![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
1120 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is the relationship between the notochord, neural plate and neural crest cells?
|
-Notochord induces overlying ectoderm to form Neural Plate
-Neural plate then folds to form the neural tube and and neural crest cells |
|
|
|
What is the embryologic origin of:
olfactory epithelium |
Surface ectoderm
|
|
|
|
What is the embryologic origin of:
Cornea of the eye |
Neural crest
|
|
|
|
What is the embryologic origin of:
lens of the eye |
surface ectoderm
|
|
|
|
What is the embryologic origin of:
retina of the eye |
neuroectoderm
|
|
|
|
What is the embryologic origin of:
salivary, sweat, mammary glands |
surface ectoderm
|
|
|
|
What is the embryologic origin of:
tissue just above the pectinate line |
endoderm
|
|
|
|
What is the embryologic origin of:
tissue just below the pectinate line |
ectoderm
|
|
|
|
What is the embryologic origin of:
lower 2/3 vagina |
endoderm
|
|
|
|
What is the embryologic origin of:
upper 1/3 vagina |
mesoderm
|
|
|
|
What is the embryologic origin of:
Adrenal Medulla? Adrenal cortex? |
Medulla = neural crest
Cortex = mesoderm |
|
|
|
What is the embryologic origin of:
testes, ovaries |
endoderm
|
|
|
|
The following are defects of which embryologic origin:
Vertebral Defects Anal Atresia Cardiac Defects Tracheo-Esophageal Fistula Renal Defects Limb Defects (bone and muscle) |
Mesoderm
|
|
|
|
What is the embryologic origin of:
Adenohypohysis |
Surface Ectoderm
|
|
|
|
What is the embryologic origin of:
Neurohypophysis |
Neuroectoderm
|
|
|
|
What is the embryologic origin of:
Autonomic Nervous system |
Neural Crest
|
|
|
|
What is the embryologic origin of:
CNS |
Neuroectoderm
|
|
|
|
What is the embryologic origin of:
-Aorticopulmonary Septum? -Heart Structures? |
Aorticopulmonary Septum= Neural Crest
Heart Structures = Mesoderm |
|
|
|
What is the embryologic origin of:
Eustachian tube |
Endoderm
|
|
|
|
What is the embryologic origin of:
Bones of inner ear |
Neural Crest
|
|
|
|
What is the embryologic origin of:
Melanocytes |
Neural Crest
|
|
|
|
What is the embryologic origin of:
Cranial Nerves |
Neural Crest
|
|
|
|
What vitamin overdose during pregnancy can alter HOX-gene expression and cause synpolydactyly (fused 3rd-4th digit)
|
Vitamin A
(retinoic acid) |
|
|
|
What precursor cell type invaginates to form the primitive streak?
|
Epiblast
|
|
|
|
What is the embryologic origin of:
bones of the skull |
Neural Crest
|
|
|
|
What is the embryologic origin of:
Bladder, urethra |
Endoderm
|
|
|
|
What drives the cell cycle?
|
Cyclins activate CDK forming Cyclin-CDK complexes
Complexes phosphorylate target proteins to drive the cycle |
|
|
|
What tumor suppressor blocks the G2 --> M phase?
|
p53
|
|
|
|
Which tumor suppressors inhibit G1-->S ?
|
p53
Rb |
|
|
|
Cyclin
CDK Tumor Suppressors These regulate what? |
Cell Cycle progression
|
|
|
|
When Rb is phosporylated, it is released from ____.
|
EF-2
Whith EF-2 unbound, it carries out the synthesis needed to progress to the S-phase |
|
|
|
A mother gives birth to monozygotic twins.
The placenta is sent to the lab and shows that the twins were diaminonic and dichorionic. When did cleavage take place? |
Before day 3
(@ Day 3 the chorion develops) |
|
|
|
A mother gives birth to monozygotic twins.
The placenta is sent to the lab and shows that the twins were monochorionic and diamniotic. When did cleavage take place? |
After day 3, before day 8
(after day 3 means they have one placenta that they share, after day 8 means they both have their own amniotic sac) |
|
|
|
Failure of the decidua basalis to form can result in a placenta _____ where the placenta invades the myometrium
|
placenta accreta
|
|
|
|
A child presents with increased orotic acid in the urine, megaloblastic anemia and failure to thrive.
Vit. B12 and folate supplementation do not correct the anemia. What is going on? |
Orotic aciduria
---------------------------------------------- ↓Orotic Acid PRPP or ↓ ortodine 5'-phosphate decarboxylase |
|
|
|
What drug blocks ribonucleotide reductase and inhibits pyrimidine/purine synthesis?
|
Hydroxyurea
|
|
|
|
What drug blocks thymidylate synthase (↓dTMP) which inhibits pyrimidine/purine synthesis?
|
5-FU
|
|
|
|
Orotic Acid is needed for ____ synthesis
|
pyrimidine
|
|
|
|
This disease is marked by adenosine deaminase deficiency which creates excess ATP and dATP.
Imbalances in ATP and dATP inhibit ribonucleotide reductase which PREVENTS DNA synthesis and ↓ lymphocyte count. |
SCID
|
|
|
|
This syndrome is caused by defective purine salvage due to absence of HGPRT, which converts hypoxanthine to IMP and Gaunine into GMP.
Ultimately, the result is increased uric acid production and increased de-novo purine synthesis Sx: mental retardation, self-mutilation, agression, hyperuricemia and gout |
Lesch-Nyhan Syndrome
|
|
|
|
What form of DNA repair is mutates in xeroderma pigmentosum?
Mutation prevents repair of thymine-thymine dimers caused by UV-light exposure.. |
Nucleotide Excision repair
|
|
|
|
Which tpye of DNA repair is mutated in Hereditary Nonpolyposis Colon CA?
|
mis-match repair
|
|
|
|
What is the mRNA start codon?
|
AUG
(codes for methionine in euks) (codes for formyl-methionine in proks) |
|
|
|
What are the 3 mRNA stop codons?
|
UGA (you go away)
UAG (you are gone UAA (you are away) |
|
|
|
____ is a stretch of DNA that alters gene expression by binding to transcription factors
|
Enhancer region
|
|
|
|
_____ is the site on DNA where RNA polymerase and multiple other transcription factors bind to DNA upstream from gene loci (AT-rich, upstream sequence with TATA and CAAT boxes)
|
Promoter
|
|
|
|
Where do negative regulators (repressors) bind toon DNA?
|
Silencer region
|
|
|
|
rRNA synthesis occurs in the cell's ____
|
nucleolus
|
|
|
|
mRNA and tRNA synthesis occur in the cell's ______
|
cytoplasm
|
|
|
|
What 3 steps are required for RNA processing?
|
1) 5' capping (7-methylgaunosine)
2) 3' Poly-A tail (about 200 adenines) 3) Splicing out of introns ------------------------------------------ Capped, spliced and tailed transcript is called mRNA!!!! 3) |
|
|
|
Patients with SLE make antibodies to what proteins needed for splicing of pre-RNA?
|
anti-sNRPs antibodies
|
|
|
|
Patients with SLE have anti-sNRP antibodies that ultimately inhibits _____ of pre-RNA...
|
splicing of introns
|
|
|
|
What enzyme matches AA's to tRNA?
What antibiotic blocks this enzyme on the 30s ribosome? |
Aminoacyl-tRNA synthetase
(-) by Tetracyclines |
|
|
|
Protein Synthesis inhibitors:
- bind to 30S and (-) formation of initiation complex and cause mis-reading of mRNA |
Aminoglycosides
|
|
|
|
Protein Synthesis inhibitors:
-inhibits 50S peptidyltransferase |
Chloramphenicol
|
|
|
|
Protein Synthesis inhibitors:
-block translocation (moving from A to P site) |
Macrolides (erythromycin)
|
|
|
|
Protein Synthesis inhibitors:
-blocl peptide bond formation (2) |
Clindamycin and Chloramphenicol
|
|
|
|
This cell organelle catabolizes very long-chain fatty acids and amino acids via beta-oxidation
Helps to generate PLASMALOGEN for neural tissue which aid in getting rid of reactive O2 species |
Peroxisome
|
|
|
|
In this disease, ↓ mannose-6-phosphate means that lysosomal enzymes cannot be targeted to lysosomes for trafficking.
Enzymes leak outside of cell instead of sent to lysosomes. Sx: -coarse facial features - ↓ joint movement - ↑ levels of lysosomal enzymes in serum |
I-cell Disease
|
|
|
|
Name 5 drugs that act on microtubules:
|
1) Mebendazole (anti-helminthic)
2) Vincristine (anti-cancer 3) Paclitaxel (anti-breast cancer) 4) Griseofulvin (antifungal) 5) Colchicine (anti-gout) |
|
|
|
Which disease is characterized by a microtubule polymerization defect resulting in ↓ fusion of of phagosomes and phagolysosomes?
Sx: recurrent pyogenic infections partial albinism peripheral neuropathy |
Chediak Higashi Syndrome
|
|
|
|
What is the powerhouse behind cilia movement?
|
Dynein ATPase
(absent in Kartagener's) |
|
|
|
What is alcohol's effect on a cell?
|
degrades the plasma membrane
|
|
|
|
What intermediate filament stain could you use for:
-osteosarcoma |
Vimentin
(Connective tissue) |
|
|
|
What intermediate filament stain could you use for:
-Squamous cell carcinoma |
Cytokeratin
(Epithelial cells) |
|
|
|
What intermediate filament stain could you use for:
-Astrocytoma, GBM, Schwannoma |
GFAP
|
|
|
|
What intermediate filament stain could you use for:
-Leiomyoma (uterine fibroid) |
Desmin
(smooth m, skeletal m., cardiac m.) |
|
|
|
What intermediate filament stain could you use for:
-Neuroblastoma (Adrenal) |
Neurofilaments
(Axons within neurons) |
|
|
|
Na+/K+ ATPase
For every 3 Na+ that come into the cell, how many K+ molecules are pumped out? |
2
|
|
|
|
Name the type of collagen that produces:
-Skin, Tendon, Bone |
Type I
|
|
|
|
Name the type of collagen that produces:
-cartilage, vitreous body, nucleus pulposis |
Type II
|
|
|
|
Name the type of collagen that produces:
-Cornea |
Type I
|
|
|
|
Name the type of collagen that produces:
-skin, blood vessels, uterus, fetal tissue, granulation tissue |
Type III
|
|
|
|
Name the type of collagen that produces:
-Basement membrane or basal lamina |
Type IV
|
|
|
|
What type of collagen is missing/defective in:
-Osteogenesis imperfecta |
Type I
|
|
|
|
What type of collagen is missing/defective in:
-Ehrler's Danlos |
Type III
|
|
|
|
What type of collagen is missing/defective in:
-Alport Syndrome |
Type IV
|
|
|
|
What's the best Tx for a keloid scar?
|
glucocorticoids
|
|
|
|
Collagen is made inside ____blasts
|
fibroblasts
|
|
|
|
During collagen synthesis, hydroxylation of proline and lysine residues in the RER of the fibroblasts requires ______
|
Vit. C
|
|
|
|
During collagen synthesis, tropocollagen molecules are reinforced by COVALENT lysine-hydroxylysine cross linkage to make collagen fibrils.
Does this take place inside or outside of the fibroblast? |
outside of fibroblast
|
|
|
|
Type ___ osteogenesis imperfecta is fatal in the utero or neonatal perioid
|
Type II osteogenesis imperfecta
|
|
|
|
elastase is normally inhibited by _____
|
alpha-1-antitrypsin
|
|
|
|
What is the inheritance of Alport syndrome?
|
XR
|
|
|
|
This blotting test identifies DNA-binding proteins (transcription factors) using labeled oligonucleotide probes
|
Southwestern Blot
(longest name, longest probe) |
|
|
|
What antibiotic can be used to treat SIADH?
|
demeclocycline
|
|
|
|
What is it causes when 1 gene has more than 1 effect on a person's phenotype?
|
Pleiotrophy
|
|
|
|
What is genetic imprinting? Give an example..
|
At some loci, only one gene is active while the other is Inactive.
With 1 allele inactivated, deletion of the active allele results in disease. In Prader Willi syndrome, the maternal allele is inactivated, while the PATERNAL allele is deleted. (Chromosome 15) |
|
|
|
What heart-valve deformity is associated with ADPKD?
|
mitral valve prolapse
|
|
|
|
In patients with Familial adenomatous polyposis, the mutation of the APC gene occurs on chromosome ____
|
chromosome 5
|
|
|
|
This autosomal dominant disease affects the blood vessels and features:
-telangiectasia -recurrent epistaxis -skin discoloration -arteriorvenous malformations (AVM) |
Hereditary hemorrhagic telangiectasia
(Osler-Weber-Rendu Syndrome) |
|
|
|
What type of aortic necrosis occurs in patients with Marfan Syndrome?
|
cystic medial necrosis of the aorta
|
|
|
|
This AD disease features:
-cafe-au-lait spots -neuronal tumors -Lisch nodules (pigmented iris hamartomas) -skeletal deformities -optic gliomas -mutation on chromosome 17 |
Neurofibromatosis type I
(von Recklinghausen) |
|
|
|
This AD disease features:
-Bilateral acoustic schwannomas -juvenile cataracts -mutation on chromosome 22 |
Neurofibromatosis type II
|
|
|
|
A sweat chloride test greater than 60 mg/L is diagnostic of ____
|
cystic fibrosis
(CTFR gene chromosome 7) |
|
|
|
In this autosomal recessive disease, a mutation causes ABNORMAL PROTEIN FOLDING resulting in the degredation of the Cl- channel
|
Cystic fibrosis
|
|
|
|
patients with cystic fibrosis can have deficiencies in what vitamins?
|
Fat Soluble
(ADEK) |
|
|
|
What drug can you give to loosen mucus plugs in patients with CF?
|
N-acetylcisteine
|
|
|
|
What is the inheritance pattern for:
-Wiskott-Aldrich -Fabry Disease -Hunter Disease -G6PD deficiency -Ocular albinsim -Lesch-Nyhan Syndrome -Duchenne + Becker MD -Hemophilia A + B |
x-linked recessive
|
|
|
|
What is the inheritance pattern for:
-Albinism -Infant Polycystic Kidney Dz -cystic fibrosis -glycogen storage diseases -mucoploysaccharidoses -PKU -Sickle Cell Anemia -Sphingolipidoses -Thalassemias |
Autosomal recessive
|
|
|
|
-CGG repeat
-macro-orchidism -long face w/ large jaw - large everted ears -autism -Mitral valve prolapse |
Fragile X
(X-linked) |
|
|
|
What is the trinucleotide repeat for:
-Fragile X Syndrome: -Friedrich's Ataxia: -Huntington's: -Myotonic dystrophy: |
-Fragile X Syndrome: CGC
-Friedrich's Ataxia: GAA -Huntington's: CAG -Myotonic dystrophy: CTG |
|
|
|
Fetal Quad Screen Shows:
↓ α-fetoprotein ↑ β-hCG ↓ estriol ↑ inhibin A |
Downs Syndrome
|
|
|
|
Fetal Quad Screen Shows:
↓ α-fetoprotein ↓ β-hCG ↓ estriol normal inhibin A |
Trisomy 18 (Edwards)
|
|
|
|
Quad Screen Shows:
normal α-fetoprotein normal β-hCG normal estriol normal inhibin A *Baby is born with severe MR, cleft palate/lip holoproscenephaly, polydactyly |
Trimsomy 13 (Patau)
|
|
|
|
95% of cases of Down Syndrome are associated with _____ in women over the age of 35
|
↑ meiotic non-dishunction
|
|
|
|
-Child is born with:
rocker bottom feet severe MR micrognathia low-set ears clenched hands** |
Trisomy 18 (Edwards)
|
|
|
|
Robertsonian translocation commonly occurs on which (5) chromosomes?
|
13, 14, 15
21, 22 ------------------------------------------ Long arms of two chromosomes fuse and the short arms are lost |
|
|
|
This vitamin is essential for normal differentiation of epithelial cells into specialized tissue
|
Vit. A
|
|
|
|
This vitamin is used to treat measles and AML type M3
|
Vit A
|
|
|
|
Deficiency of this vitamin causes night-blindness and dry skin
|
Vit. A
|
|
|
|
Defieciencies of this vitamin can cause beriberi
|
Vit. B1 (thiamine)
---------------------------------------------- **Dry Beriberi** -polyneuritis, symetrical muscle wasting **Wet Beriberi** -high-output cardio failure (dilated cardiomyopathy), edema |
|
|
|
This vitamin is derived from tryptophan and requires B6
|
B3 (niacin)
|
|
|
|
This vitamin is a cofactor in oxidation and reduction (FADH2)
-Deficiency causes Cheilosis and Corneal vascularization |
Vitamin B2 (riboflavin)
|
|
|
|
This Vitamin is used as a constituent of NAD+, NADP+ (used in redox rxns)
Deficiency may result in Pellagra. |
Vitamin B3 (niacin)
(excess=flushing) |
|
|
|
This B vitamin is an essential component of CoA and fatty acid synthesis
Deficiencies result in Dermatitis, enteritis, alopecia and adrenal insufficiency |
B5 (pantothenate)
|
|
|
|
This vitamin is needed for synthesis of cystathionine, heme, niacin and GABA
|
Vit. B6
|
|
|
|
Deficiency of this vitamin is inducible from drugs such as INH and OCPs
|
Vit. B6
|
|
|
|
This vitamin is an antioxidant for erythrocytes.
Deficiency of this vitamin leads to ↑ RBC fragility (hemolytic anemia) |
Vit. E
|
|
|
|
This Vitamin is an antioxidant that also:
1) Facilitates iron absorption by keeping iron in reduced Fe++ state 2) Necessary for hydroxylation of proline and lysine in collagen synthesis 3) necessary for dopamine β-hydroxylase which converts dopamine to NE |
Vit. C
|
|
|
|
This product in raw egg whites binds up biotin and can cause a biotin deficiency
|
Avidin
|
|
|
|
Vit. K catalyzes the ___-carboxylation of glutamic acid residues on various proteins concerned with blood clotting
|
γ-carboxylation of glutamic acid
|
|
|
|
Aerobic Metabolsim produces ___ ATP via the malate-aspartate shuttle (Heart and Liver)
___ ATP are produced via the glycerol-3-phosphate shuttle (muscle) |
32
30 |
|
|
|
What AA is the precursor to:
-Dopamine, NE, Epi |
Phenylalanine
|
|
|
|
What AA is the precursor to:
-GABA, Glutathione |
Glutamate
|
|
|
|
What AA is the precursor to:
-Heme |
Glycine
|
|
|
|
What AA is the precursor to:
Serotonin, melatonin, Vit. B3 (niacin) |
Tryptophan
|
|
|
|
What metabolic scenario favors Ketone production?
|
When Acetyl CoA exceeds oxidative capacity of TCA cycle
|
|
|
|
What controls our blood glucose during times of fasting between meals?
|
Hepatic Glycogenolysis is major contributor
Gluconeogenisis and FFA are minor contributors |
|
|
|
This vitamin is also called α-tocopherol
|
Vit. E
|
|
|
|
What amniotic fluid abnormality might you find in a fetus with anencephaly?
|
↑ α-fetoprotein
↑ AChE |
|
|
|
Which amino acids are modified in the golgi apparatus?
|
Serine
Asparagine Threonine "SAT" |
|
|
|
What sense is preserved in the upper extremities in a patient with syringomyelia?
|
sense of touch is preserved
**Bilateral loss of pain and temperature** |
|
|
|
What are the phagocytes of the CNS?
What is their embryonic origin? |
Microglia
**Derived from MESODERM** |
|
|
|
What are Lewy Bodies found in Parkinson's composed of?
|
α-synnuclein
|
|
|
|
A patient sustains a lesion to the right cortical motor face region..
What will the face look like? |
Left Lower Face will Droop
----------------------------------------------- NOTES: The facial motor nucleus receives motor fibers for the lower face from the opposite motor cortex. Motor fibers for the upper face are sent by both the left and right motor cortex |
|
|
|
A patient receives a lesion to the right facial nerve (CN VII).
What will the face look like? |
Both Upper + Lower Face will droop
|
|
|
|
A CN XII lesion will cause the tongue to deviated to the ____ of the lesion
|
same side
|
|
|
|
In a patient with a CN X lesion, the uvula deviates ___ the side of the lesion
|
away
(Weak palate collapses and uvula moves away) |
|
|
|
A patient with a CN XI lesion will have weakness turning the head to the ___ side and ____ side shoulder droop.
|
turning head to contralateral side
same side should droop |
|
|
|
What structures travel through the cavernous sinus?
|
Internal carotid a.
