt you notice an upper and lower face drooping.
1. Does this pt have a lower or upper motor neuron lesion? 2. What dz'es are assoc w/ Bell's Palsy? |
1. LMN Lesion
2. "ALexander graHam Bell w/ STD"- Aids, Lyme dz, Herpes simplex, Sarcoidosis, Tumors, Diabetes |
|
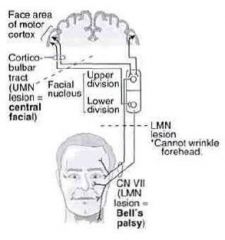
***OWN QUES TO GO W/ TOPIC ON LAST FLASHCARD
1. Give the 2 pathways for innervation of face muscles? 2. So, which division of the facial nucleus receives innervation from both sides of the brain? A) Therefore, which part of face receives innervation from both sides of brain? 3. So a lesion of the motor cortex of connection between the motor cortex and the facial nucleus will --> what s/s? A) Why? 4. A Lesion in the LMN will produce what s/s? A) Why? 5. Bell's Palsy results from what? A) This leads to what s/s? B) Do you remember from the last card, what Dz'es can lead to Bell's Palsy? |
1.
Face area of Motor Cortex --> Cortico-Bulbar Tract and Cross at Pyramids --> Upper AND Lower divisions of CL Facial Nucleus --> CL Upper and Lower face muscles via facial nerve Face area of Motor Cortex --> __?___ Tract --> Upper Division of Ips Facial Nucleus --> Upper Face Muscles via facial nerve 2. Upper division A) Upper part of face 3. CL paralysis of Lower face only A) BC CL upper face receives additional innervation from the ipsilateral motor cortex 4. Ips paralysis of upper AND lower face A) BC it knocks out the facial nerve AFTER all the UMNs have converged on the facial nucleus 5. Complete destruction of facial nucleus A) Complete facial paralysis of entire side Ips to destroyed facial nucleus (can't close eye!) B) See Previous Card |
|
|
What are the important fnctns of Vitamin C?
|
-Antioxidant
-Reduces Fe3+--> Fe2+ --> Fe to be in an absorbable state -Req'd for Dopamine beta-hydroxylase which converts dopamine to NE -Req'd for Hydroxylation of proline and lysine during collagen synthesis |
|
|
***Own Ques based on previous card
1. Vit C Defic --> What 2 Dz'es / Cond'ns? 2. 5 s/s of scurvy? 3. 5 s/s of Vit C Excess? A) Can lead to Fe toxicity in what 2 groups of people? |
1. Scurvy and weakened immune system
2. Swollen gums, bruising, hemarthrosis, anemia, poor wound healing 3. N/V/D, Fatigue, Sleep probs A) Pts w/ transfusions and hereditary hemochromatosis |
|
|
A Physician while working with a humanitarian aid organization in Africa, is seeing a 30 y/o male pt w/ HIV. The pt c/o fever, wt loss and a cough assoc w/ hemoptysis over the past 2 months. CXR reveals a perihilar lymphadenopathy and a left lower lobe granulomatous formation.
1. What is the name for these x-ray findings? A) A Ghon Complex is composed of what? 2. What other 2 Myocbacteria species causes pulmonary dz? 3. What are the potential extrapulmonary manifestations of Mycobacterium tuberculosis? (5) |
1. Ghon Complex
A) TB Granulomas in Lung (Ghon focus + Lobar and Perihilar Lymph Node Involvement) 2. Mycobacterium kansasii Mycobacterium avium 3. CNS: Parenchymal Tuberculoma or Meningitis Vertebral Body: Pott's Dz Lymphadenitis Renal TB Infxn GI TB Infxn |
|
|
The neonatologist you're working with on your pediatrics rotation suspects a newborn to have DiGeorge syndrome.
1. What is the underlying cause of DiGeorge syndrome? 2. What are the 5 manifestations of DiGeorge Syndrome? ***Own Ques: What are 4 labs / imaging findings? |
1. 22q11 deletion -->
failure of 3rd and 4th pharyngeal pouches to develop --> Thymic Aplasia (Thymus doesn't form) 2. Hypocalcemia --> Tetany; Recurrent viral / fungal infxn (remember, T-cells mature in thymus); Congenital Heart and Great Vessel Defects; Cleft Pallate; Abnormal Facial Features ***Own Ques: Dec T-CElls, Dec PTH, Dec Ca, No Thymic Shadow on CXR (Understand why, bc they should all make sense!) |
|
|
1) Amyloidosis and sarcoidosis are associated w/ which cardiomyopathy?
A) What is restrictive / Obliterative Cardiomyopath 2) What are some other dz'es or cond'ns associated w/ this cardiomyopathy? |
1) Restrictive / Obliterative Cardiomyopathy
A) Stiff vents --> diastolic dysfnctn (probs filling) 2) Sarcoidosis, Amyloidosis, Postradiation Fibrosis, Endocardial Fibroelastosis (thick fibroelastic tissue in endocardium of kids), Loffler's Syndrome (Endomyocardial fibrosis w/ prominent eosinophilic infiltrate), Hemochromatosis |
|
|
A pt of yours with recent complaints of weakness, pallor, craving for ice chips and tachycardia has a hx of chronic hemorrhoids.
1. What do you immediately suspect is the cause of this pt's anemia 2. How do you tx it / work it up? ***Own Ques 1) Give the pathogenesis of Fe Defic anemia? 2) 2 Typical findings of Fe defic anemia? A) Assoc w/ what syndrome? What is the classic triad of this syndrome? |
1. Fe deficiency anemia
2. Fe Replacement; Possible Colonoscopy to eval for colon cancer ***Own Ques 1) Chronic Bleeding from GI or menorrhagia, malnutrition, Fe malabsorption --> Dec Fe OR Pregnancy --> Inc Fe Demand --> Dec Heme Synthesis 2) Microcytosis and hypochromia A) Plummer-Vinson Syndrome. Fe Defic Anemia, Esophageal Web, Atrophic Glossitis |
|
|
How is the body affected by a prolonged stay in space @ zero gravity? (5)
|
Dec Blood Volume
Dec RBC Mass Dec Muscle Strength --> Dec work capacity Dec Max Cariac Output Dec Bone Mass |
|
|
1) What are the 3 MC Viral Causes of Myocarditis?
2) What are 2 LC Viral Causes of Myocarditis |
1) Coxsackie A & B
Echovirus 2) Influenza HIV CMV |
|
|
SET 2
|
SET 2
|