CN III CN IV CN V1 CN V2 CN VI (6) |
|
|
|
What should you immediately think of if a patient presents with Bilateral Bell's Palsy?
|
Guillan Barre
|
|
|
|
This disease is associated with both LMN + UMN signs. It can be caused to a defect in superoxide dismutase 1
There are NO sensory, occulomotor or cognitive defects |
ALS
|
|
|
|
Tabes dorsalis is caused by tertiary syphillis and causes degeneration of the ____ columns and roots
|
dorsal columns + dorsal roots
|
|
|
|
What CNs exit the internal auditory meatus?
|
CN VII
CN VIII |
|
|
|
What artery supplies the retinal artery?
|
choroid artery
|
|
|
|
Which nerve carries the post-ganglionic sympathetic signal to dilate the eye?
|
long ciliary n.
|
|
|
|
β-amyloid plaques
Neurofibrillary tangles |
Alzheimers
|
|
|
|
APOE4 = late onset of disease
APOE2= protective |
Alzheimers
|
|
|
|
See intracellular inclusions of tau protein in frontal lobe
|
Pick's Dz
(frontotemporal dementia) **Pick bodies** |
|
|
|
Dementia + hallucinations + α-synuclein defect
|
Lewy Body Dementia
|
|
|
|
APP gene in chromosome 21 makes patients with Down Syndrome more susceptible to what?
|
Alzheimer's
|
|
|
|
Rapid onset dementia
Spongiform cortex |
Creutzfield-Jacob
(prion disease) |
|
|
|
Dementia and ↓ACh
|
Alzheimers
|
|
|
|
Ascending muscle weakness following a Campylobacter jejuni or Herpes Virus infection
↑ CSF protein with a normal cell count (no increase in WBCs) |
Guillan Barre
"Albuminocytologic Dissociation" |
|
|
|
What anti-seizure drug can be used to increase liver enzyme synthesis in a patient with Crigger Najar?
|
phenobarbitol
|
|
|
|
skip lesions + transmural inflammation
|
crohn's dz
|
|
|
|
skip lesions
granulomas spares rectum |
crohn's dz
|
|
|
|
G+ vs. G-
-Peptidoglycan for support. -Lipoteichoic Acid induces TNF, IL-1, IL-6 |
G+ cell wall/cell membrane
|
|
|
|
G+ vs. G-
-Site of major endotoxin (lipopolysaccharide) -Lipid A induces TNF and IL-1, polysaccharide is the antigen |
G- outer membrane
|
|
|
|
Mediates adherence of bacteria to foreign surfaces such as catheters or tubes
|
glycocalyx
|
|
|
|
Protects bacteria against phagocytosis
|
capsule
|
|
|
|
Bacterial capsules are made of polysaccharide
Except for Bacillus anthracis which has a capsule made of ____ |
D-glutamate
|
|
|
|
This provides rigid support for the bacterial cell and proctects against osmotic pressure differences
|
peptidoglycan
(sugar backbone w/ crosslinked side chains) |
|
|
|
What is the space between the inner and outer cell membranes in G (-) bacteria?
|
periplasm
|
|
|
|
This bacterial structure mediates adherence of bacteria to cells
|
fimbrea/pilus
|
|
|
|
This is a keratin-like coat made of dipicolinic acid and is produced by bacteria in the end of the stationary phase of their life cycle
|
spore
|
|
|
|
What is a bacterial spore made of?
|
dipicolinic acid
|
|
|
|
What type of stain would you use to visualize Cryptococcus neoformans?
|
india ink
|
|
|
|
What stain would you use for Pneumocystis jirovecii?
|
silver stain
|
|
|
|
What type of stain would you use for amyloid?
|
congo red
|
|
|
|
what type of stain would you use for Chlamydia?
|
Giemsa
|
|
|
|
Lipoteichoic acid is unique to Gram ___ bacteria
|
Gram +
(induces TNF, IL-1, IL-6) |
|
|
|
Which has a bigger peptidoglycan membrane? G(+) or G(-) organisms?
|
G +
|
|
|
|
Which has a endotoxin/LPS outer membrane? G(+) or G(-) organisms?
|
G(-)
|
|
|
|
What 2 bugs are "branching filamentous"?
|
Actinomyces
Nocardia |
|
|
|
Use a ____ stain for Legionella
What type of agar? |
silver stain
charcoal auger |
|
|
|
These bacteria have no cell wall, only cell membranes containing sterols
|
Mycoplasma
|
|
|
|
These bugs have cell walls that contain mycolic acid and a high lipid content
|
Mycobacterium (TB, leprae)
|
|
|
|
What bugs do not gram stain well? (6)
"These Bugs May Microscopically Lack Color" |
Treponema
Boriella Mycobacterium Mycoplasma Legionella Chlamydia |
|
|
|
What type of stain is used to diagnose Tropheryma whippelii infection in the distal small intestine?
|
PAS stain
(Periodic acid-Schiff) |
|
|
|
One bug and one fungus that are stained with silver stain
|
Pneumocystis jirovecii
Legionella pneumophilia |
|
|
|
What type of stain do you use for:
Borrelia, Plasmodium, trypanosomes, Chlamydia |
Giemsa
|
|
|
|
What type of stain do you use for Mycoplasma?
|
Ziehl-Neelson
(Acid Fast Stain) |
|
|
|
This bug is grown on a Chocolate Agar with factors V (NAD+) and X (hematin)
|
Haemophilus influenzae
|
|
|
|
This bug is grown on a Lowenstein-Jensen agar
|
Mycobacterium tuberculosis
|
|
|
|
This bug is grown on Eaton's agar
|
Mycoplasma pneumoniae
|
|
|
|
This bug is grown on a charcoal yest extract agar
(buffered with cysteine and iron) |
Legionella pneumophilia
|
|
|
|
An infection with this bug may reactivate after using TNF-α inhibitors (Inflixumab, Etanercept)
It has a predilection for the apices of the lung where the O2 content is high |
Mycobacterium tuberculosis
|
|
|
|
What are the obligate aerobe bacteria? (4)
"Nagging Pests Must Breathe" |
Nocardia
Pseudomonas Mycobacterium tuberculosis Bacillus |
|
|
|
What are the obligate anaerobic bacteria? (3)
"Can't Breathe Air" |
**All lack catalase/Super oxide dismutase**
Clostridium Bacteroides Actinomyces |
|
|
|
What are the two obligate intracellular bacteria?
|
Chlamydia
Rickettsia |
|
|
|
Which bugs are encapsulated? (6)
"Some Killers Have Nice Shiny Bodies" |
Strep pneumo
Klebsiella Haemophilus Neisseria Salmonella group B Strep (agalactiae) |
|
|
|
What test is (+) for encapsulated bacteria?
|
Quellung
|
|
|
|
People with Chronic Granulomatous disease have recurrent infections with ____ (+) bacteria
|
catalase (+)
|
|
|
|
What are the catalase (+) bacteria? (6)
"SSPACE" |
Staph aureus
Serriata Pseudomonas Actinomyces Candida E. coli |
|
|
|
If a vaccine containing polysaccharide capsule chains was NOT conjugated protein, what type of immune response would occur?
|
No T-cell response because a polysaccharide capsule alone would not be presented to T-cells
***Only IgM antibodies would be produced*** |
|
|
|
____ is a polysaccharide vaccine with no conjugated protein
|
Pneumovax
(Strep pneumo) |
|
|
|
_____ is a conjugated capsular polysacharride vaccine
|
HiB (H. influenzae type B)
|
|
|
|
A positive Urea breath test indicates ____ colonization
|
H. pylori
|
|
|
|
this bug produces yellow "sulfur granules"
|
Actinomyces israelii
|
|
|
|
This bug produces a blue-green pigment that smells fruity (grapes)
|
Pseudomonas
|
|
|
|
***HY***
What is the virulence factor for Staph. aureus that binds Fc region of Ig and prevents opsonization and phagocytosis? |
Protein A
|
|
|
|
**HY***
What bugs produce IgA protease? Enzyme that cleaves IgA in order to colonize the respiratory mucosa? (3) "SHiN" |
Strep pneumo
Haemophilus influenza Neisseria |
|
|
|
**HY**
What is Strep pyogenes' (Group A) virulence factor? Helps it to evade phagocytosis |
M protein
|
|
|
|
Exotoxins are _______
Endotoxins are _______ A) Lipopolysaccharides B) Polypeptides |
Exotoxins are Polypeptides
Endotoxins are Lipopolysaccharides (Endotoxins are mostly found in G (-) ) |
|
|
|
This bacteria has Endotoxin A which inactivates EF-2 and causes host cell death
|
Pseudomonas
|
|
|
|
This toxin inactivates EF-2 and causes Pharyngitis and Pseudomembranes in the throat
|
diptheria toxin
(Cornybacterium diptheriae) |
|
|
|
This toxin inactivates the 60s ribosome by cleaving rRNA.
Leads to GI mucosal damage, bloody diarrhea and release of cytokines causing HUS |
Shiga toxin
(Shigella) |
|
|
|
This toxin inactivates the 60s ribosome by cleaving rRNA.
DOES NOT INVADE HOST Causes cytokine release leading to HUS |
Shiga-Like Toxin
(E. coli 0157:H7) |
|
|
|
Enterotoxigenic E. coli (ETEC) has **heat labile toxin** which over-activates ______ leading to watery diarrhea.
It also has a **heat-stabile** toxin that causes watery diarrhea by over-activating ______ |
Heat-Labile: adenylate cyclase, ↑ cAMP
Heat-Stabile: gaunylate cyclase, ↑cGMP |
|
|
|
Y. enterolitica has ___ toxin which activates adenylate cyclase (↑ cAMP) and and causes BLOODY diarrhea by invading and destroying cells
|
Heat-Stabile toxin
|
|
|
|
What is the name of the exotoxin of Bacillus anthracis that **mimics adenylate cyclase enzyme** ( ↑ cAMP)
Causes erythematous borders around black eschar |
Edema Factor
|
|
|
|
What is the mechanism of Edema Factor released by B. anthracis?
|
**mimics adenylate cyclase enzyme**
(↑ cAMP) |
|
|
|
What is the mechanism of Cholera toxin?
|
Over-activates adenylate cyclase (↑ cAMP) by PERMANENTLY ACTIVATING Gs --> "rice water" diarhhea
(Vibrio cholerae) |
|
|
|
This toxin Over-activates adenylate cyclase by (↑ cAMP) by PERMANENTLY INHIBITING Gi
-Impairs phagocytosis to permit survival of microbe |
Pertussis toxin
**WHOOPING COUGH** (Bordatellu pertussis) |
|
|
|
Which bug releases a toxin that prevents the release of inhibitory GABA and glycine neurotransmitters in the spinal cord?
Leads to muscle rigidity |
C. tetani
tetanospasmin |
|
|
|
What is the mechanism by which Botulism toxin and Tetanospasmin prevent neurotransmitter release?
|
cleave SNARE protein
|
|
|
|
This bug produces a toxin that inhibits the RELEASE of ACh into the neuromuscular junction.
Leads to flaccid paralysis |
C. botulinum
Botulism toxin |
|
|
|
What is the exotoxin of Clostridium perfringes responsible for degrading phospholipids and causing **Gas Gangrene**?
|
Alpha toxin
(see **double zone** of hemolysis on blood agar) |
|
|
|
What is the exotoxin produced by Strep pyogenes (GBHS) that lyses RBCs and contributes to β-hemolysis?
|
Streptolysin O
(body makes ASO ab) |
|
|
|
Bacteria release exotoxins that bring MHC II and T-cell receptors into close proximity to each other to cause an overwhelming release of IFN-γ and IL-2 -->SHOCK
|
Superantigens
-Strep pyogenes --> Exotoxin A -Staph aureus --> TSST-1 |
|
|
|
Are ENDOtoxins (G-) heat stabile?
|
Yes
|
|
|
|
Which Staph. aureus toxin causes scalded-skin syndrome?
|
efoliative toxin
|
|
|
|
Which toxin secreted by Strep. pyogenes causes Scarlet Fever?
|
erythrotoxin/pyrotoxin
|
|
|
|
Toxin released by Staph aureus that causes Leukocytosis
|
Leukocidin
|
|
|
|
By what method are plasmids exchanged by bacteria?
|
Sex pilus --> conjugation
|
|
|
|
Which ENDOtoxin (G-) activates Hageman factor?
|
Lipid A
|
|
|
|
These bacteria (4) produce toxins that are ADP-ribosylating A +B toxins.
B component binds to host cell, while the A component attaches ADP-ribosyl to disrupt cell proteins |
Pseudomonas --> Exotoxin A
EHEC --> Heat Labile toxin V. cholerae --> cholera toxin B. pertussis --> pertussis toxin |
|
|
|
Penicillins and Cepahlosporins act on bacteria in the ______ phase as peptidoglycan is being made
|
Exponential Growth Phase
|
|
|
|
What is it called when a bacterium takes up DNA from the environment?
|
**Transformation**
(SHiN bacteria with IgA protease are really good at this) |
|
|
|
What is it called when a bacterium is infected by a viral phage and parts of the bacterial DNA are packed into the virus when it goes off to infect another bacterial cell?
|
**Tranduction**
|
|
|
|
What is it called when a bacterial segment of DNA "jumps" (excision and reincorporation) from one location to the other?
|
**Transposition**
|
|
|
|
Causes dental carries
|
Strep mutans
(Strep viridans group- alpha hemolytic) |
|
|
|
Strep viridans is ____ to optichinin
|
Resistant
|
|
|
|
Strep pyogenes is ___ to optichinin
|
Susceptible
|
|
|
|
This bug is the most common cause of:
Meningitis Otitis Media Pneumonia Sinusitus |
Strep pneumoniae
|
|
|
|
Which type of streptococcus coloonizes the vagina, causes pneumonia, meningitis and sepsis in neonates?
|
Group B Beta-Hemolytic Strep
-Strep agalactiae |
|
|
|
Lancefield group D Steptococci =?
|
Enterococci spp.
|
|
|
|
This bug can cause sub-acute endocarditis in colon cancer patients
|
Strep. bovis
|
|
|
|
Club-shaped gram (+) rods with metachromic (blue+red) granules.
-Use Elek test for toxin |
Cornybacterium diptheriae
(remember, ADP-ribosylation, and a Beta-prophage codes for the exotoxin) |
|
|
|
Where do the GABA and Glycine inhibitory neurotransmiters blocked by tetanus in the spinal cord come from?
|
Renshaw cells
|
|
|
|
Describe the 2 toxins of C. diffiile
|
Toxin A:
binds to brush border Toxin B: destroys cytoskeletal structure of enterocytes |
|
|
|
Faculative intracellular anaerobe acquired by eating unpasteurized milk/cheese and deli meats.
|
Listeria monocytogenes
|
|
|
|
Caseous cavitary lesion in the lung
|
Tuberculosis
**CASEATING GRANULOMA** |
|
|
|
Perihilar lymphadenopathy + caseating granuloma in lung
|
Gohn Complex
**PRIMARY TB INFECTION** |
|
|
|
Prophylactic treatment for Mycobacterium avian-intracellulare (MAC) in an AIDS patient?
|
Azithromycin
|
|
|
|
resevoir in the U.S. is an armidillo
|
Mycobacterium leprae
|
|
|
|
Treatment for M. leprae?
|
Dapsone
|
|
|
|
T cell response Lepromatous M. leprae infection?
|
Th1
|
|
|
|
T cell response for Tuberculoid M. lepreae infection (hypoesthetic skin plaques)
|
Th2
|
|
|
|
Do Neisseria ferment glucose?
|
yes
|
|
|
|
Which Neisseria ferments Maltose
|
N. meningitidis
|
|
|
|
Does N. gonorrhea have a capsule?
How about N. meningitidis? |
N. gonorrhea = no
N. meningitidis = yes |
|
|
|
Superior colliculi lesion
|
paralysis of upward gaze
|
|
|
|
Inferior colliculi lesion
|
hearing issues
|
|
|
|
What causes Epiglottitis
(+) thumb sign |
Haemophilus Influenzae type B
|
|
|
|
Tx. for Legionella pneumophilia?
|
erythromycin
|
|
|
|
DOC for Haemophilus influenzae
|
ceftriaxone
|
|
|
|
Aerobic, G (-) rod, non-lactose fermenter, oxidase positive
|
Pseudomonas
|
|
|
|
E. coli virulence factor for cystitis and pyelonephritis
|
fimbriae
|
|
|
|
E.coli virulence factor for pneumonia and meningitis
|
k capsule
|
|
|
|
Salmonella Vs. Shigella
-Produces H2S4 |
Salmonella
|
|
|
|
Bloody Diarrhea
-poultry, meat, unpasteurized milk -Comma or S-shaped, grows at 42*C |
Campylobacter jejuni
|
|
|
|
-Pet feces, contaminated milk, pork
-G (-) -outbreaks of diarrhea common at day-care centers |
Yersinia enteroliticus
|
|
|
|
-Question mark shaped G (-)
-found in water contaminated with animal urine Flulike symptoms, jaundice, photophobia with conjunctivitis. -Surfers in the Tropics |
Leptospira interrogans
|
|
|
|
"bullseye" rash with central clearing (erythema chronicum migrans)
Joint pain, headache |
-Lyme Dz
Borrelloa burgdorferi |
|
|
|
DOC for Lyme Dz
|
doxycycline or ceftriaxone
|
|
|
|
Darkfield microscopy
|
Treponema pallidum
|
|
|
|
DOC for Treponema pallidum
|
Penicillin G
|
|
|
|
Rash on the palm and soles is seen with what? (3)
|
Coxsackie A
Rickettsia rickettsi Syphillis (Treponema) |
|
|
|
Oncogenes:
abl |
CML
------------------------------------ Gene product? |
tyrosine kinase
|
|
|
Oncogenes:
c-myc |
Burkitt Lymphoma
--------------------------------- Gene product? |
transcription factor
|
|
|
Oncogenes:
bcl2 |
Follicular and undifferentiated lymphomas
(inhibits apoptosis) --------------------------- Gene product? |
Anti-apoptotic molecule
|
|
|
Oncogenes:
-erb-B2 |
Breast, ovarian, gastric carcinoma
-------------------------------- Gene product? |
tyrosine kinase
|
|
|
Oncogenes:
ras |
Colon cancer
----------------------------- Gene product? |
GTPase
|
|
|
Oncogenes:
L-myc |
Lung tumor
------------------------------- Gene product? |
Transcription factor
|
|
|
Oncogenes:
ret |
MEN types 2A, 2B, Medullary Thyroid CA
------------------------- Gene Product? |
tyrosine kinase
|
|
|
Oncogenes:
c-kit |
Gastrointestinal stromal tumor
----------------------------------- Gene product? |
cytokine receptor
|
|
|
Oncogenes:
N-myc |
Neuroblastoma (Adrenal)
----------------------------- Gene product? |
transcription factor
|
|
|
Which tumor marker would you use to follow the progression of Colon Cancer?
|
CEA
|
|
|
|
What tumor marker would you use to monitor treatment of a Neuroblastoma (Adrenal) ?
|
Bombesin
|
|
|
|
Anti-presynaptic Ca++ antibodies
|
Lambert Eaton Syndrome
-Small cell lung CA -Also thymomas |
|
|
|
How can tumor cells induce apoptosis of T-cells?
|
FasL
|
|
|
|
What types of receptors relax renal vascular smooth m.?
|
D1--->Gs--> ↑cAMP --> ↑ protein kinase A --> (-) myosin light chain kinase
|
|
|
|
What receptors are found in the neuromuscular junction and autonomic ganglia?
|
Nicotonic receptors
ACh binds---> (+) Na+/K+ ligand gated channel |
|
|
|
Are nicotinic receptors G-coupled receptors?
|
No
The (+) Na+/K+ ligand gated channel |
|
|
|
How do H2 receptors increase gastric acid secretion?
|
Facilitate K+ resorption, which means for every K+ absorbed, a H+ is released into the lumen
Bind to Gs --> (+) adenylate cyclase --> ↑cAMP --> ↑ protein kinase A |
|
|
|
What are the Gq coupled receptors?
|
H1
α1 V1 M1 M3 "HAVe 1 M&M" |
|
|
|
What are the Gi coupled receptors?
|
M2
α2 D2 "MAD 2's" |
|
|
|
What are the Gs coupled receptors?
|
β1
β2 H2 V2 D1 |
|
|
|
What type of drugs are these?
-Bethanechol -Carbachol -Pilocarpine -Methacholine |
Direct Muscarinic Agonists
(↑ PNS activity) |
|
|
|
What types of drugs are these?
-Neostigmine -Pyridostigmine -Edrophonium -Physostigmine -Echothiphate -Donepezil |
AChE inhibitors
(↑ PNS activity) |
|
|
|
Antidote for organophosphate poisoning?
|
Atropine + Pralidoxime
|
|
|
|
What are the side effects of Atropine overdose?
|
Hot as a hare (↓ sweat)
Dry as a bone (dry mouth, urine retention) Blind as a bat (mydriasis) Red as a beet (flushing) Mad as a hatter (delirium) |
|
|
|
What types of drugs are clonidine and α-methyldopa?
|
α2 central agonists
(decrease central SNS flow) |
|
|
|
What drug would you give to someone who is depressed and refuses to eat?
|
Mirtazapine
α2-blocker that increases appetite |
|
|
|
How do Beta-blockers affect renin release from JG cells?
|
↓ renin release
|
|
|
|
If you were to increase the radius of a blood vessel 2x, how would that effect resistance of flow?
|
↓ resistance 16x
|
|
|
|
If you were to decrease the size of a blood vessel to 1/2 it's radius, how would that effect resistance of flow?
|
↑ resistance 16x
|
|
|
|
What are the waveforms of the Jugular venous pulse?
|
a = RA contracts
c = RV contracts x = RA relaxes (during RV contraction) v = RA fills y = RA empties to RV "At Carter's X (crossing), Vehicles Yield" |
|
|
|
When does Isovolumetric Contraction occur in the cardiac cycle?
|
After mitral valve closes and before aortic valve opens...
So, LV is contracting, but the aortic valve is closed so you're not affecting the volume in the LV |
|
|
|
When does isovolumetric relaxation occur in the cardiac cycle?
|
After aortic valve closes, before mitral valve opens...
You've pushed everything out, there's nothing left in the LV After the Mitral valve opens back up, rapid ventricular filling can occur |
|
|
|
Why does normal S2 splitting occur during inspiration?
|
When you inhale, you ↓ intrathoracic pressure.
This drop in pressure causes an ↑ in preload, and in ↑ in the amount of blood in the RV. As a result, the RV takes longer to push out all the blood and the PULMONIC VALVE CLOSES LATER THAN THE AORTIC VALVE |
|
|
|
Crescendo-decrescendo systolic murmur heard in the 2nd-3rd right IC space, close to sternum
|
Aortic Stenosis
|
|
|
|
Early diastolic decrescendo murmur best heard along the left side of the apex.
|
Pulmonic Regurge
|
|
|
|
Late diastolic decrescendo murmur best heard along the left side of the apex.
|
Tricuspid Stenosis
|
|
|
|
Pancystolic (Holosystolic) murmur best heard at the apex and radiates to the axilla
|
Mitral Regurge
|
|
|
|
Late systolic murmur preceded by a mid-systolic click
|
MVP
|
|
|
|
Crescendo-decrescendo systolic murmur heard in the 2nd-3rd left IC spaces close to the sternum
|
Pulmonic Stenosis
|
|
|
|
Pansystolic (holosystolic) murmur heard best along the left lower sternal border and radiates to right sternal border
|
Tricuspid Regurge or VSD
|
|
|
|
Pansystolic (holosystolic) murmur heard best along the left 4th-6th intercostal spaces
|
Tricuspid Regurge or VSD
|
|
|
|
Rumbling late diastolic murmur with an opening "snap"
|
Mitral Stenosis
|
|
|
|
High-pitched diastolic murmur associated with widened pulse pressure and "head bobbing"
|
Aortic Regurge
(Syphilis, Marfans) |
|
|
|
Ventricular tachycardia with *sinusoidal waveforms** =
|
Torsades de Pointes
d/t prolonged QT (Na+ & K+ channel conductance) |
|
|
|
Why would you give a pt. in A-fib warfarin?
|
Prophylaxis against thromboembolism
|
|
|
|
What is Atrial natriuetic peptide's action on the efferent and afferent renal arterioles?
|
Afferent: DILATES
Efferent: CONSTRICTS Diuresis occurs as a result. Helps to curb effects of ↑↑ aldosterone in Conn Syndrome |
|
|
|
A pulmonary capillary wedge pressure (PCWP) > than LV diastolic pressure indicates what valve problem?
|
Mitral Stenosis
|
|
|
|
In the lungs, hypoxia causes ____ so only the will ventilated areas are prefused
|
vasoconstriction
|
|
|
|
If there are ↓ plasma proteins, that means there is ↓ ____ pressure pulling fluid into the vascular system..
The result is edema in the form of nephrotic syndrome or renal failure |
↓ plasma oncotic pressure (↓πc)
|
|
|
|
What change in pressure causes edema in CHF?
|
↑ capillary pressure
↑ pressure causes fluid to leak from the capillaries into the interstitium |
|
|
|
Edema caused by toxins or burns is due to ↑ ______
|
↑ capillary permeability (↑Kf)
|
|
|
|
Lymphatic blockage causes a ↑ in _____ pressure causing fluid to be pulled from systemic circulation and into the interstitium
|
↑ interstitial osmotic pressure
↑ interstitial osmotic pressure (more proteins) draws fluid from vasculature into the interstitium |
|
|
|
What are the 5 T's that cause early cyanosis in newborns?
|
Truncus arteriosus
Tetralogy of Fallot Transposition of great vessels Tricuspid Atresia Total Anomalous Pulmonary Venous return (TAPVR) |
|
|
|
Kid comes in with late cyanosis.
You hear a loud S1 and a fixed, split S2 |
ASD
|
|
|
|
What heart anomaly can occur to babies born to diabetic mothers?
|
Transposition of the great vessels
|
|
|
|
This heart anomaly is due to failure of the aorticopulmonary septum to spiral (Neural crest)
|
Transposition of the great vessels
|
|
|
|
This heart anomaly is connected with Turner's Syndrome?
|
Coarctation of the Aorta
|
|
|
|
Infantile Coarctation of the Aorta occurs PROXIMAL (before) the _________
|
ligamentum arteriosum
|
|
|
|
Coarctation of the Aorta is most commonly associated with what valve problem?
|
Bicuspid aortic valve
|
|
|
|
Which congenital cardiac anomaly is related to:
-22q1 deletions |
Truncus arteriosus
Tetralogy of fallot |
|
|
|
Which congenital cardiac anomaly is related to:
-Down Syndrome |
endocardial cushion defects
(VSD, ASD, AV septal defect) |
|
|
|
Which congenital cardiac anomaly is related to:
-Congenital Rubella |
PDA
Pulmonary a. stenosis |
|
|
|
Which congenital cardiac anomaly is related to:
Marafan's |
Aortic Insufficiency
(dilation of aortic root) |
|
|
|
Why are Turner Syndrome patients at an increased risk for subacute bacterial endocarditis?
|
bicuspid aortic valve
|
|
|
|
Foam cells are macrophages seen in ____
|
atherosclerosis
|
|
|
|
Hyaline arteriolosclerosis is seen in patients with long-standing ____ or ____ and causes hyaline thickening of small arteries and hyperplastic "onion skinning" in episodes of malignant hypertension
|
longstanding HTN
diabetes |
|
|
|
Longstanding hypertension may result in hyaline arteriosclerosis of the ________ and weaken the media of the aorta.
This can lead to an aortic aneurysm.. |
vasa vasorum
(supply the media of the aorta with blood) |
|
|
|
_____ angina shows ST depression on EKG
|
Stable angina
(secondary to atherosclerosis) |
|
|
|
_____ angina shows ST elevation on EKG
|
Prinzmetal's Angina
(secondary to CORONARY VASOSPASM) |
|
|
|
What is the most common cause of death one hour after an MI?
|
Lethal arrythmia
|
|
|
|
The heart undergoes _____ necrosis if damaged
|
coagulative necrosis
|
|
|
|
What presents as chest pain with a friction rub following an MI?
|
Fibrinous pericarditis
|
|
|
|
If an MI causes subendocardial necrosis in less than 50% of the myocardial wall, what will be seen on EKG?
|
ST-depression
|
|
|
|
If an MI causes transmural necrosis of the entire mycoardial wall, the EKG will show ______
|
ST-elevation
|
|
|
|
What appears at the margins of an MI 5-10 days after?
|
Granulation tissue
(Macrophages have removed dead tissue making it weak and more susceptible to papillary free wall rupture) |
|
|
|
ST-elevation and Abnormal Q waves signifies a ____ MI
|
Transmural MI
|
|
|
|
Dilated cardiomyopathy causes a ____ heart sound and systolic dysfunction
|
S3
(causes: chronic alcohol, Coxsackie B, Cocaine, Chagas, Doxorubicin toxixity) |
|
|
|
Hypertrophic cardiomyopathy causes a ____ hear sound and diastolic dysfunction
|
S4
|
|
|
|
Disordered, tangled, hypertrophied myocardial fibers
|
hypertrophic cardiomyopathy
|
|
|
|
What should you think if you see a low-voltage EKG with a diminished QRS amplitude
|
Restrictive Cardiomyopathy
decreased compliance leads to shitty filling of the heart during diastole (Causes: sarcoidosis, amyloidosis, post-radiation, endocardial fibreolastosis) |
|
|
|
What is the cause of orthopnea in a patient with Left CHF?
|
↑ Venous Return in supine position exacerbates pulmonary congestion
|
|
|
|
A patient with SLE has sterile vegetations on BOTH sides of the mitral valve... What's up?
|
Libman Sacks endocarditis
|
|
|
|
Staph aureus most commonly effects which heart valve?
|
tricuspid
|
|
|
|
Which bug causes bacterial endocarditis on prosthetic heart valves?
|
Staph. epidermitis
|
|
|
|
Which bug infects previously damaged heart valves?
|
Strep. viridans
|
|
|
|
What bug causes endocarditis in people with colon cancer?
|
Strep. bovis
|
|
|
|
You suspect endocarditis but the blood culture is negative, what organisms could be causing it?
|
HACEK Bugs
-Haemophilus -Actinobaccilus -Cardiobacterium -Eikenella -Kingella |
|
|
|
IV drug use endocarditis caused by S. aureus, Pseudomonas or Candida spp.most commonly infects which valve?
|
tricuspid
|
|
|
|
Which valve is most likely to be infected in bacterial endocarditis?
|
Mitral valve
|
|
|
|
What antibodies are seen in rheumatic fever?
|
anti-M protein
M protein mimics myocytes so body attacks its own myocytes |
|
|
|
What are the major Jones criteria for rheumatic fever?
|
J-joints
♡-Pancarditis N- Nodules (SubQ) E- Erythema marginatum S- St. Vitus' Dance (chorea) |
|
|
|
A patient presents with sharp chest pain aggrevated by inspiration.
He leans forward to decrease the pain. Auscultation reveals a friction rub and EKG shows ST-elevation in all 12 leads. |
Acute pericarditis
|
|
|
|
Temporal arteritis causes granulomatous inflammation of the branches of the ____ artery
Biopsy shows an inflamed vessel wall with giant cells in the INTIMA. |
carotid arteries
**may involve joint pain and stiffness in proximal joints = polymyalgia rheumatica** |
|
|
|
Takayasu's arteritis causes granulomatous thickening of the ________.
Classically presents as the "pulseless disease" (weak UE pulses) |
aortic arch
|
|
|
|
This medium vessel vasculitis is associated with Hepatitis B.
Causes FIBRINOID necrosis of vessels leading to multiple organs (spares the lungs) It is immune complex mediated. "String of pearls" sign on angiogram due to fibrosis and subsequent dilation of vessels. Presents with Fever, weight loss, malaise, abdominal pain, melana, neurologic dysfunction and cutaneous eruptions |
Polyarteritis Nodosa
****(-) p-ANCA **** |
|
|
|
Granulomatous
URI symptoms, sinusitis Hemoptysis, cough Renal = hematuria and red cell casts (+) c-ANCA |
Wegener's Granulomatosis
(+) c-ANCA |
|
|
|
Non-granulomatous inflammation of small vessels
-no Nasal/URI involvement -may involve lungs and kidneys (+) p-ANCA |
Microscopic polyangitis
|
|
|
|
Asthma, sinusitis palpable purpura and peripheral neuropathy (wrist/foot drop)****
-Granulomatous vaculitis with EOSINOPHILIA (+) p-ANCA |
Churg-Strauss syndrome
|
|
|
|
This is a highly lethal liver malignancy.
Associated with vinyl chloride, arsenic and ThO2 (Thorotrast) exposure |
Angiosarcoma
|
|
|
|
What are benign skin papules found in AIDS patients due to Bartonella henselae infections called?
|
Bacillary angiomatosis
(confused for Kaposi's) |
|
|
Explain whats going on in Phase 0-4
|
Phase 0
voltage gated Na+ channels open Phase 1 Na+ channels close. K+ channels open Phase 2 Ca++ channels open and balance K+ efflux Phase 3 massive efflux of K+ due to opening of slow K+ channels. Ca++ channels close Phase 4 high permeability through K+ channels |
|
|
|
Pancreas:
-What do pancreatic α cells, β cells, and δ cells secrete? |
α cells = Glucagon
β cells = Insulin δ cells = Somatostatin |
|
|
|
What types of receptors are utilized by insulin and IGF-1?
|
Intrinsic Tyrosine Kinase Receptors
|
|
|
|
What types of signaling pathways are used by FSH, LH, ACTH, hCG, PTH and ADH and glucagon?
|
cAMP
|
|
|
|
What type of steroid receptor is used for Vit. D, Estrogen, Testosterone, Cortisol, Aldosterone and Progesterone
|
Cytosolic Steroid receptor
|
|
|
|
What type of steroid receptor is used for T3/T4?
|
Nuclear Receptor
|
|
|
|
What is the result of ↑ SHBG in men?
|
↑ SHBG --> binds free Testosterone --> Gynecomastia
|
|
|
|
What is the result of ↓ SHBG in women?
|
↓ SHBG --> more free testosterone unbound
leads to hirsutism |
|
|
|
What will ACTH levels be like in a patient with Cushing Disease (pituitary adenoma)?
|
↑ ACTH being pumped out by tumor
|
|
|
|
What will ACTH levels be like in a patient with Cushing's Syndrome due to a cortisol-producing adrenal adenoma?
|
↓ ACTH
|
|
|
|
What is the rule of 10's for pheochromocytoma?
|
10% malignant
10% bilateral 10% extra-adrenal 10% calcify 10% kids 10% familial |
|
|
|
What marker do you find in the urine that would suggest a Neuroblastoma (adrenal) in a kid?
|
HVA
(breakdown marker of dopamine) |
|
|
|
Pretibial myxedema is seen in _______
|
Grave's Dz
(hyperthyroid) |
|
|
|
What is the most common Thyroid CA?
|
Papillary Thyroid CA
----------------------------------- -"Ground-glass" nuclei (Orphan Annie) -PSAMMOMA BODIES -Nuclear grooves |
|
|
|
Which thyroid CA is associated with amyloid sheets composed of calcitonin?
|
Medullary Thyroid CA
----------------------------------- -Parafollicular C cells - assoc w/ MEN 2A + MEN 2B |
|
|
|
The ret gene mutation is associated with which two forms of thryoid CA?
|
Medullary Thyroid CA
Papillary Thyroid CA |
|
|
|
What is the mechanism of hyperpigmentation in Addison's Disease?
|
Addison's = Primary Adrenal Insufficiency
-Adrenal atrophy = no corisol or aldosterone - ↑ ACTH production from Ant. Pituitary - POMC needed to make ACTH also stimulates MSH to increase melanocyte producton |
|
|
|
Patient presents one week after a recent flu-like illness.
They complain of jaw pain and have a tender thyroid to palpation |
Subacute Thyroiditis
(de Quervain's) |
|
|
|
What is the name given to a thyroid-secreting teratoma?
|
Struma Ovari
-contains thyroid tissue, presents as hyperthryroidism |
|
|
|
Are you hyper- or hypo- natreminc when you have SIADH
|
hyponatremic
You are reabsorbing too much water and diluting your serum sodium |
|
|
|
Urine osmolarity > Serum osmolarity
|
SIADH
|
|
|
|
In which type of Diabetes Mellitus would you see:
-Islet amyloid deposit |
Type II DM
|
|
|
|
In which type of Diabetes Mellitus would you see
-Islet lymphocytic infiltrate |
Type I DM
|
|
|
|
What is the most common tumor of the appendix?
-Derived from neuroendocrine cells |
Carcinoid Tumor
|
|
|
|
Increased 5-HIAA in urine
|
Carcinoid Syndrome
|
|
|
|
Which MEN syndrome is associated with Zollinger-Ellison syndrome?
|
MEN 1
|
|
|
|
What does a Zollinger-Ellison tumor secrete?
|
Gastrin --> hyperacidity of the stomach and RUGAL THICKENING
|
|
|
|
What tumors are associated with MEN type I?
**Commonly presents with kidney stones and stomach ulcers** |
Pituitary Adenomas
Parathyroid tumors Pancreatic Tumors (Zollinger-Ellison) |
|
|
|
What tumors are associated with MEN 2A?
|
Parathyroid tumors
Pheochromocytoma Medullary Thyroid CA |
|
|
|
What tumors are associated with MEN 2B?
|
Oral/intestinal ganglioneuromatosis
Pheochromocytoma Medullary Thyroid CA |
|
|
|
Name the retroperitoneal organs
"SAD PUCKER" |
Suprarenal (Adrenal) Glands
Aorta Duodenum Pancreas (except tail***) Ureter Colon (Descending + Ascending) Kidneys Esophagus (lower 2/3) Rectum (upper 2/3) |
|
|
|
What is the portal triad?
What ligament holds the portal triad? |
**Triad**
1) Common Bile duct 2) portal vein 3) proper hepatic a. **Hepatoduodenal Ligament** |
|
|
|
What ligament connects the liver to the abdominal wall?
What is it a remnant of? |
Falciform ligament
**Derived from Umbilical Vein** |
|
|
|
The submucosa of the gut wall contains the _____ plexus
|
Meissner's Plexus
|
|
|
|
The muscularis of the gut wall contains the _____ plexus
|
Auerbach's plexus
|
|
|
|
Brunner's glands are located in the _____ and serve to secrete an alkaline rich secretion to protect the rest of the GI tract from stomach acid
|
Duodenum
|
|
|
|
Peyer's patches are normally found in which portion of the small intestine?
They are located in the submucosa and lamina propria |
Ileum
|
|
|
|
Which portion of the small intestine has neither Brunner's glands or Peyer's patches?
|
Jejunum
|
|
|
|
The ____ artery supplies the Stomach to proximal duodenum, liver, gallbladder, pancreas, spleen
|
celiac artery
**Foregut** |
|
|
|
The ____ artery supplies the distal duodenum to proximal 2/3 of the transverse colon
|
SMA
**Midgut** |
|
|
|
The ____ artery supplies the Distal 1/3 of the transverse colon to upper portion of rectum
(splenic flexure is watershed area) |
IMA
|
|
|
|
Name the 3 main branches of the celiac trunk
|
Common Hepatic a.
Splenic a. L. gastric a. |
|
|
|
Why are internal hemorrhoids NOT painful?
|
They are above the pectinate line and receive visceral innervation.
|
|
|
|
Why are external hemorrhoids PAINFUL?
|
They are below the pectinate line and receive innervation from the inferior rectal branch of the pudendal nerve.
|
|
|
|
Internal vs. External Hemorrhoids:
-sign of portal HTN |
Internal Hemorrhoids
----------------------------------------- Internal hemorrhoids drain to the superior rectal vein which drains to the portal system External hemorrhoids drain to the inferior rectal vein --> internal pudendal v. --> internal ilac v. --> IVC |
|
|
|
Failure of the ________ to close may result in an indirect inguinal hernia.
**LATERAL to inferior epigastric a.*** |
Processus Vaginalis
|
|
|
|
A direct inguinal hernia will go through the _____ ring
|
Superficial inguinal ring
------------------------------------ An indirect hernia will enter the internal inguinal ring and travel with the spermatic cord down into the scrotum |
|
|
|
What 2 amino acids are potent stimulators of Gastrin release from G cells in the antrum of the stomach?
|
Phenylalanine and tryptophan
|
|
|
|
Explain why an oral glucose load is used more rapidly than an IV glucose load.
|
K cells in the duodenum/jejunum sense glucose and secrete **Gastric Inhibitory Peptide** which ↑ insulin release
↑ insulin utilizes the glucose more quickly |
|
|
|
What is the purpose of Pepsin produced by chief cells in the stomach?
|
protein digestion
|
|
|
|
What is the most common tumor of the salivary glands?
-Composed of stromal (cartilage) and epithelial tissue |
Plepmorphic Adenoma (benign)
-Arises in **parotid gland** but DOES NOT affect CN 7 -HIGH RATE OF RECURRENCE (Surgeon misses some of the tumor) |
|
|
|
What type of salivary gland tumor has:
-Abundant lymphocytes with germinal centers (lymph-node like stroma)? -Almost always arises from parotid gland |
Warthin Tumor (benign)
|
|
|
|
What is the most common malignant tumor of the salivary gland?
-Contains squamous + mucinous cells -Commonly involves the facial n. (CN 7) |
Mucoepidermoid Carcinoma
|
|
|
|
-Failure of LES to relax as a result of the loss of Auerbach's (myenteric) Plexus.
-High LES opening pressure --Trouble swallowing liquids + solids |
Achalasia
"Bird Beak" seen on barium swallow |
|
|
|
What type of things would a person with esophageal webs have trouble swallowing?
|
Solids (food) only..
(obstruction) |
|
|
|
Which type of CA occurs in the upper 2/3 of the esophagus?
|
Squamous Cell
|
|
|
|
Which type of CA occurs in the lower 1/3 of the esophagus?
|
Barret's Esophagus --> Adenocarcinoma
|
|
|
|
Malabsorption Syndrome:
-PAS(+) foamy macrophages in intestinal LAMINA PROPRIA - (+) mesenteric nodes -Steatorrhea b/c chylomicrons can't be offloaded from enterocytes to lymphatics - Arthralgias, cardiac symptoms are common |
Whipple's Dz
T. whippelii (GRAM +++) |
|
|
|
What skin rash is common with Celiac Sprue?
|
dermatitis herpetiformis
(IgA deposition at tips of dermal papillae) |
|
|
|
Which part of the small bowel is tropical sprue most likely to infect?
|
Jejunum + Ileum
(distal small bowel) |
|
|
|
What may be a consequence of tropical sprue due to destruction of the ileum and jejunum?
|
Vit. B12 and Folate deficiency
|
|
|
|
Which type of gastritis would you expect to find in a patient with RA taking heavy doses of NSAIDs?
|
Acute Gastritis
(NSAIDs decrease PGs which help to protect the mucous linings!) |
|
|
|
What is a Curling Ulcer in the stomach?
|
Patient suffers a BURN --> hypovolemia
Hypovolemia --> ↓ Blood supply to stomach |
|
|
|
What is a Cushing's ulcer in the stomach?
|
↑ ICP --> (+) vagus nerve --> ↑ stomach acid production
|
|
|
|
Type __ chronic gastritis is autoimmune and affects the body/fundus***
-Anti-parietal cell Ab, and Anti-IF Ab -Achlorydia with ↑ Gastrin levels from G-cell Hyperplasia*** -May ↑ Goblet cells --> Gastric adenocarcinoma ** |
Type A Chronic Gastritis
(Autoimmune) |
|
|
|
What type of hypersensitivity is seen in Type A (autoimmune) Chronic Gastritis ?
|
Type IV
(T-cell mediated) |
|
|
|
Type B Chronic gastritis is caused by H. pylori colonization in the ____ of the stomach
|
antrum
|
|
|
|
(+) urea breath test = ?
|
H. pylori infection
|
|
|
|
If a peptic ulcer in the duodenum eats through the entire posterior intestinal wall, it may damage the _____ artery
|
gastroduodenal a.
(branch of common hepatic a. from Celiac trunk) **Can also cause acute pancreatitis** |
|
|
|
-Gastric hypertrophy with protein loss
-Parietal cell atrophy and ↑ mucous cells -Rugae of stomach are so hypertrophied they resemble brain gyri*** |
Menetrier's Disease
|
|
|
|
Epigastric pain that improves with meals
|
Duodenal ulcer
|
|
|
|
Epigastric pain that increases with meals
|
Gastric ulcer
|
|
|
|
Ruptures of gastric ulcers carry risk of bleeding from damage to the ___ artery
|
L. gastric artery
|
|
|
|
Which form of GI cancer is a/w dietary nitrosamines** (smoked foods)?
(Japan)** |
Intestinal Gastric Carcinoma
|
|
|
|
Involvement of left supraclavicular node d/t mets from the stomach
|
Virchow Node
|
|
|
|
Bilateral mets to the ovaries from stomach, abundant mucous and **signet ring cells**
|
Krukenberg's Tumor
|
|
|
|
Stomach mets to subcutaneous periumbilical lymphnodes
|
Sister Mary Joseph's Nodule
|
|
|
|
What skin sign do gastric carcinomas often create at the base of the neck?
|
Acanthosis nigricans
|
|
|
|
What are two primary forms of cancer that you see **Signet ring** cells?
|
Stomach CA (Diffuse)
Lobular Breast CA |
|
|
|
Gastric vs. Duodenal ulcers
-No risk of cancer |
Duodenal ulcer
|
|
|
|
what blood type is associated with stomach CA?
|
Type A
|
|
|
|
What is the "triple therapy" for H. pylori?
|
-PPI (-prazole)
-clarithromycin -amoxicillin (use metronidazole if pt. allergic to penicillins) |
|
|
|
Granulomas seen in Crohn's Dz are mediated by which type of T-helper cells?
|
Th1
(Th1 + Macrophages = granuloma) |
|
|
|
Crohn's Dz Vs. Ulcerative Colitis
-may see calcium oxolate nephrolithiasis |
Crohn's
|
|
|
|
Crohn's Dz Vs. Ulcerative Colitis
- associated with HLA-B27 and Jewish descent |
Crohn's
|
|
|
|
Crohn's Dz Vs. Ulcerative Colitis
-associated with (+) p-ANCA and primary sclerosing cholangitis |
UC
|
|
|
|
Crohn's Dz Vs. Ulcerative Colitis
-Crypt abscesses |
UC
|
|
|
|
Crohn's Dz Vs. Ulcerative Colitis
-loss of haufstra |
UC
"lead pipe" |
|
|
|
Crohn's Dz Vs. Ulcerative Colitis
-associated with bladder infections |
Crohn's
**fistulas** |
|
|
|
Common cause of appendicitis in kids?
|
lymphoid hyperplasia
|
|
|
|
Meckel's diverticulum is an outpouching of ______
|
**all three gut layers**
-Mucosa -Submucosa -Muscularis propria ** failure of vitelline duct to involute** |
|
|
|
-Colon pathology related to ↑ intraluminal pressure (constipation, straining)
-Many outpouchings -Most often in sigmoid colon |
Diverticulosis
|
|
|
|
What is a Zenker's Diverticulum?
|
Herniation of mucosal tissue*** at junction of pharynx and esophagus.
-hallotosis, obstruction, dysphagia (FALSE DIVERTICULUM) |
|
|
|
What two types of tissue might be found in a Meckel's diverticulum?
|
Pancreatic or Gastric tissue
|
|
|
|
Buzzword:
**currant jelly stools** |
intussusception
|
|
|
|
-Failure of Neural crest cells to migrate
-see dilated megacolon with failure to pass stool -↑ risk in Down Syndrome |
Hirschsprung's Dz
(absent Auerbach + Meissner's Plexus) |
|
|
|
What is the most common cause of ischemic colitis?
|
Atherosclerosis of the SMA
-Splenic Flexure is most common area (watershed) |
|
|
|
A patient has Familial Adenomatous Polyposis + osseous +soft tissue tumors and retinal hyperplasia
|
Gardner's Syndrome
|
|
|
|
A patient has Familial Adenomatous Polyposis + a malignant CNS tumor (medulloblastoma)
|
Turcot Syndrome
|
|
|
|
This form of colon cancer features micro-satellite instability due to a defect in DNA mismatch repair
|
Hereditary non-polyposis colorectal cancer
** increased risk for breast, ovarian and endometrial cancer** |
|
|
|
What is the APC/β-catenin pathway that leads to colorectal cancer?
|
loss of APC gene
↓ k-ras mutation ↓ loss of p53 ----------------------------------------- Start seeing polyps after k-ras mutation ***p53 loss is mediated by ↑COX (asprin will hault this*** |
|
|
|
Reye's syndrome causes _____ damage of hepatocytes
|
mitochondrial damage
**Seen when Aspirin is given to kids*** -Aspirin metabolites ↓ β-oxidation by mitochondrial enzymes |
|
|
|
This is a benign tumor of hepatocytes
-Associated with OCP use and regresses when OCPs are stopped |
Hepatic Adenoma
(Tumors are subcapsular and grow with exposure to estrogen** |
|
|
|
-Jaundice, tender hepatomegaly
-ascites -polycythemia + hypoglycemia - ↑ α-fetoprotein |
hepatocellular carcinoma
|
|
|
|
-Occlusion of IVC or hepatic veins with centrilobular necrosis
-leads to congestive liver disease -May develop varices and be able to see abdominal and back veins |
Budd-Chiari Syndrome
|
|
|
|
(+) PAS globules in liver --> cirrhosis
- Emphysema in lungs |
α-1 antitrypsin deficiency
|
|
|
|
Hereditary CONJUGATED Bilirubinemia
|
-Dubin-Johnson
-can't excrete conjugated bilirubin from liver |
|
|
|
-Mutation of HFE gene
-Triad: cirrhosis, secondary diabetes, hyperpigmentation |
Hemochromatosis
|
|
|
|
What will ferritin, TIBC, Serum Iron, and % Iron saturation look likein a patient with Hemochromatosis?
|
↑ Ferritin
↓ TIBC ↑ Serum iron ↑ % Saturation |
|
|
|
"Onion Skin" bile duct fibrosis
Alternating strictures with dilation causing a "Beading" of bile ducts (+) p-ANCA Associated with Ulcerative Colitis |
Primary Sclerosing Cholangitis
|
|
|
|
-Pruritus, jaundice, dark urine (tea colored), light stool
-hepatosplenomegaly -Anti-mitochondrial Ab, including IgM |
Primary Biliary Cirrhosis
|
|
|
|
Is alcohol a risk factor for pancreatic carcinoma?
|
No, but tobacco is...
|
|
|
|
This drug is a long-acting somatostatin analog used for acromegaly, variceal bleeds, carcinoid tumors and VIPomas
|
Ocreotide
|
|
|
|
What does anisocytosis mean?
|
varying sizes of RBCs
|
|
|
|
What does poikilocytosis mean?
|
varying shapes of RBCs
|
|
|
|
What is the lifespan of an RBC?
|
120 days
|
|
|
|
Platelets are derived from _____
|
megakaryocytes
(fragment off) |
|
|
|
Platelet glycoprotein that binds to vWF?
|
Gp1b
|
|
|
|
Platelet glycoprotein that binds to fibrinogen?
|
G2b/3a
|
|
|
|
What is the WBC differential from highest to lowest?
|
Neutrophils (57-67%)
Lymphocytes (23-33%) Monocytes (3-7%) Eosinophils (1-3%) Basophils (0-1%) "Neutrophils Like Making Everything Better" |
|
|
|
Where do you see hyper-segmented PMNs?
|
Megaloblastic anemia
(↓ B12 + Folate) |
|
|
|
These WBCs are marked with CD40 + CD14
|
Macrophages
|
|
|
|
These blood cells can bind to the Fc portion of IgE
|
Mast Cells
|
|
|
|
Multiple myeloma is a ____ cell neoplasm
|
plasma cell neoplasm
----------------------------------- -abundant RER -chromatin = "clock-face" |
|
|
|
"A" antigen on RBCs and "B" antibodies in plasma
|
Type A
|
|
|
|
"B" antigen on RBCs and "A" antibody in the blood
|
Type B
|
|
|
|
Both "A+B" antigens on RBCs and NO antibodies in plasma.
"Universal recipient" |
Type AB
|
|
|
|
Neither "A" or "B" antigens on RBCs, but "A+B" antibodies in the plasma.
"Universal donor" |
Type O
|
|
|
|
Why is it that a mom can carry a baby with a different bloodtype than her own?
Say, a type A blood mom is having a Type AB baby and this wouldn't cause a reaction. |
anti-AB antigbodies are IgM
DO NOT CROSS PLACENTA |
|
|
|
What clotting factors does Antithrombin inactivate?
|
II, VII, IX, X + XI & XII
(1972 +11+12) |
|
|
|
Warfarin inhibits what enzyme?
|
epoxide reductase
(enzyme that activates Vit. K) |
|
|
|
How does Clopidogrel block thrombus formation?
|
Blocks ADP
-By blocking ADP the platelet cannot express GpIIb/IIIa needed for fibrinogen cross-linking to other platelets |
|
|
|
This is a monoclonal antibody to GIIb/IIIa that inhibits fibrinogen binding and crosslinking between platelets
|
Abciximab
|
|
|
|
What is the deficiency in Glanzmann's thrombasthenia?
|
GpIb/IIIa deficiency
**↓ Aggregation** |
|
|
|
What is the deficiency in Bernard-Soulier Syndrome that impairs platelet adhesion?
|
GpIb deficiency
**Platelets can't bind to vWF on damaged endothelial surface** |
|
|
|
How does Asprin inhibit thrombus formation
|
Asprin irreversibly inhibits COX
↓ ↓ Thromboxane A2 **↓ Aggregation) |
|
|
|
What is Thromboxane A2's job in platelet aggregation?
|
↓ blood flow , allows more platelets to bind
|
|
|
|
How do prostaglandins (PG I2) and NO stop platelet aggregation?
|
Increase bloodflow through the area
|
|
|
|
What do you call RBCs with nuclear remnants?
|
Howell Jolly Bodies
|
|
|
|
What is the job of Proteins C + S regarding anti-coagulation?
|
Cleave factors Va and VIIIa
(In Factor V Leiden, factor V is resistant to cleaving) |
|
|
|
Thalassemia:
4 α-gene mutations |
Hb Barts (γ4) --> hydrops fetalis
|
|
|
|
Thalassemia:
3 α-gene mutations |
HbH disease (β4)
|
|
|
|
-Marrow expansion --> "crewcut" on XR
-Chipmunk facies -Mediterranean descent - See ↑ HBF (α2γ2) |
β-thalassemia major
|
|
|
|
Lead poisoning inhibits what two enzymes?
|
δ-ALA-dehydratase
ferrochelatase |
|
|
|
Burton's Lines on Gingiva + Epiphyses of long bones
-RBC basophilic stippling -Abdominal Colic -Wrist/foot drop |
Lead Poisoning
|
|
|
|
Sideroblastic anemia is a hereditary defect in which enzyme needed for Heme Synthesis?
**ringed sideroblasts**--> Fe++ in mitochondria -Can also be caused by alcohol + lead |
δ-ALA synthase
|
|
|
|
In megaloblastic anemia caused by folate deficiency, what are the levels of homocysteine and methylmalonic acid like?
|
↑ homocysteine
normal methylmalonic acid |
|
|
|
In megaloblastic anemia caused by Vit. B12 deficiency, what are the levels of homocysteine and methylmalonic acid like?
|
↑ homocysteine
↑ methylmalonic acid |
|
|
|
Which tapeworm can cause megaloblastic anemia?
|
Diphyllobothrium latum
|
|
|
|
What type of anemia occurs in patients on chemotherapy (5-FU, AZT, Hydroxyurea)?
|
Nonmegaloblastic Macrocytic Anemia
|
|
|
|
In a patient using Heparin, you monitor the ____
|
PTT
|
|
|
|
In a patient using warfarin, you monitor the _____
|
PT/INR
|
|
|
|
Anemia of chronic disease is innitiated when long-standing inflammation causes the liver to release _______
|
hepcidin
(binds to ferroportin on intestinal cells and inhibits iron transport, decreases iron relased from MΦ |
|
|
|
What are the lab findings for total iron, TIBC and ferritin in Anemia of Chronic Dz?
|
↓ Iron
↓ TIBC ↑ Ferritin |
|
|
|
What will bone marrow look like in a patient with aplastic anemia?
|
Hypocellular bone marrow with fatty infiltration (full of adipocytes)
|
|
|
|
What is aplastic anemia?
|
**Failure or destruction of myeloid stem cells**
1) Radiation and drugs 2) Viral (parvo B19, EBV, HIV, HCV) 3) Fanconi's Anemia (DNA repair defect) 4) Idiopathic (may follow hepatitis) |
|
|
|
(+) osmotic fragility test
|
Hereditary Spherocytosis
|
|
|
|
↓ Ankyrin, Spectrin, band 3, protein 4.2
|
Hereditary Spherocytosis
|
|
|
|
What does the MCHC and RDW look like in Hereditary Spherocytosis?
|
↑ MCHC (measures [Hb] in RBCs)
↑ RDW (measures variation in RBC size) --------------------------------------- With MCHC, larger cells (Macrocytic) still have the same concentration of hemoglobin as normal cells, but their increased size decreases the MCHC |
|
|
|
Where do you see Heinz bodies + Bite Cells
|
G6PD deficiency
-back pain, with hemoglobinuria a few days later |
|
|
|
Hemolytic anemia of the newborn
- ↓ ATP production due to an enzyme deficiency --> rigid RBCs |
Pyruvate Kinase Deficiency/Defect
|
|
|
|
What is the mutation seen in patients with Hemoglobin C?
**See HbC Crystals in RBCs** |
Glu --> Lys
(at position 6) |
|
|
|
What is the mutation seen in in patients with Sickle Cell Anemia?
|
Glu --> Val
|
|
|
|
What test can you use to cause RBC sickling to diagnose sickle cell anemia?
|
Metabisulfide test
(causes any cell with HbS to sickle) |
|
|
|
In a patient with Sickle Cell Anemia, HbS _____ when deoxygenated and the cell forms a sickled shape
|
polymerizes when deoxygenated
|
|
|
|
Reticulocyte Count is often falsely elevated in anemia.
How do you correct reticulocyte count? |
(Ret. count )x (Hct/45)
If corrected count > 3%, marrow has a good response --> peripheral RBC destruction Corrected count < 3% = poor bone marrow response --> bone marrow destruction (underproduction) |
|
|
|
(+) Ham's Test
↓ CD 55 ↓ CD 59 |
Paroxysmal Nocturnal Hemoglobinuria
↑ complement-mediated lysis of RBCs d/t: -impaired synthesis of GPI and ↓DAF |
|
|
|
Which virus can cause aplastic crisis in a patient with Sickle Cell?
(Seen in spherocytosis too) |
Parvo B19
(ss DNA) |
|
|
|
Heterozygotes with Sickle Cell Trait have resistance to _____
|
Malaria
|
|
|
|
Why does Paroxysmal Nocturnal Hemoglobinuria occur at night?
|
Shallow breathing during sleep causes Resp. Acidosis which (+) complement
|
|
|
|
(+) Direct Coombs Test
Diagnosis? |
Autoimmune Hemolytic Anemia
(IgG or IgM coating the cells) |
|
|
|
What drug can trigger warm agglutinins and thus, hemolytic anemia?
|
α-methyldopa
|
|
|
|
-What does a Direct Coombs Test look for?
|
Agglutination occurs if patient's RBCs are coated with Ig
|
|
|
|
What does an Indirect Coomb's Test look for?
|
agglutination if patient's serum has anti-RBC surface Ig
( + in Erythroblastosis Fetalis) |
|
|
|
Schistocytes confirm ____ destruction of RBCs
|
mechanical destruction
(DIC, HUS, Malignant HTN, Prothetic Valves) |
|
|
|
How does pregnancy affect transferrin, and TIBC
|
↑ Transferrin
↓ TIBC -Normal Ferritin + Serum Fe++ |
|
|
|
anti-GpIIb/IIIa antibodies
anti-platelet antibodies |
Idiopathic Thrombocytic Purpura
Tx: Splenectomy (kills site of Ab production) |
|
|
|
What are some common things you see in platelet abnormalities?
|
Mucous membrane bleeding, epitaxis, petechiae, purpura
**↑ Bleeding Time** |
|
|
|
This platelet disorder results from defiency of the ADAMS13 enzyme.
ADAMS13 cleaves vWF multimers into smaller monomers for degredation -Larger vWF multimers result in abnormal platelet adhesion and microthrombi ↑ Megakaryocytes in marrow biospy |
Thrombotic Thrombocytopenic Purpura
-normal PT+ PTT **↑ Bleeding time*** |
|
|
|
ADAMS13 (vWF metalloprotease) deficiency
|
Thrombotic Thrombocytopenic Purpura
**See schistocytes on blood smear!!** |
|
|
|
Tx: for von Willebrand's Disease?
|
Desmopressin
↑ vWF release |
|
|
|
What is the most common inherited bleeding disorder?
|
von Willebrand Disease
Decreased vWF |
|
|
|
What do Bleeding time, PT and PTT look like in von Willebrand's Disease?
|
↑ Bleeding time
Normal PT ↑ PTT (↑ PTT = vWF stabilizes factor VIII) |
|
|
|
Abnormal ristocetin test
|
von Willebrand's Disease
|
|
|
|
What is the best screening test for DIC?
|
↑ D-dimer
(derived from splitting cross-linked fibrin) |
|
|
|
Anti-platelet 4 antibodies
|
Heparin-induced thrombocytopenia
(destroyed platelet fragments may activate and cause a thrombus) |
|
|
|
What will PT, PTT and Bleeding time look like in a patient with Disseminated Intravascular Coagulation (DIC)
|
↑ PT
↑ PTT ↑ Bleeding time (low platelet count) |
|
|
|
What happens in Protein C + S deficiency?
|
No inactivation of factors V and VIII, continuous clot formation
|
|
|
|
What might you see after a rattlesnake bite?
|
DIC
(venom activates coagulation) |
|
|
|
(+) Reed Sternberg Cells
-Localized nodal involvement |
Hodgkin's Lymphoma
|
|
|
|
What is the most common form of Hodgkin's Lymphoma?
|
Nodular Sclerosing type
|
|
|
|
(+) CD 34
Marker for which type of cells? |
Hematopoeitic Stem Cells
|
|
|
|
Neutrophilic Left Shift is characterized by what CD marker?
|
↓ CD-16 (↓Fc receptors)
------------------------------------------- During an infection, you are pumping out PMNs to deal with it... Some of them are immature, so they will have ↓CD-16 |
|
|
|
What can you give to a neutropenic patient to boost PMN production
|
GMCSF +GCSF
(colony stimulating factors) |
|
|
|
Hodgkin Lymphoma Vs. Non-Hodgkin:
See eosinophilia due to ↑ IL-5 |
Hodgkin Lymphoma
|
|
|
|
Which bacteria produces lymphocytosis-promoting factor which blocks circulating lymphocytes from leaving blood?
|
Bordetella pertussis
(WBCs can't get into Lymph nodes) |
|
|
|
(+) Monospot test
|
EBV
|
|
|
|
(-) Monospot test
|
CMV
|
|
|
|
What is the most common cause of inherited hypercoagulability?
|
Factor V Leiden
(mutated factor V can't be degraded by protein C) |
|
|
|
Reed-Sternberg cells are (+) for CD__ and CD__
|
CD15
CD30 |
|
|
|
Pt. presents with a solitary enlarging cervical lymph node.
Biopsy shows: -lymph node is divided by sclerosing bands -Reed Sternberg cells are present in lacunar-lakes (Lacunar cells) |
Nodular Sclerosis
|
|
|
|
Which type of Hodkgin's Lymphoma has the ↑ number of Reed-Sternberg cells?
|
Mixed Cellularity
|
|
|
|
Which form of Hodkgin's Lymphoma occurs in males under 35?
|
Lymphocyte Predominant
(excellent prognosis, not a lot of RS cells) |
|
|
|
Non-Hodgkin's Lymphoma:
t (8;14) |
Burkitt's Lymphoma
c-myc gene |
|
|
|
Non-Hodgkin's Lymphoma:
-Most common Non-Hodgkin's Lymphoma |
Large B-cell lymphoma
|
|
|
|
Non-Hodgkin's Lymphoma:
t (11;14) |
Mantle Cell Lymphoma
-Deactivates Cyclin D1 gene |
|
|
|
Non-Hodgkin's Lymphoma:
t (14 ;18) |
Follicular Lymphoma
(+) bcl-2 (decreases apoptosis) (-) Tingible Body Macrophages |
|
|
|
"Starry Sky" appearance on microscopy
|
Burkitt Lymphoma (NHL)
|
|
|
|
What "M-spike" is seen in Waldenstom's macroglobulinemia?
|
⇈IgM
-IgM forms pentamers and creates hyperviscosity of the blood |
|
|
|
What cytokine is increased in Multiple Myeloma?
|
⇈ IL-6
**Stimulates plasma cell growth** |
|
|
|
What are calcium levels like in Multiple Myeloma?
|
Hypercalcemia
**Plasma cells (+) RANK ligand which (-) osteoblasts and (+) osteoclasts** |
|
|
|
(+) TdT
|
ALL
|
|
|
|
(+) TdT
-CD10, CD19, CD20 |
B-ALL
|
|
|
|
-Neoplastic proliferation of naive B cells
**Smudge Cells** -Warm Ab Hemolytic Anemia - (+) CD5, CD20 |
CLL
------------------------------- CD5 normally present on T cells!!! |
|
|
|
(+) TRAP
-Bone marrow fibrosis -B-cells are trapped in red pulp of spleen |
Hairy Cell Leukemia
|
|
|
|
Neoplastic Proliferation of CD4 T cells
-Infiltrate the skin and cause rash, plaques and nodules -Aggregates in epidermis are called Pautrier Microabcesses** -Can spread to blood, causes **Sezary Syndrome** --> lymphocytes with cerebreform nuclei (look like brain) |
Mycosis Fungioides
|
|
|
|
Acute Leukemia that is PAS (+)
|
ALL
|
|
|
|
-Auer Rods --> (+) Myeloperoxidase Stain
-CD13/33 PAS (-) |
AML
|
|
|
|
M3 AML subtype responds to ____
|
All-trans-retinoic acid (Vit. A)
-causes differentiation of myeloblasts |
|
|
|
Treatment of M3 AML may cause ____
|
DIC
|
|
|
|
Tranlocation for M3 subtype of AML?
|
t (15;17)
RAR (retinoic acid receptor) |
|
|
|
t (9 ; 22)
(-) Leukocyte Alkaline Phosphatase (LAP) |
CML
-Philadelphia Chromosome (incudces BCR-ABL fusion protein with increased tyrosine kinase activity) |
|
|
|
What drug is used to treat CML?
|
Imatinib
|
|
|
|
Peroxidase (+) inclusions seen in granulocytes and myeloblasts
|
Auer Rods (AML)
(Particularly AML M3) |
|
|
|
-Cells functionally immature and do not stimulate T-cells
(+) S-100 (+) CD1a **Birbeck Granules** |
Langerhans Histiocytosis
|
|
|
|
Tx: for Heparin over-dose?
|
Protamine Sulfate
|
|
|
|
MOA of Heparin?
|
Cofactor for activation of Antithrombin
|
|
|
|
MOA of LMWH (enoxaparin)?
|
inhibits factor Xa
|
|
|
|
MOA of Lepirudin, Bivalirudin?
|
Inhibit thrombin
(Leech Saliva derivatives) |
|
|
|
Warfarin MOA?
|
Interferes with synthesis and γ-carboxylation of Vit. K dependent factors
(1972 + C&S) |
|
|
|
What is the antidote for a thrombolytic overdose?
|
Aminocaproic Acid
|
|
|
|
Thrombolytics are contraindicated in patients with _____
|
an active bleed
(think brain aneurysm) |
|
|
|
MOA: thrombolytics ?
|
Aid in concersion of plasminogen to plasmin --> cleaves thrombin and fibrin
|
|
|
|
This anticancer drug causes myelosuppression that is reversible by leucovorin
|
MTX
(leucovorin is a folinic acid analog) |
|
|
|
This anticancer drug causes myelosuppression that is NOTreversible by leucovorin
Must use **thymidine** instead |
5-FU
|
|
|
|
How does the body metabolize 6-mecaptopurine (6-MP)?
|
Xanthine Oxidase
**AVOID ALLOPURINOL** |
|
|
|
Name the cancer drug:
-Forms a complex between topoisomerase II and DNA |
Etoposide
|
|
|
|
Name the cancer drug:
-Alkylates DNA Toxicity = pulmonary fibrosis |
Busulfan
|
|
|
|
Name the cancer drug:
-Fragments DNA Toxicity = Pulmonary Fibrosis |
Bleomycin
|
|
|
|
Name the cancer drug:
-Blocks purine synthesis -metabolized by xanthine oxidase |
6-MP
|
|
|
|
Name the cancer drug:
-Cross-links DNA Toxicities: Nephrotoxic/Ototoxic |
Cisplatin
|
|
|
|
Name the cancer drug:
-Nitrogen mustard, alkylates DNA |
Cyclophosphamide
|
|
|
|
Name the cancer drug:
-Folic acid analog that inhibits dihydrofolate reductase |
MTX
|
|
|
|
Name the cancer drug:
-Prevents tubulin disassembly |
Paclitaxel/Taxols
|
|
|
|
Name the cancer drug:
-Intercalates DNA, creates free radicals Toxicity: cardiotoxic*** |
Doxorubicin
Daunorubicin |
|
|
|
Name the cancer drug:
DNA alkylating agents used in brain cancer |
Nitrosoureas
(cross CNS) |
|
|
|
Name the cancer drug:
-prevents tubulin assembly -Toxicity: CNS, paralytic ileus |
Vincristine/ Vinblastine
|
|
|
|
Name the cancer drug:
Inhibits thymidylate synthase --> decreases nucleotide synthesis |
5-FU
(pyrimidine analog) |
|
|
|
Name the cancer drug:
SERM, blocks estrogen binding to Estrogen (+) receptors |
Tamoxifen/Raloxifen
|
|
|
|
Name the cancer drug:
-Monoclonal Ab against HER-2 (erb-2) |
Trastuzumab
|
|
|
|
Name the cancer drug:
Inhibitor of PRPP synthetase |
6-MP
|
|
|
|
What drugs are used for testicular cancer?
|
Etoposide
Bleomycin Cisplatin "Eradicate Ball Cancer" |
|
|
|
What anti-cancer drug can be applied topically for basal-cell cancers?
|
5-FU
|
|
|
|
What anticancer drug is preferred to treat childhood tumors:
-Ewing Sarcoma -Wilm's Tumor -rhabdomyosarcoma |
Dactinomycin
|
|
|
|
Name the cancer drug:
Inhibits ribonucleotide reductase |
Hydroxyurea
|
|
|
|
Name the cancer drug:
Toxicity = Hemorrhagic Cystitis |
Cyclophosphamide
(prevent with MESNA) |
|
|
|
Name the cancer drug:
-antibody against protein kinases displayed in CML |
Imitinab
|
|
|
|
What are the muscles of the rotator cuff?
What movements are they responsible for? |
Supraspinatus - ABducts
Infraspinatus - LATERALLY rotates teres minor - LAT rotation and ADducts Subscapularis = MEDIALLY rotates, ADducts |
|
|
|
What are the layers of the epidermis?
|
Stratum Corneum
Stratum Lucidum Stratum Granulosum Stratum Spinosum Stratum Basalis |
|
|
|
What landmark would you useto give a pudendal nerve block?
|
Ischial Spine
|
|
|
|
The ACL is connected to the ____ tibia
|
anterior tibia
|
|
|
|
The PCL is connected to the ___ tibia
|
posterior tibia
|
|
|
|
A patient presents with pain in the forearm and a characteristic weakness of the pincer movement of the thumb and index finger.
What nerve has been damaged? |
Ant. interosseous n.
(branch of median nerve) |
|
|
|
What is the "million dollar nerve"?
Damage here you would lose the ability to grasp things (loss of opposition of the thumb with the fingers) |
recurrent branch of median n.
------------------------------------------ innervates "OAF": Opponens Pollicis Abductor Pollicis Brevis Flexor Pollicis Brevis |
|
|
|
What forms the "roof"of the carpal tunnel?
|
flexor retinaculum
|
|
|
|
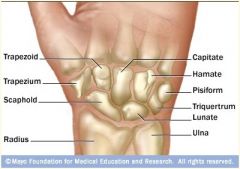
|
|
|
|
A patient fell on an outstretched hand and now experiences:
-↓ ABduction and ADduction of fingers -↓ ADduction of thumb -↓ Externsion of 4th-5th digits What bone was fractured? |
Hook of Hamate
(lesion to distal ulnar nerve) |
|
|
|
The dorsal lumbricles ___ the fingers
The palmar lumbricles ___ the finger |
Dorsal = ABduct
Palmar = ADduct **DAB** **PAD** |
|
|
|
A patient has with a knee injury:
↓ Foot INVERSION ↓ PLANTAR FLEXION ↓ Toe Flexion -Sensory deficit on sole of foot -What nerve is damaged? |
Tibial (L4-S2)
|
|
|
|
A patient presents with trauma to the lateral leg:
↓ Foot EVERSION ↓ DORSIFLEXION ↓ Toe flexion **FOOT DROP/FOOT SLAP** ↓ Sensation on anteriolateral leg and top of foot |
Common Peroneal Nerve (L4-S2)
|
|
|
|
Damage to which nerve will result in Trendelenberg Gait?
(Contralateral hip drops when standing on leg ispilateral to lesion) |
Superior Gluteal n. (L4-S1)
|
|
|
|
A patient presents saying they have trouble climbing stairs and rising from a seated position. What nerve do you suspect is damaged?
|
Inferior Gluteal n. (L5-S2)
|
|
|
|
What type of ossification occurs in long bones? (bone growth)
|
**Endochondral ossification**
-Cartilaginous model made first -O-blasts and O-clasts replace cartilage model with woven bone to lamellar bone |
|
|
|
What type of ossification occurs in flat bones? (bone growth)
-Facial bones -Skull -Pelvis -Ear bones -Ribs -Vertebrae |
**Membranous Ossification**
-Woven bone is formed directly without cartilage, later remodeled to lamellar bone |
|
|
|
Achondroplasia results in failure of longbone growth
(↓ endochrondral ossification) -There is a constitutive activation in the _____ receptor that inhibits chondrocyte proliferation. -Autosomal Dominant inheritance Associated with **advanced paternal age** |
FGR3
(fibroblast growth factor receptor) |
|
|
|
Postmenopausal/Type 1 Osteoporosis is caused by ↓ ____ levels
|
↓ Estrogen levels
Tx: -Vit D. + Calcium -Calcitonin -PULSATILE PTH -Bisphosphonates **Glucocorticoids are CONTRAINDICATED** |
|
|
|
Explain the mutation that occurs in Achondroplasia
|
**ACTIVATING MUTATION**of FGF3
***ACTIVATING*** |
|
|
|
Why are the sclera blue in a patient with Osteogenesis imperfecta?
|
↓ Sclera collagen reveals **choroidal veins**
|
|
|
|
-Failure of normal bone resorption
↓ THICK, WEAK BONE -Commonly due to loss of **Carbonic Anhydrase III** -Hearing/Vision problems fromimpinged CNs -Hydrocephalus from narrow foramen magnum -**Renal tubular acidosis** ↓ Lack of CA results in ↓ reabsorption of HCO3- |
Osteopetrosis
Tx: Marrow Transplant |
|
|
|
What causes the following sequelae of Rickets:
Pigeon Breast Deformity Frontal Bossing Rachitic Rosary Bowing of the Legs |
**Osteoid Deposition**
-Rachitic Rosary ↓ osteoid deposition at costochondral junction |
|
|
|
What will the labs for Ca++, Phosporus, PTH and Alkaline Phosphatase look like in Osteomalacia or Rickett's Disease
(low Vit. D.) |
↓ Ca++
↓ Phosphorus ↑ PTH ↑ Alkaline Phosphatase (Vit D. needed for Ca+ and P absorption in gut) |
|
|
|
What will the labs for Ca++, Phosporus, PTH and Alkaline Phosphatase look like in Osteoporosis?
|
All NORMAL****
|
|
|
|
Loss of trabecular bone mass
-Can occur with Menopause (↓ Estrogen) -Or increased age (>70) |
Osteoporosis
|
|
|
|
-Mosaic Patter of Lamellar Bone
("Puzzle Pieces" -Bone pain -Increased hat size -Hearing loss -Lion like facies Only abnormal lab is ↑ Alkaline Phosphatase |
Paget's Dz of Bone
-Imbalance b/t osteoclast and osteoblast function ----------------------------------- Osteoclasts go crazy and reabsorb tons of bone. Osteoblasts see whats going on and try to build new bone at the same time. The osteoclast tires out and you are left with osteoblasts laying down crappy bone that is THICK and SCLEROTIC |
|
|
|
What will the labs for Ca++, Phosporus, PTH and Alkaline Phosphatase look like in Paget's Dz of Bone?
|
All normal except for ↑ Alkaline Phosphatase****
|
|
|
|
"Chalk-stick fractures"
-High-output cardiac failure due to ↑ AV shunts through crappy bone |
Paget's Dz of Bone
|
|
|
|
Cystic bone spaces are filled with brown fibrous tissue
-Brown Tumors -Caused by HYPERparathyroidism ↓ Increased Bone resorption |
Osteitis fibro cystica
**HIGH PTH** |
|
|
|
A patient with longstanding HYPERparathyroidism presents with "bone pain"
-You do a bone biopsy and see Cystic bone spaces are filled with brown fibrous tissue **BROWN TUMORS** -You diagnose Osteitis fibro cystica What lab findings do you expect for Ca++, Phosphorus, PTH, and alkaline phosphatase? |
↑ Ca++
↓ Phosphorus ↑↑ PTH ↑ Alkaline Phosphatase |
|
|
|
Where does osteomyelitis occur in children?
|
metaphysis
|
|
|
|
Where does osteomyelitis occur in adults?
|
epiphysis
|
|
|
|
Where do bacteria seed in osteomyelitis in:
Children? Adults? |
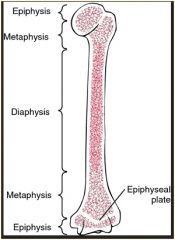
Children = METAPHYSIS
ADULTS = EPIPHYSIS |
|
|
|
What drugs would you use for a patient with Paget's Dz of Bone?
|
Calcitonin --> ↓ osteoclast activity
Bisphosphonates -->↓ osteoclast activity |
|
|
|
Which drugs can lead to increased risk of avascular necrosis?
|
Corticosteroids
|
|
|
|
Bone Tumors:
Benign tumor of bone -arises on surface of **FACIAL BONES** - a/w **GARDNER SYNDROME (FAP)** |
Osteoma
|
|
|
|
Bone Tumors:
Benign tumor of osteoblasts Arises in cortex of long bones (femur) - Bone pain that ***resolves with aspirin** - <2cm mass with radiolucent core coming off the side of the bone |
Osteoid Osteoma
|
|
|
|
Bone Tumors:
-Similar to Osteoid osteoma but is larger --> >2cm -Arises in vertebrae - Bone pain that **DOES NOT** respond to aspirin |
Osteoblastoma
|
|
|
|
Bone Tumors:
-Tumor of bone with overlying cartilage cap -Arises as a lateral projection of the **growth plate** (metaphysis) -Bone is continuous within marrow space |
Osteochondroma
**M/C benign bone tumor** |
|
|
|
Bone Tumors:
-Malignat proliferation of osteoblasts **Risk Factors** Familial retinoblastoma Paget Dz Radiation exposure -Arises in **METAPHYSIS** - Destructive "Sunburst pattern" and Codman's Triangle (lifting of periosteum) |
Osteosarcoma
|
|
|
|
Bone Tumors:
Bone biopsy reveals pleomorphic cells that produce osteoid |
Osteosarcoma
|
|
|
|
Most common bone tumor in children?
|
Osteosarcoma
|
|
|
|
Bone Tumors:
-Composed of mutli-nucleated giant cells -Young adults - Grows in **epiphysis of long bones** -"Soap bubble" on X-ray |
Giant Cell Bone Tumor
|
|
|
|
Bone tumors:
The malignant cells in Ewing Sarcoma are derived from ___ |
Neuroectoderm
|
|
|
|
Bone Tumors:
-Arises in DIAPHYSIS of long bones -"Onion Skin" appearance on Xray -Biopsy reveals **small, blue cells resembling lymphocytes** -t (22; 11) |
Ewing Sarcoma
|
|
|
|
Bone tumors:
-What does bone biopsy show in a Ewing Sarcoma? |
**small, blue cells resembling lymphocytes**
|
|
|
|
Chondromas = benign tumor of cartilage.
-They usually occur in the ____ and ___ (What bones) |
Medulla of Hands and Feet
|
|
|
|
Chondrosarcoma =malignant
-Ususally occurs in the ___ or ____ |
Medulla of pelvis and central skeleton
|
|
|
|
Hallmark of this joint disease is synovitis leading to formation of pannus tissue
-Pannus = inflammed granulation tissue |
Rheumatoid Arthritis
|
|
|
|
Osteophyte formation in DIP and PIP
|
Osteoarthritis
DIP = Herbeden Node PIP = Bourchard's Node |
|
|
|
Joints:
Ig M antibody against the Fc portion of IgG |
Rheumatoid Arthritis
**rheumatoid factor** |
|
|
|
Which finger joint does Rheumatoid Arthritis spare?
|
DIP
**HY** |
|
|
|
Arthritis and morning stiffness that lasts for more than 30 minutes and improves with use
|
Rheumatoid Arthritis
|
|
|
|
Explain the swan-neck deformity seen in Rheumatoid Arthritis
|
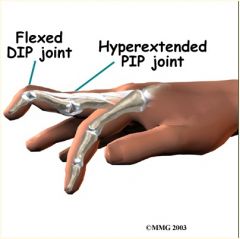
|
|
|
|
Describe the Boutonniere deformity seen in Rheumatoid Arthritis
|
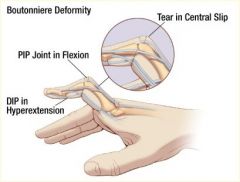
|
|
|
|
-Joint pain/stiffness with psoriasis
"sausage" fingers or toes - "pencil in cup" deformity on X-ray (+) HLA B27 |
Psoriatic Arthritis
|
|
|
|
Aortic regurgitation (Aortitis)
(+) HLA-B27 |
Ankylosing
-Bamboo spine -Sacroilitis |
|
|
|
(+) HLA-B27
-Conjunctivitis -Urethritis -Arthritis |
Reactive Arthritis
(Reiter's Syndrome) -"Can't see, can't pee, can't climb a tree" - Post GI or chlamydial infections |
|
|
|
Why does SLE cause false (+) syphilis tests (RPR/VDRL)?
|
Anti-phospholipid antibodies cross-react with cardiolipin used in tests
|
|
|
|
Epithelial granulomas containing Schaumann and asteroid bodies
|
Sarcoidosis
|
|
|
|
-Bilateral hilar lymphadenopathy
-erythema nodosum -Elevated ACE levels** -Elevated 1-alpha-hydroxylase --> INCREASED VIT. D activation in epithelial macrophages |
Sarcoidosis
-Most common in black women |
|
|
|
-Bilateral hilar lymphadenopathy
-Non-caseating granulomas in lungs *** |
Sarcoidosis
|
|
|
|
-Skeletal Muscle Dz:
-Involves skin + skeletal muscle -Bilateral PROXIMAL muscle weakness -Often associated with carcinoma - "Malar rash" or "Heliotrope Rash" (under eyes) -Grotton papules (red) on elbows, fingers and knees **Perifasicular atrophy** |
**Dermatomyocitis**
(+) Anti-Jo 1 antibodies (+) ANA |
|
|
|
(+) Anti-Jo 1 antibodies
(+) ANA |
Dermatomyositis
Polymoyositis |
|
|
|
-Inflammatory disorder of skeletal muscle
-resembles Dermatomyositis -**Endomysial inflammation** seen on muscle biopsy |
Polymyositis
(+) Anti-Jo 1 antibodies (+) ANA |
|
|
|
A keloid scar is characterized by excess type ___ collagen
|
type III
|
|
|
|
Auto-antibodies to pre-synaptic Ca++ channels which decrease ACh release
|
Lambert Eaton
-Seen with small cell CA in lung*** |
|
|
|
Increased Stratum spinosum
Decreased Stratum Granulosum (+) Auspitz sign |
Psoriasis
|
|
|
|
Hyperpigmentation of face associated with pregnancy
|
Melasma
|
|
|
|
What layer of epidermis does S. aureus exotoxin destroy keratinocyte attachments in during Scalded Skin Syndrome
|
Stratum Granulosum
-Generalized erythematous rash with sloughing of upper layers of the epidermis |
|
|
|
Deposits of IgA at tips of dermal papillae
-pruritic papules and vesicles -Seen in **Celiac Dz** |
Dermatitis Herpetiformis
|
|
|
|
Wickham Striae seen in oral mucosa
-biopsy reveals "Sawtooth" inflammation at the dermal/epidermal junction |
Lichen Planus
-associated with Hep C |
|
|
|
Pruritic, Purple, Polygonal Papules
-"Sawtooth" infiltrate of lymphocytes at dermal/epidermal junction -Associated with Hepatitis C |
Lichen Planus
|
|
|
|
Inflammatory lesions of subQ fat.
-usually on anterior shins |
**Erythema nodosum**
Associated |
|
|
|
Patient develops a "Herald Patch"
-followed days later by "Christmas Tree" distribution rash |
pityriasis rosea
|
|
|
|
What is the most common skin cancer overall?
|
Basal Cell CA
-rolled edges -Central ulceration -"Pearly papules" |
|
|
|
Patient presents with a lesion on the nose:
-rolled edges -Central ulceration -"Pearly papules" -Biopsy shows **palisading nuclei** |
Basal Cell CA
(almost never metastasizes) |
|
|
|
Very common skin cancer associated wtih exposure to sunlight and arsenic.
|
Squamous cell CA
|
|
|
|
Patient who works outside as a landscaper presents with an ulcerative red lesion on his face.
Biopsy show **keratin pearls** |
Squamous cell CA
|
|
|
|
A dysplastic nevus is a precursor to _____
|
Melanoma
-Asymmetry -Borders (irregular) -Color Variation -Diameter (>6mm) |
|
|
|
Tumor marker for Malignant Melanoma?
|
S-100
|
|
|
|
____ is a precursor to squamous cell CA in skin
|
Acatinic keratosis
|
|
|
|
Corticosteroids block _____ and prevent Membrane lipids (phosphatidylinosinotol) from converting to Arachidonic acid
|
Phospholipase A2
|
|
|
|
Arachidonic Acid is converted to Hydroperoxides ---> Leukotrienes by _________
|
Lipoxygenase
|
|
|
|
Prostacyclins (PG12) vs. Prostaglandins (PGE2)
↓ Platelet aggregation ↓ Vascular tone ↓ Bronchial tone ↓ Uterine Tone |
Prostacyclins (PGI2)
|
|
|
|
Prostacyclins (PG12) vs. Prostaglandins (PGE2)
↑ Uterine tone (contraction) ↓ Bronchial tone ↓ Vascular tone |
Prostaglandins (PGE2)/(PGF2)
|
|
|
|
How does Thromboxane A2 affect:
-Platelet aggregation -Vascular tone -Bronchial tone |
↑ Platelet aggregation
↑ Vascular tone ↑ Bronchial tone |
|
|
|
What is the main action of LTB4 (leukotriene)?
|
PMN Chemotaxis
|
|
|
|
What effect do leukotrienes have on bronchial tone?
|
↑ Bronchial tone
|
|
|
|
Prostacyclins Vs. Prostaglandins
-Which ↑ uterine tone? |
Prostaglandins ↑ Uterine Tone
|
|
|
|
Prostacyclins Vs. Prostaglandins
-Which ↓ uterine tone? |
Prostacyclins ↓ uterine tone
|
|
|
|
This drug blocks Lipoxygenase from forming Leukotrienes
|
Zileutron
|
|
|
|
These drugs block leukotriene receptors
|
Zafirlukast
Montelukast |
|
|
|
These drugs are good to use in patients with RA or osteoarthritis that also have a gastric ulcer
|
COX-2 inhibitors = Celecoxib
-NO GASTRIC SIDE EFFECTS |
|
|
|
This OTC drug has antipyretic and analgesic properties, but LACKS anti-inflammatory properties.
Reversibly inhibits COX in CNS |
Acetaminophen
|
|
|
|
This drug inhibits uric acid resorption in the in the PCT
Useful in gout |
Probenecid
|
|
|
|
These two drugs inhibit xanthine oxidase and can be used for gout.
|
Allopurinol
Febuxostat |
|
|
|
Why can't a person taking Allopurinol also use Azithioprine or 6-mecaptapurine?
|
They are metabolized by xanthine oxidase and can build to toxic levels
|
|
|
|
This drug is used for acute gout and stabilizes tubulin to inhibit polymerization and impair leukocyte chemotaxis and degranulation.
|
Colchicine
|
|
|
|
An elderly patient presents with a raised discolored plaque on his right arm.
It appears **waxy** and "stuck on" -Biopsy shows **keratin pseudocysts** |
Seborrheic Keratosis
|
|
|
|
The "Leser-Trelat" sign is the sudden onset of multicle seborrheic keratoses and suggests underlying ___ carcinoma
|
GI tract
|
|
|
|
What causes the pigmentation seen in freckles?
-Small tan to brown maculae with darkness that increases with exposure to sunlight. |
**melanosomes***
(NOT MELANOCYTES!!) |
|
|
|
Which form of UV light causes DNA damage?
|
UV-B
|
|
|
|
Vitiligo is the loss of skin pigmentation. It is due to the autoimmune destruction of _____
|
melanocytes
|
|
|
|
Patient presents with firm, pink umbilicated papules.
-Associated with poxvirus |
Molluscum contagiosum
-See **molluscum bodies** in keratinocytes |
|
|
|
This nerve controls:
-Biceps -Brachialis **Felxion at the elbow** |
Musculocutaneous n.
|
|
|
|
This nerve controls:
-Brachioradialis -Extensors of wrist and fingers -**SUPINATORS** -Triceps **Extensors + Supinators** |
Radial N.
|
|
|
|
This nerve controls pronation of the forearm
|
Median n.
|
|
|
|
During muscle contraction, what receptor opens the sarcoplasmic reticulum?
|
ryanodine receptor
(coupled with Dihydropyridine receptor and activated by depolarization coming down T-tubule) |
|
|
|
During muscle contracytion, Ca++ binds to troponin C causing a conformational change.
This allows _____ to mov eout of the way to allow actin/myosin cycling |
tropomyosin
|
|
|
|
Describe the venous drainage of the LEFT ovary/testicle
|
Left ovary/testicle→left gonadal v. → left renal vein → IVC
|
|
|
|
Describe the venous drainage of the RIGHT ovary/testicle
|
Right ovary/testicle → Right gonadal vein → IVC
|
|
|
|
Varicoceles most commonly occur in the (left/right) testicle
|
left testicle
-------------------------------- The left spermatic vein hits the left renal vein at a 90 degree angle Flow is more backed up on the left Left testicle also hangs lower due to this reason |
|
|
|
What lymph nodes do the ovaries/testicles drain to?
|
PARA-AORTIC
|
|
|
|
Which ligament holds the Ovarian vessels?
|
Suspensory Ligament of the Ovaries
(Connects ovaries to lateral pelvic wall) |
|
|
|
Which ligament holds the uterine vessels?
|
Cardinal Ligament
(Connects cervix to side-wall) |
|
|
|
Which uterine ligament is a derivative of of the gubernachulum?
|
Round ligament of uterus
(connects uterine fundus to labia majora and runs through the inguinal canal by passing through deep ring) |
|
|
|
What is the histology of the endocervix?
------------------**transition zone** What is the histology of the ectocervix? |
Endocervix = simple columnar
Ectocervix = stratified squamous |
|
|
|
Which male reproductive cells:
-Secrete inhibin → inhibits FSH -Secrete Androgen Binding Protein → Maintains testosterone levels -Form blood-testis barrier via tight junctions -Produce anti-mullerian hormone |
Sertoli Cells
-grow and nourish sperm |
|
|
|
Male reproductive cells:
-stimulated by FSH |
Sertoli
|
|
|
|
Male reproductive cells:
Stimulated by LH |
Leydig cells
(+) Testosterone |
|
|
|
Female Reproductive:
-The ___ cell is stimulated by LH -It has 17α-hydroxylase which converts cholesterol into Andostenedione |
Theca Cell
**no Aromatase --> can't convert Andostenedione to Estrogen** |
|
|
|
Female Reproductive:
-The _____ cell is stimulated by FSH - It converts Andostenedione to Estrogen via Aromatase |
Granulosa Cell
**no 17α-hydroxylase *** |
|
|
|
Estrogen receptros are expressedin the ____ of a cell
|
cytoplasm
Move to nucleus when bound by a ligand |
|
|
|
Which layers of the endumetrium are shed during menstruation?
|
-Stratum compactum
-Stratum spongiosum ------------------------------------------- Endometrial layers from top to bottom: -Stratum compactum -Stratum spongiosum -Stratum basalis (not shed) |
|
|
|
Which hypothalamic nucleus is involved with ovulation?
|
Arcuate Nucleus
|
|
|
|
Which female sex hormone:
-stimulates endometrial glandular secretions and spiral artery development -produces thick cervical mucous -Inhibits LH +FSH - ↓ estrogen receptor expressivity |
**Progesterone**
-Produced by the CORPUS luteum for about 14 days (luteal phase) -Will die if no fertilization occurs -beta-hCG from placenta will maintain the corpus luteum for 6 weeks until the placenta can take over progesterone production |
|
|
|
This female sex hormone:
↓ myometrial excitability (+) uterine smooth muscle relaxation ↑ Body Temperature |
Progesterone
|
|
|
|
GnRH is synthesized and released by the _____ of the hypothalamus
|
Arcuate Nucleus
|
|
|
|
The luteal phase of menstruation is about ____ days
|
14 days
(lifespan of corpus luteum) |
|
|
|
When do fetal oocytes complete meiosis I ?
|
After ovulation --> secondary oocytes
------------------------------------------- Then, they are stuck in Meiosis II Metaphase unless fertilization occurs |
|
|
|
Primary fetal oocytes are arrested in _____ of Meosis I
|
Prophase of Meiosis I
|
|
|
|
Where does fertilization normally take place?
|
Ampulla of Fallopian Tube
|
|
|
|
When does implantation occur?
|
~ day 6
|
|
|
|
After implantation, what cells produce βhCG?
|
Syncytiotrophoblasts of placenta
|
|
|
|
A decrease in _____ after delivery helps to induce lactation
|
Progesterone
|
|
|
|
What is partly responsible for decreased fertility in a breast-feeding mother?
|
**Prolactin**
-maintains lactation - 95% contraceptive action |
|
|
|
What are the hormonal levels of estrogen, FSH, LH and GnRH like durinf Menopause?
|
↓ Estrogen
⇈ FSH ↑ LH (no surge d/t low estrogen) ↑ GnRH |
|
|
|
Testicular Atrophy
Euchnoid Body Shape Tall, long extremities Gynecomastia, female hair distribution |
Klinefelters
(47 XXY) **Presence of inactivated C "Barr Body"** |
|
|
|
Do patients with Turner Syndrome have a Barr-body?
|
No
|
|
|
|
If a patient presents with pre-eclampsia before 20 weeks of pregnancy, what should you rule out?
|
Molar Pregnancy
|
|
|
|
↑ βhCG
"Honey-combing" of uterus with "cluster of grapes" appearance -Abnormal uterine size |
Hydatidiform Mole
|
|
|
|
-Autosomal recessive
-Inability to convert testosterone to DHT -Ambiguous genitalia until puberty when ↑ testosterone causes maculinization and growth of external genitalia |
5α-reductase deficiency
|
|
|
|
-Defective development of GnRH cells and olfactory placode
- ↓ synthesis of GnRH in hypothalamus -Anosmia - lack of secondary sexual characteristics |
Kallman Syndrome
|
|
|
|
This type of hydatidiform mole is 100% paternal origin
|
Complete
(2 sperm + empty egg) |
|
|
|
A young female presents with two bilateral bumps in her labia majora
-You notice no pubic hair development -Labs show ↑ testosterone, ↑ estrogen, ↑ LH |
Androgen Insensitivity Syndrome
**defect in androgen receptor** - female external genitalia with rudimentary vagina -no uterus or fallopian tubes |
|
|
|
Complete hydatidiform moles run the chance of developing into what malignancy?
|
Choriocarcinoma
|
|
|
|
What is the DOC for eclampsia?
|
IV Magnesium Sulfate
+ Diazepam for seizures |
|
|
|
Over 20 week mark in pregnancy
-HTN + proteinuria + Edema |
Pre-eclampsia
|
|
|
|
Over 20 week mark in pregnancy
HTN + proteinuria + Edema + Seizures |
Eclampsia
|
|
|
|
What causes the symptoms seen in Pre-eclampsia and Eclampsia?
|
-Placental ischemia
- due to impaired vasodilation of spiral arteries resulting in ↑ vascular tone |
|
|
|
Use of what drug is linked with Abruptio placentae?
|
cocaine
|
|
|
|
-Premature detachment of placenta from attachment site
-PAINFUL bleeding in 3rd trimester |
Abruptio placentae
|
|
|
|
-Defective decidua basalis due to prior C-section or placenta previa
-Placenta attaches to myometrium -***Massive bleeding after delivery** |
Placenta accreta
|
|
|
|
-Attachment of placenta to lower uterine segment
**May occlude os** -Painless bleeding during any trimester of pregnancy -History of multiparity or C-section |
Placenta previa
**Deliver with C-section** |
|
|
|
-Fetal vessels crossing or running in close proximity to the inner cervical os.
These vessels course within the membranes (unsupported by the umbilical cord or placental tissue) and are at risk of rupture when the supporting membranes rupture |
Vasa previa
|
|
|
|
A 17 year old female presents with severe abdominal pain.
She has a (+) βhCG and endometrial biopsy shows **decidualized endometrium with NO chorionic villi** |
Ectopic Pregnancy
Tx: MTX |
|
|
|
endometrial biopsy shows **decidualized endometrium with NO chorionic villi**
|
Ectopic Pregnancy
|
|
|
|
Name 2 causes of polyhydramnios
|
1) Esophageal/Duodenal Atresia
2) Anencephaly (Also maternal diabetes) |
|
|
|
What is a common cause of oligohydramnios in a Mother with a male fetus?
|
posterior urethral valves
|
|
|
|
HPV 16 --> E6 gene inhibits ___
|
p53 suppressor gene
|
|
|
|
HPV 18 --> E7 gene inhibits ____
|
Retinoblastoma suppressor gene
|
|
|
|
What is the #1 risk factor for cervical cancer?
|
Multiple Sexual Partners
(increase risk of HPV) |
|
|
|
Cervical biopsy shows koilocytes with "raisinoid" nuclei and peri-nuclear hallows
|
HPV --> cervical CA
|
|
|
|
-Endometrial gland/stroma outside of normal location
-presents as pain during menstruation -Most commonly affects ovaries and leads to **Chocolate cysts** - May present as: **pelvic pain (uterine ligaments)** **Pain on defecation (Pouch of Douglas)** **Painful intercourse** |
Endometriosis
-Uterus is NORMAL size |
|
|
|
-Endometrial glands implanted within myoetrium of the uterus
-Menorrhagia, dysmenorrhea, pelvic pain -Uterus is ENLARGED |
Adenomyosis
-Uterus is ENLARGED (basically, it's endometriosis of the uterus) |
|
|
|
-Postmenopausal vaginal bleeding
-Results from excess estrogen stimulation throughout lifetime -Abnormal endometrial gland proliferation |
Endometrial Hyperplasia
|
|
|
|
What is the most likely cause of Endometriosis?
|
Retrograde menstruation with ectopic implantation on other tissues
|
|
|
|
Risk factors for endometrial hyperplasia?
|
↑ Estrogen Exposure
-nullparity -early menarche -late menopause -granulosa cell tumor -PCOS -Hormone replacement therapy |
|
|
|
What is the most common gynecologic malignancy?
|
Endometrial CA
|
|
|
|
What is the most common tumor in women?
|
Leiomyoma
|
|
|
|
What ethnic group has ↑ incidence of Leiomyomas?
|
Blacks
|
|
|
|
-Benign smooth muscle tumor
- ↑ size with pregnancy - ↓ size after menopause -**Whorled pattern of smooth muscle bundles** |
Leiomyoma
|
|
|
|
"gun-powder" nodules found outside endometrium
|
Endometrial implants
|
|
|
|
Of all the gynecological malignancies, which has the worst prognosis?
|
Ovarian CA
|
|
|
|
-Malignant proliferation of smooth muscle arising from the myometrium
-usually seen in post menopausal women - areas of necrosis and hemorrhage |
Leiomyosarcoma
-do NOT arise from Leiomyomas!!! |
|
|
|
Risk factors for endometrial carcinoma?
|
-HTN
-Obesity -Nullparity -Diabetes - lAte menopause "HONDA" |
|
|
|
Common side effect of Clomiphene
(partial estrogen agonist that can lead to ovulation) |
Vision disturbances
|
|
|
|
What is the LH:FSH ratio seen in PCOS?
|
2:1
|
|
|
|
Why is FSH decreased in PCOS?
|
There is ↑ conversion of testosterone (from theca hyperplasia) to ESTRONE.
Estrone feedback inhibits FSH resulting in cystic degredation of the follicles |
|
|
|
What can you give to a woman with PCOS to ↓ LH and androgenesis?
|
low-dose OCP
medroxyprogesterone |
|
|
|
What can you give to a woman with PCOS to decrease acne and hirsutism?
|
Spironolactone
|
|
|
|
What is the most common ovarian mass in young women?
|
Follicular cyst
|
|
|
|
A dermoid ovarian cyst is a mature teratoma. They are filled with various types of tissue such as fat, bone, teeth cartilage and are derived from _____ tissue
|
Ectodermal tissue
|
|
|
|
Fetal tissue is present in a _____ hydatidiform mole
|
Partial Mole
|
|
|
|
How many chromosomes are present in a partial hydatidiform mole?
|
69
-Normal ovum fertilized by 2 sperm |
|
|
|
How many chromosomes are present in a complete hydatidiform mole?
|
46
|
|
|
|
Ovarian Germ Cell Tumors:
Malignant germ cell tumor that is equivalent to a male seminoma -tumor is composed of sheets of large shells with clear cytoplasm and central nuclei -**Most common malignant germ cell tumor in females** |
Dysgerminoma
***a/w Turner's Syndrome!!*** |
|
|
|
Tumor marker for Dysgerminoma?
(Ovarian germ cell tumor) |
↑ LDH ***
|
|
|
|
Ovarian Germ Cell Tumor:
-Malignant tumor of tropoblasts and synsychioblasts -mimics placental tissue -NO CHORIONIC VILLI PRESENT *** -⇈ βhCG |
Choriocarcinoma
|
|
|
|
Ovarian Germ Cell Tumor:
-Aggressive malignancy in ovaries (testes in boys) -Yellow, friable masses - Histology resembles glomeruli (**Schiller Duval Bodies**) **↑ AFP** |
Yolk Sac/Endometrial Sinus Tumor
|
|
|
|
What is the most common germ cell tumor in females?
|
Cystic Teratoma
|
|
|
|
Ovarian tumor that is composed of thyroid tissue
|
Struma Ovarii
(a teratoma) |
|
|
|
Ovarian Germ Cell Tumor:
-Malignant tumor comprised of large, primitive cells |
Embryonal Tumor
|
|
|
|
What gene mutations cause increased risk for Ovarian CA and Tumors?
|
BRCA-1
BRCA-2 HNPCC |
|
|
|
Ovarian non-germ cell tumor:
-Benign, frequently bilateral -have a **fallopian-tube** like epithelium |
Cystadenoma
|
|
|
|
Ovarian non-germ cell tumor:
-Malignant, frequently bilateral -**Psammoma bodies** seen on histology |
Serous Cystadenocarcinoma
**Psammoma Bodies** |
|
|
|
Ovarian non-germ cell tumor:
-Malignant -Can result in **Pseudomyxoma peritonei** -Intrapreitoneal accumulation of mucinous material from OVARIAN or APPENDICEALl tumors |
Mucinous Cystadenocarcinoma
|
|
|
|
Ovarian non-germ cell tumor:
-multilocular cyst lined by mucous secreting epithelium -Intestine-like tissue |
Mucinous Cystadenoma
|
|
|
|
Ovarian non-germ cell tumor:
-Benign and unilateral -**Bladder epithelium** -Solid tumor with pale yellow/tan color that appears encapsulated - ***Coffee-bean like nuclei**** |
Brenner Tumor
|
|
|
|
-Bladder epithelium in ovarian cyst
***Coffee-bean nuclei*** |
Brenner Tumor
|
|
|
|
Intraperitoneal accumulation of mucinous material from an ovarian or apendiceal tumor
|
Pseudomyxoma peritonei
|
|
|
|
Female Sex-chord stromal tumors:
-Bundles of spindle-shaped fibroblasts - "Pulling sensation" in groin **Meig's Syndrome** Triad of: 1) ovarian fibroma 2) ascites 3) hydrothorax |
Fibroma
|
|
|
|
Triad of:
-Ovarian fibroma -Ascites -Hydrothorax (pleural effusion) |
**Meig's Syndrome**
due to fibromas... Symptoms go away with removal of tumors |
|
|
|
Female Sex-chord stromal tumors:
-Secretes estrohen --> precocious puberty -Can cause endometrial hyperplasia in adults -Abnormal uterine bleeding **Call-Exner Bodies** = small follicles with eosinophilic secretions |
Granulosa-Theca Cell Tumor
|
|
|
|
GI malignancy that metastasizes to the ovaries causing:
**mucin-signet ring cells** |
Krukenberg Tumor
|
|
|
|
What is Ashermann Syndrome?
(female repro) |
Secondary ammenorrhea due to loss of basalis and scarring
-Result of overly-aggressive dilation and curettage |
|
|
|
Cancer from the lower 2/3 of the vagina spreads to the ____ nodes
|
inguinal nodes
|
|
|
|
Cancer from the upper 1/3 of the vagina metastasizes to the _____ nodes
|
Iliac nodes
|
|
|
|
Reproductive Neoplasm:
-Malignant mesenchymal proliferation of immature skeletal muscle -seen in children < 4 **Bleeding, "grape-like" mass on vagina (or penis)** - Contains spindle-shaped **Rhabdomyoblasts** with cross-striations - stain (+) for desmin and myogenin |
**Stroma botryoides**
(Embryonal rhabdomyosarcoma) (+) Desmin stain |
|
|
|
A young child presents with:
**Bleeding, "grape-like" mass on vagina (or penis)** - Biopsy stains (+) for **Desmin** |
**Stroma botryoides**
(Embryonal rhabdomyosarcoma) |
|
|
|
DES exposure in utero may lead to ______ in women
|
Clear Cell Vaginal CA
|
|
|
|
Breast tumors:
- Small, mobile firm mass with sharp edges ↑ Size and tenderness with pregnancy or menstruation Regress after pregnancy/menstruation |
Fibroadenoma
**Benign** -Bilateral - Not a precursor to breast cancer |
|
|
|
What is the most common breast tumor in women under 35 years of age?
|
Fibroadenoma
|
|
|
|
Breast tumors:
-Small tumor that grows in lactiferous ducts **Serous Bloody Nipple Discharge** - Slight increased risk for carcinoma |
Intraductal Papilloma
-Benign |
|
|
|
**Serous Bloody Nipple Discharge**
|
Intraductal Papilloma
|
|
|
|
Breast tumors:
- Common in women in their 60's -Large, bulky mass of connective tissue cysts **Leaf-like** projections |
Phyllodes Tumor
-benign --> some may become malignant |
|
|
|
Where is cancer most commonly found in the breast?
|
Upper-outer quadrant
|
|
|
|
What is the single most important prognostic factor for breast cancer?
|
Axillary Node Involvement
|
|
|
|
What are some risk factors for breast cancer?
|
↑ estrogen exposure
-early menarche, late menopause -older age at 1st live birth -obesity |
|
|
|
Breast Tumors:
-Malignant - Fills ductal lumen -Arises from ductal hyperplasia **DOES NOT cross basement membrane** |
DCIS
-Non-invasive |
|
|
|
Breast Tumors:
-Malignant -Ductal **Caseous necrosis** -Does not cross BM, it is a subtype of DCIS |
**Comedocarcinoma**
-non-invasive |
|
|
|
**Caseous necrosis** of Ductal lumen in breast
|
**Comedocarcinoma**
-subtype of DCIS, non-invasive |
|
|
|
Breast Tumors:
-Firm, fibrous "rock-hard" mass - Sharp margins and small, glandular duct-like cells **Stellate Morphology** |
Invasive Ductal Carinoma
|
|
|
|
Breast Tumors:
-Malignant -Multiple, Bilateral **Metastasis to peritoneum** **Signet-ring cells** |
Invasive Lobular CA
- **Single file** patternof growth in lobules -Lacks E-CADHERIN --> can't stick to ducts so they remain in the lobule |
|
|
|
This form of Breast CA. forms no calcifications on biopsy.
Discohesive cells **lack-e-cadherin** adhesion protein |
Lobular Carcinoma in Situ
or Invasive Lobular CA |
|
|
|
-Nipple retraction (new retraction)
-Peau d'orange (dimpling) -Neoplastic cells block lymphatic drainage (swollen breast) |
Inflammatory Breast CA
-50% survival |
|
|
|
Which breast cancer has the worst prognosis?
|
Inflammatory Breast CA
|
|
|
|
Eczematous patches on the the nipple that will not go away.
Epidermal biopsy show **large cells with clear halo** |
Paget's Disease of the breast
|
|
|
|
The BRCA-1 mutation is associated with ____ and ____
|
breast and ovarian CA
|
|
|
|
The BRCA-2 mutation is associated with ________
|
breast cancer in MALES****
|
|
|
|
Why do lobular breast carcinomas have good prognoses and are treatable?
|
They are Estrogen & Progesterone receptor (+)
|
|
|
|
Breast Tumor:
-malignant -Fleshy, cellular, lymphocytic infiltrate (lymphocytes + plasma cells) -May mimic fibroadenoma on mammogram |
Medullary Breast CA
-good prognosis |
|
|
|
What drugs have a side-effect of gynecomastia?
|
Spironolactone
Digitalis Cimetidine Alcohol Ketoconazole "Some Drugs Create Awesome Knockers" |
|
|
|
Extramammary Paget Disease can occur on the vulva.
It most be distinguished from Melanoma. How would these two stain for PAS, Keratin and S100? |
**Pagets**
(+) PAS (+) Keratin (-) S100 **Melanoma** (-) PAS (+) Keratin (+) S100 |
|
|
|
Which is associated with underlying malignancy, Paget's Disease of the breast of Paget's diseaseof the vulva?
|
Paget's Dz of Breast
|
|
|
|
During BPH, which lobes of the prostate enlarge and cause compression of the ureter leading to urinary Sx?
|
Lateral & Middle Lobes
(Periurethral) |
|
|
|
Is BPH considered pre-malignant?
|
No
|
|
|
|
↑ free prostate-specific antigen (PSA)
|
Indicator for BPH
|
|
|
|
↑ total PSA
↓ **fraction** of free PSA |
Prostate CA
|
|
|
|
Prostate CA arises from the ____ lobe
|
Posterior Lobe
|
|
|
|
Testicular Germ Cell Tumors:
-Most common testicular tumor |
Seminoma
|
|
|
|
Testicular Germ Cell Tumors:
-Most common testicular tumor -PAINLESS -Occurs in young males -Cells are in lobules and have **fried egg** |
Seminoma
|
|
|
|
Testicular Germ Cell Tumors:
-PAINFUL -glandular/papillary pathology - may be associated with ↑βhCG and ↑AFP |
Embryonal Carcinoma
|
|
|
|
Testicular Germ Cell Tumors:
-Yellow, mucinous -Resemble glomeruli (Schiller-Duval Bodies) -↑AFP |
Yolk Sac Tumor
|
|
|
|
Testicular Germ Cell Tumors:
-Malignant -↑βhCG -Disordered trophoblasts -May metastasize to LUNGS** -Gyencomastia from ↑βhCG |
Choriocarcinoma
|
|
|
|
Testicular non-Germ Cell Tumors:
-Golden brown color, produces testosterone -Precocious puberty in boys -Gynecomastia in men **Reinke Crystals** seen histologically |
Leydig-Cell Tumor
**Reinke Crystals*** Increased Testosterone |
|
|
|
What is the most common cause of prostatitis in older men?
|
E.coli (#1)
Pseudomonas |
|
|
|
What is the most common cause of prostatitis in young men?
|
N. gonorrhea
Chlamydia |
|
|
|
Which antidepressant causes priapism?
|
Trazadone
|
|
|
|
Not having a circucism puts men at risk for what cancer of the penis?
|
Squamous cell CA
|
|
|
|
Opening of urethra on the inferior surface of the penis.
-due to **failure of urethral folds to close** |
Hydrospadias
|
|
|
|
Opening of urethra on the superior surface of the penis.
Due to **abnormal positioning of genital tubercle** |
**Epispadias**
-a/w bladder extrophy (part of bladder outside of body) |
|
|
|
This drug is a GnRH analog with agonist properties when used in pulsatile fashion
-Pulsatile Use treats infertility*** -Normal use is for prostate cancer or uterine fibroids |
Leuprolide
|
|
|
|
This drug is a testosterone receptor inhibitor that is used to treat Prostate CA
|
Flutamide
|
|
|
|
How does ketoconazole inhibit steroid synthesis and act as an antiandrogen drug?
|
inhibits desmolase
|
|
|
|
What type of drugs are clomiphene, tamoxifen and raloxifene?
|
SERMs
|
|
|
|
Which SERM drug acts as anagonist in bone and may treat osteoporosis?
|
Raloxifene
|
|
|
|
Anastrozole/Exemestane inhibit what enzyme?
-Used in postmenopausal women with breast cancer |
Aromatase Inhibitors
|
|
|
|
This drug is a competitive inhibitor of progestins at the progesterone receptor.
Used in the termination of pregnancy along with Misoprostol (PGE2) |
Mifepristone
|
|
|
|
How do OCPs treat acne in women?
|
OCPs increase Estrogen
↓ Increased SHBG ↓ Decreased Testosterone --> ↓ Acne |
|
|
|
What β2 agonists are used to relax the uterus and prevent pre-mature uterine contractions?
|
Terbutaline
Ritodrine** |
|
|
|
******
This drug is an alpha blocker specific for the **α1A,D** receptor which is only found on the prostate! Decrease smooth muscle contraction to help control urinary problems **NO ORTHOSTATIC HYPOTENSION** |
Tamulosin
|
|
|
|
-These drugs may cause impaired blue-green vision
|
PDE Inhibitors
(Sildenafil) |
|
|
|
These drugs inhibit cGMP phosphodiesterasec--> ↑ smooth muscle relaxation --> ↑ blood flow to corpus cavernosum
|
Sildenafil, vardenafil
(PDE Inhibitors) |
|
|
|
What is the name of a synthetic androgen drug that acts as a partial agonist at androgen receptors?
-Used for endometriosis and hereditary angioedema |
Danazol
|
|
|
|
Learning in which a natural response (salivation) is elicited by a conditioned, or learned stimulus (bell) that was previously presented in conjunction with an unconditioned stimulus (food)
|
Classical conditioning
|
|
|
|
Learning in which a particular action is elicited because it produces a reward
|
Operant Conditioning
|
|
|
|
What are the 4 mature defense mechanisms?
|
Sublimation
Altruism Suppression Humor **SASH** |
|
|
|
What is anaclitic depression? Where is it seen
|
Severe depression in an infant.
Seen in long-term deprivation of affection |
|
|
|
Who is the most likely person to physically abuse a child?
|
Mother/Primary care-giver
|
|
|
|
Who is the most likely person to sexually abuse a child?
|
Known to victim, usually male
|
|
|
|
Neurotransmitter Changes:
Alzheimer's |
↓ ACh
|
|
|
|
Neurotransmitter Changes:
Depression |
↓Dopamine
↓Serotonin ↓NE |
|
|
|
Neurotransmitter Changes:
Huntington's Dz |
↓ GABA
↓ ACh ↑ Dopamine |
|
|
|
Neurotransmitter Changes:
Anxiety |
↑ NE
↓ GABA ↓Serotonin |
|
|
|
Neurotransmitter Changes:
Schizophrenia |
↑ Dopamine
|
|
|
|
Neurotransmitter Changes:
Mania |
↑ NE
↑ Serotonin |
|
|
|
Neurotransmitter Changes:
Parkinson's Dz |
↓ Dopamine
↑ Serotonin ↑ ACh |
|
|
|
Which portion of the brain is responsible for memory/
|
Hippocampus
|
|
|
|
What psychosocial crisis is seen in young adults (18-35)
|
Intimacy vs. Isolation
|
|
|
|
What psychosocial crisis is seen in teens (12-18)?
|
Identity vs. Role Confusion
|
|
|
|
What psychosocial crisis is seen in infants (birth-18m)
|
Trust vs. Mistrust
|
|
|
|
What are the Kubler-Ross Stages of Grief? (5)
|
Denial
Anger Bargaining Grief/Depression Acceptance **DABGA** |
|
|
|
Name the DSM_IV axes:
|
I) Psychiatric Disorders
II) Intellectual disabilities/ Personality Disorders III) General Medical Dx IV) Psychosocial (stuff at home, work etc..) V) Global Assessment Functioning |
|
|
|
What is the most common cause of CONGENITAL mental retardation?
|
Down Syndrome
|
|
|
|
What is the most common cause of mental retardation
(not congenital!) |
Fetal Alcohol Syndrome
|
|
|
|
What eating disorder features enlarged parotid glands?
|
Bulemia Nervosa
|
|
|
|
Define alcohol abuse
|
Continued alcohol use after recurrent, negative consequences
|
|
|
|
What are the stages of behavioral change? (5)
|
!) Precontemplation = +/- awareness, no thought in changing
2) Contemplation = desire to change 3) Preparation = intention to change 4) Action = begins to change 5) Maintenance = consistent change > 6 months (Stage 6 is relapse) |
|
|
|
****Delirium vs. Dementia****
"Waxing, waning level of conciousness with acute onset" Acute changes in mental status, ↓ attention span and level of arousal Disorganized thinking **Abnormal EEG** |
Delirium
-Reversible (check drugs) |
|
|
|
****Delirium vs. Dementia****
- Gadual decrease in cognition -Consciousness IS NOT affected -Memory Deficits -Aphasia -Impaired Judgment **Normal EEG** |
Dementia
-Irreversible |
|
|
|
What is a hypnagogic hallucination?
|
Hallucination while GOING to sleep
**HypnaGOgic |
|
|
|
What is a hypnopompic hallucination?
|
Hallucination when waking from sleep
|
|
|
|
_____ use is a risk factor for Schizophrenia in teens
|
Marijuana
|
|
|
|
In order to be diagnosed with Schizophrenia, a patient must have symptoms for at least ___ months
|
6 months
|
|
|
|
Schizophreniform disorder is diagnosed when a patient has symptoms for at least ___ months but less than ____ months
|
at least 1 month
No more than 6 months (more than 6 months is Schizophrenia) |
|
|
|
What is Schizoaffective disorder?
|
at least 2 weeks of stable mood with psychotic symptoms
+ a major depressive, manic or mixed episode |
|
|
|
A brief psychotic disorder has symptoms of schizophrenia that last ______
|
less than one month
|
|
|
|
This is defined as a fixed, persistent, non-bizarre (could be plausible) belief system lasting more than 1 month.
Functioning isnot otherwise impaired. |
Delusional Disorder
|
|
|
|
In order for a set of symptoms to be considered a "Manic" episode, they must be present for at least ______ and affect functioning
|
at least 1 week
**AFFECTS FUNCTIONING** |
|
|
|
How do you distinguish a manic episode from a hypomanic episode.
|
Manic = affects functioning
Hypomanic = doesn't affect functioning |
|
|
|
Cyclothymia is symptoms of dysthymia and hypomania, it is a milder form of bipolar disorder lasting at least ______
|
2 years
|
|
|
|
This is a milder form of depression lasting at least 2 years
|
Dysthymia
|
|
|
|
In order to be diagnosed with a major depressive episode, a patient must have symptoms for at least ____
|
2 weeks
|
|
|
|
What is a treatment option for pregnant women with major depressive disorder refractory to other treatments?
|
Electroconvulsive Therapy
-SE: anterograde/retrograde amnesia |
|
|
|
A patient presents with hypersomnia, over-eating and mood reactivity (able to have a good mood).
He is sensitive to rejection. |
Atypical Depression
**M/C type of depression** |
|
|
|
Drug of choice for acute panic attacks?
|
BZDs
|
|
|
|
Drug of choice for "stage-fright"?
|
Beta-blocker
|
|
|
|
Go over Defense Mechanisms
|
DIT-Psych Section (pg.16)
|
|
|
|
What are the Cluster A Personality Disorders?
|
Paranoid
Schizoid Schizotypal |
|
|
|
What are the Cluster B Personality Disorders?
|
Narcissistic
Histrionic Borderline Antisocial |
|
|
|
What are the Cluster C Personality Disorders?
|
Avoidant
Dependent Obsessive-Compulsive |
|
|
|
What sets Obsessive Compulsive Personality disorder apart from Obsessive Compulsive Disorder?
|
People with OC Personality Disorder have no idea they have a problem
|
|
|
|
What street drug causes Vertical + Horizontal nystagmus?
|
PCP
|
|
|
|
What are the "Mood Stabilizers" used in Bipolar disorder?
|
Lithium
Carbamazepine Valproic Acid |
|
|
|
Busiprone stimulates _____ receptors
|
5-HT1A receptors
-Tx: General Anxiety Disorder |
|
|
|
Which antipsychotic drugs cause extrapyramidal symptoms?
(tardive dyskinesia) |
**1st Generation**
-Haloperidol -Fluphenazine Trifluoperazine **Block D2 receptor** |
|
|
|
A patient who was recently prescribed antipsychotics presents with hyperpyrexia, rigidity, myoglobinuria and autonomic instability
|
Neuroleptic Malignant Syndrome
**Treat with dantrolene + Dopamine agonist (bromocriptine)** |
|
|
|
These drugs primarily treat the positive symptoms of Schizophrenia
|
Antipsychotics
|
|
|
|
These drugs treat both positive and negative symptoms of schizophrenia (mostly negative)
|
Atypical Antipsychotics
|
|
|
|
This atypical antipsychotic may cause agranulocytosis
|
Clozapine
|
|
|
|
These atypical psychotics cause considerable weight gain
|
Olanzapine/Clozapine
|
|
|
|
This atypical antipsychotic prolongs the QT interval
|
Ziprasidone
|
|
|
|
What is an endocrine side effect of the typical antipsychotics?
|
Hyperprolactemia
|
|
|
|
haloperidol + "-azines"
|
Antipsychotics (typical)
|
|
|
|
MOA of Antipsychotics (typical)
|
block D2 receptors
Tx: Schizophrenia, Tourettes |
|
|
|
Which atypical antipsychotic is used for OCD, anxiety disorder, depression, mania and Tourette's
|
Olanzapine
|
|
|
|
Which generation of antipsychotics has side effects of:
-Antimuscarinic = dry mouth, constipation -Histamine = sedation - α = HYPOtension |
2nd Generation Antipsychotics
-Chlorpromazine -Thioridazine |
|
|
|
Which TCA can be used to treat bedwetting?
|
imipramine
|
|
|
|
Why do you want to try and avoid TCA use in the elderly?
|
Antimuscarinic effects can cause confusion and hallucinations
**use nortryptyline** |
|
|
|
Which TCA has the largest antimuscarinic effect?
|
Amitriptyline
|
|
|
|
MOA of TCAs?
|
block reuptake of NE and Dopamine
|
|
|
|
Which antidepressant class causes the "Tri-C's" side effects of:
1) Convulsions 2) Coma 3) Cardiotoxicity (arrythmias) |
TCAs
|
|
|
|
How do you treat TCA overdose?
|
Alkalinize urine
**NaHC03** |
|
|
|
Antidepressants:
"iptyline" or "ipramine" + doxepin + amoxapine |
TCAs
|
|
|
|
Antidepressants:
Fluoxetine Paroxetine Sertaline Citalopram |
SSRIs
|
|
|
|
What happens if a patient takes an SSRI and an MAO inhibitor at the same time?
|
**Serotonin Syndrome**
-hyperthermia, myoclonus, CV collapse, flushing, diarrhea, seizures |
|
|
|
What is the antidote for Serotonin Syndrome?
|
Cyproheptadine
(5-HT2 agonist) |
|
|
|
What type of drug would you use in a patient with Bulemia?
|
SSRIs
------------- Fluoxetine Paroxetine Sertaline Citalopram |
|
|
|
What happens if you ingest tyramine while on an MAO inhibitor?
-Tranylcypromine -Phenelzine -Isocarboxazid -Selegiline |
Hypertensive Crisis
|
|
|
|
MAO inhibitors increase levels of which neurotransmitters?
|
NE
Serotonin Dopamine |
|
|
|
What is the MOA of Selegiline? Used in Parkinson's
|
MAO-B inhibitor
Prevents the breakdown of levodopa!! |
|
|
|
MOA of SNRIs
-Venlafaxine -Duloxetine |
block reuptake of NE, Serotonin
|
|
|
|
Name the SNRIs
|
-Venlafaxine
-Duloxetine |
|
|
|
Name the MAO inhibitors
|
-Tranylcypromine
-Phenelzine -Isocarboxazid -Selegiline |
|
|
|
Name the SSRIs
|
Fluoxetine
Paroxetine Sertaline Citalopram |
|
|
|
These drugs are used for:
-Depression -OCD -Bulemia -Social Phobias -PTSD |
SSRIs
------------ Fluoxetine Paroxetine Sertaline Citalopram |
|
|
|
Which SNRI is indicated for diabetic peripheral neuropathy?
|
duloxetine
|
|
|
|
This atypical anti-depressant is used for insomnia.
High doses are needed for anti-depressant effects. May cause ***priapism*** |
Trazodone
|
|
|
|
Does Buproprion have sexual side effects?
|
No
-also used for smoking cessation |
|
|
|
Name 2 drugs used for smoking cessation
|
Varenicline
Buproprion |
|
|
|
This Atypical-antidepressant is an α2 antagonist that ↑ release of NE + Serotonin
- it also stimulates 5-HT2 and 5-HT3 receptors **Antihistamine affects may ↑ appetite** **Sedation effects good for Depression + Insomnia** |
Mirtazapine
|
|
|
|
What % of body weight is:
-Total Body Water? -ICF? -ECF? |
-Total Body Water = 60%
-ICF = 40% -ECF = 20% (25% is plasma, 75% is interstitial) |
|
|
|
Where do the ureters pass near the vas deferens?
|
Ureters go UNDER the vas deferens
|
|
|
|
In a female, the ureters pass UNDER the ____ artey
|
Uterine
|
|
|
|
A loss of negative charge in the glomerular basement membrane will cause _____ syndrome
|
NEPHROTIC syndrome
|
|
|
|
Plasma volume is measured by radiolabeled _____
|
albumin
|
|
|
|
Extracellular volume is measured by _____
|
inulin
|
|
|
|
What is the equation for renal clearance?
|
Cx = (Ux χ V)/Px
-------------------------------------- Cx < GFR = net tubular reabsorption of x Cx > GFR = net tubular secretion of X |
|
|
|
Prostaglandins DILATE the AFFERENT arteriole
How does this affect GFR, RPF, FF? |
↑ GFR
↑ RPF No change FF |
|
|
|
ACE inhibitors CONSTRICT the EFFERENT tuble.
How does this affect GFR, RPF, FF? |
↑ GFR
↓ RPF ↑ FF |
|
|
|
Renal:
There is CONSTRICTION at the afferent arteriole. How does this affect GFR, RPF, FF? |
↓ GFR
↓ RPF No change FF |
|
|
|
Renal:
There is CONSTRICTION at the EFFERENT arteriole How does this affect GFR, RPF, FF? |
↑ GFR
↓ RPF ↑ FF |
|
|
|
Renal:
There is an INCREASE in plasma protein concentration. How does this affect GFR, RPF, FF? |
↓ GFR
No change RPF ↓ FF **Increased Viscosity** |
|
|
|
Renal:
There is a DECREASE in plasma protein concentration. How does this affect GFR, RPF, FF? |
↑ GFR
No Change RPF ↑ FF **Decreased Viscosity** |
|
|
|
Renal:
There is constriction of the ureter. How does this affect GFR, RPF, FF? |
↓ GFR
No change RPF ↓ FF |
|
|
|
Glucose is reabsorped in the proximal tubule by ____/glucose cotransport
|
Na+/glucose cotransport
|
|
|
|
Hartnup's Disease is a deficiency of ____ transport which results in ↓ Vit. B3 (niacin) and PELLAGRA
|
Tryptophan
--------------------------------------------- Pellagra 1) Diarrhea 2) Dermatitis 3) Dementia |
|
|
|
ADH binds to __ receptors at the collecting tubules of the nephron
|
V2 receptors
|
|
|
|
Renal:
These drugs block the Na+/K+/2Cl- transporter in the Thick Ascending Loop of Henle |
Loop Diuretics
|
|
|
|
Renal:
These drugs block the Na+/Cl- transporter in the Distal Convoluted Tubule |
Thiazides
|
|
|
|
Renal:
Which drugs work in the Collecting Tubule to inhibit Na+/K+ exchange |
Potassium Sparing Diuretics
|
|
|
|
How does ↑ sympathetic tone (β1) afect the JG cells?
|
↑ renin rlease
|
|
|
|
This hormone is released from the atria in response to ↑ volume.
Acts to "check" the RAAS system. Relaxes smooth muscle via cGMP --> ↑GFR --> ↓ renin |
ANP
|
|
|
|
How can NSAIDs cause renal failure?
|
↓ Prostaglandins needed to DILATE the afferent tubule in order to maintain GFR
|
|
|
|
What enzyme in the kidney converts:
25-OH Vit. D ↓ 1,25 (OH)2 Vit. D? |
1α-hydroxylase
|
|
|
|
Potassium Shifts:
- ↓ insulin - β-blockers - Acidosis/Extreme Excercise - Hyperosmolarity - Digitalis - Cell Lysis |
K+ shifts OUT OF CELL
↓ HYPERkalemia --------------------------------------- - ↓ insulin (blocks Na/K ATPase) - β-blockers (blocks Na/K ATPase) - Acidosis/Extreme Excercise (↑ K/H exchange) - Hyperosmolarity - Digitalis (blocks Na/K ATPase) - Cell Lysis |
|
|
|
Potassium Shifts:
↑ Insulin β-agonists Alkalosis Hypo-osmolarity |
Potassium shifts INTO cell
↓ HYPOkalemia ----------------------------------- ↑ Insulin (↑ Na/K ATPase) β-agonists (↑ Na/K ATPase) Alkalosis (↑ K/H exchange) Hypo-osmolarity |
|
|
|
U waves on ECG
Flattened T waves |
HYPOkalemia
|
|
|
|
What class of diuretic primarily affects Principle Cells in the Colecting Duct of the nephron?
|
K+ sparing diuretics
|
|
|
|
Does excess insulin cause hyperkalemia or hypokalemia?
|
Hypokalemia
Shifts K+ INto cells |
|
|
|
oxalate crystals in urine
|
Ethylene Glycol Ingestion
↓ Acute Tubular Necrosis |
|
|
|
What segement of the renal tubule is responsible for concentrating the urine?
|
collecting duct
|
|
|
|
What segement of the renal tubule is responsible for diluting the urine?
|
Thick Ascending Limb of Loop of Henle
(Impermeable to Water) |
|
|
|
What segement of the renal tubule is the only site where glucose and amino acids are absorbed?
|
Proximal tubule
|
|
|
|
What segement of the renal tubule is the only portion where water resorption occurs in the Loop of Henle?
|
Thin Descending Limb
|
|
|
|
Urine osmolarity < Serum Osmolarity
|
Diabetes Insipidus
|
|
|
|
Subendothelial immune complex deposits in gomeruli
|
Membranoproliferative GN
**See Tram Tracking** |
|
|
|
Subepithelial immune complexe deposits in glomeruli
|
Membranous GN
**Spikes and domes of BM*** |
|
|
|
Other than Polycystic Kidneys, what 3 other complications are associated with ADPKD?
|
MVP
Berry Aneurysm Hepatic Cysts |
|
|
|
What is the most common glomerular disease seen in HIV patients and Heroin users?
|
Focal Segmental Sclerosis
|
|
|
|
What is the most common nephrotic syndrome seen in adults?
|
Membranous GN
**Spikes and domes of BM*** |
|
|
|
Why are patients with a nephrotic syndrome in a hypercoaguble state?
|
Loss of Anti-thrombin III in urine
|
|
|
|
Crescents seen in urine
-Hemoptysis/Hematuria |
Goodpastures
**Linear Immunoflouresence** |
|
|
|
Crescents seen in urine
(+) p-ANCA |
Microscopic polyangitis
|
|
|
|
Crescents seen in urine
(+) c-ANCA |
Wegener's
|
|
|
|
What diseases are associated with Type I MPGN?
|
HBV
HCV |
|
|
|
What autoantibody is associated with Type II MPGN?
|
C3 nephritic factor
|
|
|
|
If a patient with SLE presents with a nephrotic syndrome, what is the most likely diagnosis?
|
Membranous GN
**Spike and Dome** |
|
|
|
What is the first step of nephrotic syndrome in a patient with Diabetes?
|
Non-enzymatic glycosylation of BM
|
|
|
|
What type of kidney stone would you see in a patient being treated for leukemia?
|
Uric Acid Stone
(high cell turnover) |
|
|
|
This Cancer presents with hematuria, palpable mass and flank pain.
-May see polycythemia |
Renal Cell CA
**May see polycythemia from ↑EPO** |
|
|
|
What autosomal dominant disease is associated with bilateral cenal cell CA?
|
von Hippel Lindau
(deletion Chromosome 3) |
|
|
|
What is the main rout of renal cell CA metastasis?
|
Spreads via IVC
|
|
|
|
Wilm's tumor is caused by a deletion of the WT1 gene on chromosome ____
|
chromosome 11
|
|
|
|
A patient complains of painless hematuria.
There are no casts in his urine |
Transitional Cell CA
|
|
|
|
What organism can cause squamous cell carcinoma of the bladder?
|
Schistosoma hematobium
|
|
|
|
These agents may cause what type of cancer?
-Phenacetin -Smoking -Aniline dyes -Cyclophosphamide |
Transitional Cell CA
|
|
|
|
Bladder biospy shows:
"Papillary growth lined by transitional epithelium with mild nuclear atypia and pleomorphism" |
Transitional Cell CA
|
|
|
|
What is the most common agent of pyelonephritis?
|
E. coli
|
|
|
|
What abnormality is required in order for a patient to have Chronic pyelonephritis?
|
Vesicourethral reflux
|
|
|
|
Renal imaging shows corticomedullary scarring, blunted calyx
- Biopsy reveals tubules contain eosinophilic casts that resemble thyroid follicles (Thyroidization of kidney) (+) Vesicourethral reflux |
Chronic pyelonephritis
|
|
|
|
Crush injuries can cause what renal problem?
|
Acute tubular necrosis
**d/t myoglobinuria** |
|
|
|
granular, "muddy brown" casts in urine
|
Acute tubular necrosis
|
|
|
|
Waxy casts in urine
|
Renal Failure
|
|
|
|
How do the following K+ sparing diuretics work?
-Amiloride -Triamterene |
Block Na+ channels in the collecting duct
|
|
|
|
What effect do ACE inhibitors have on renin?
|
Increased renin
(you are decreasing AT II) |
|
|
|
What effect do ACE inhibitors have on K+ levels
|
Hyperkalemia
(decrease aldosterone by blocking AT II formation) |
|
|
|
Histology for type I pneumocytes?
|
Squamous epithelium
|
|
|
|
Histology for type II pneumocytes?
|
Cuboidal
|
|
|
|
Which type of pneumocyte carries out gas exchange?
|
type I pneumocyte
|
|
|
|
Which type of pneumocyte is increased during episodes of lung damage?
|
type II pneumocyte
(proliferate to type I and type II pneumocytes) |
|
|
|
In the lungs, these cells are nonciliated columnar with secretory granules.
Secrete a component of surfactant, degrade toxins, and act as reserve cells |
Clara Cells
|
|
|
|
Where is the pulmonary artery located in relation to the Right Bronchus?
|
ANTERIOR
**RALS** |
|
|
|
Where is the pulmonary artery located in relation to the Leftt Bronchus?
|
SUPERIOR
**RALS** |
|
|
|
At what thoracic level does the IVC perforate the diaphragm?
|
T8
|
|
|
|
At what thoracic level does the esophagus and vagal branches perforate the diaphragm?
|
T10
|
|
|
|
At what thoracic level does the Aorta perforate the diaphragm?
|
T12
|
|
|
|
What extra muscles are used for inspiration in a person excercising heavily?
|
External Intercostals
Scalenes SCM muscles |
|
|
|
What serine protease activated bradykinin?
|
Kallikrein
|
|
|
|
What extra muscles are used for expiration in a person excercising heavily?
|
rectus abdominus
internal and external obliques transversus abdominus internal intercostals |
|
|
|
What nerve innervates the latissimus dorsi muscle?
|
Thoracodorsal n.
|
|
|
|
The Taut form of Hb has a ____ affinity for oxygen
|
Lower affinity
(curve shift right) |
|
|
|
The relaxed form of Hb has a _____ oxygen affinity
|
Higher affinity
(curve shift left) |
|
|
|
Which form of Iron on Hb binds to oxygen better?
Fe++ or Fe+++ |
Fe++
---------------------------------- Reduced (ferrous) Fe3+ causes methhemoglobinuria. has a higher affinity for CN- Tx: Methylene blue + Vit. C |
|
|
|
What is the treatment for cyanide poisoning?
|
1) Nitrites --> oxidize Fe2+ to Fe3+ --> forms methemoglobin which binds to CN-
2) Thiosulfate --> binds to this CN compund--> converts to thiocyanate --> renally excreted |
|
|
|
A patient presents with headache, blurry vision and a red tint to their skin.
Normal PaO2 Low SaO2 |
CO poisoning
--------------------------------- PaO2 (pulse ox) is normal because CO is binding to hemoglobin SaO2 is decreased because CO binds Hb with GREATER affinity than O2 |
|
|
|
CO causes a ____ oxygen binding capacity with a ____ shift in the oxygen disassociation curve
|
decreased oxygen binding capacity
left shift in oxygen disassociation curve |
|
|
|
Which way would the oxygen disassociation curve shift?
↑ CO2 ↑ BPG ↑ Exercise ↑ Acid/Altitude (decreased pH) ↑ Temperature |
Right Shift
------------------------------------ ↓ O2 affinity causes oxygen unloading in states where tissues need the oxygen |
|
|
|
Which way would the oxygen disassociation curve shift?
↓ CO2 ↓ BPG ↓ Exercise Alkalosis (increase pH) ↓ Temperature |
Shift Left
--------------------------- ↑ affinity for O2 means Hb will hang on to oxygen longer |
|
|
|
How do the lungs respond in instances of ↓ PAO2 (arterial oxygen)?
|
Hypoxic Vasoconstriction
-shunts blood away from poorly ventilated regions of the lung to better ventilated regions of the lung |
|
|
|
The area available for pulmonary perfusion _____ in emphysema
|
decreases
(less USABLE area) |
|
|
|
Why does fibrosis cause poor difusion?
|
Membranes are too thick!
|
|
|
|
How does excercise affect venous PO2?
|
↓ venous PO2
|
|
|
|
What heart anomaly may occur in persons trapped at a high altitude?
|
RVH from increased hypoxic pulmonary vasoconstriction
|
|
|
|
During excercise, the V/Q ratio from the apex to the base of the lung becomes more _____
|
unified
(closer to V/Q=1) |
|
|
|
A person who is on vacation in a high altitude may have what acid/base disoder?
|
Resp. Alkalosis
**Increased rate of breathing blows off CO2** |
|
|
|
What gene mutation is present in patients with primary pulmonary HTN?
|
Inactivating mutation of BMPR2
(normally functions to inhibit vascular smooth muscle proliferation) |
|
|
|
Name some drugs to treat pulmonary HTN
|
Bosentan
Ambriosentan Sildenafil Nifedipine (DHT CCB) |
|
|
|
What is the best imaging study for Pulmonary Embolism?
|
Helical CT
|
|
|
|
(+) Homan's sign
|
Pain in calf with dorsiflexion of foot
**DVT*** |
|
|
|
Where do most pulmonary emboli arise from?
|
Deep leg veins
|
|
|
|
Hypertrophy of mucus secreting glands in the bronchioles
-Reid index > 50& Wheezing, crackles, cyanosis |
Chronic Bronchitis
|
|
|
|
Why do patients with emphysema use "pursed lip" breathing?
|
increases airway pressure to prevent airway collapse during respiration
|
|
|
|
Chronic, necrotizing infection of the bronchi
-permanently dilated airways -purulent foul smelling sputum -recurrent infections, hemoptysis |
Bronchiectasis
Seen in: CF Kartagener's Chronic smokers Can increase risk of Aspergillosis |
|
|
|
When do type II pneumocytes mature in utero and begin to make surfactant?
|
35 weeks
|
|
|
|
What musculoskeletal disease can cause restrictive lung disease if the Cobb Angle is > 50 degrees?
|
Scoliosis
|
|
|
|
Silicosis increases the risk for ____ infection
|
TB infection
|
|
|
|
What restrictive lung disease features an increase in ACE?
|
Sarcoidosis
|
|
|
|
Name 3 drugs that cause pulmonary fibrosis
|
Busulfan
Bleomycin Amiodarone |
|
|
|
____ is failure of the right side of the heart brought on by long-term high blood pressure in the pulmonary arteries and right ventricle of the heart
|
Cor Pulmonale
|
|
|
|
"golden brown fusiform rods resembling dumbells"
-found in alveolar macrophages |
Asbestosis
|
|
|
|
"Egg-shell calcification of hilar lymph nodes"
|
Silicosis
|
|
|
|
What lung lobes does Asbestosis affect?
upper vs. lower |
lower lung lobes
------------------------------------ Silicosis + Coal miners = upper lobes |
|
|
|
dipalmitoyl phosphatidylcholine
|
surfactant
|
|
|
|
Risks for Infant ARDS?
|
Prematurity (less than 35 wk)
C-section Maternal Diabetes (↑ insulin) |
|
|
|
Why do you see polycythemia in sleep apnea?
|
↑ Hypoxia --> EPO --> Erythrocytosis
|
|
|
|
Trauma, sepsis, shock, gastric aspiration, pancreatitis, amniotic fluid embolism
↑ alveolar capillary permeability ↓ protein leaks into alveoli ↓ form intra-alveolar hyaline membrane |
Acute Respiratory Distress Syndrome
-initial damage is d/t immune response to toxic substances |
|
|
|
Which way does the trachea deviate in a patient with bronchial obstruction?
|
Toward side of destruction
|
|
|
|
In which lung cancer do you see a neoplasm of neuroendocrine "Kulchitsy Cells" --> small dark blue cells
-"salt & pepper" appearance |
Small (Oat) Cell carcinoma
-Central |
|
|
|
What is the most common lung cancer in non smoker and females?
**Develops in site of previous inflammation or injury** |
Adenocarcinoma
-Peripheral |
|
|
|
This Lung Cancer grows **along the airways**
-can present as pneumonia -may lead to hypertrophic osteoarthropathy |
Bronchioalveolar CA
|
|
|
|
Lung Cancer:
-Cavitation Biopsy shows "keratin pearls and intracellular bridges" |
Squamous Cell CA
-Central |
|
|
|
Lung Cancer:
-Linked to smoking -Cavitation -PTHrP secretion acts like PTH |
Squamous Cell CA
|
|
|
|
Lung Cancer:
-Peripheral -Highly anaplastic and undifferentiated -Biopsy: **Pleomorphic Giant Cells with leukocyte fragments in cytoplasm** |
Large Cell CA
|
|
|
|
Coal miners may have exposure to ___ which puts them at risk of developing lung cancer
|
Radon
|
|
|
|
Lung Tumor:
-may also present in the appendix -can cause fibrous deposits on right heart valves, especially the tricuspid valve. (May also cause pulmonary Stenosis, RHF) |
Carcinoid Tumor
|
|
|
|
-Obstruction of the SVC that impairs blood drainage fromt he head ("facial plethora"), neck (JVD) and Upper extremities (UE)
|
SVC Syndrome
-common with Lung Tumors and thromboses |
|
|
|
Pneumonia:
Which organisms may cause Bronchopneumonia? -Acute inflammatory infiltrates from bronchioles to adjacent alveoli See **Patchy infiltrates** involving one or more lobes |
-S. aureus
-H. influenzae -Klebsiella -S. pyogenes |
|
|
|
What organism cause interstitial pneumonia in infants and children?
|
RSV
Chlamydia (stacatto cough) |
|
|
|
What organisms cause interstitial (atypical) pneumonia in adults?
|
Mycoplasma
Legionella Chlamydia |
|
|
|
Respiratory:
-Localized collection of pus within parenchyma **Air fluid levels** seen on CXR |
Lung abscess
-S. aureus -Anaerobes (Bacteroides, Fusobacterium, Peptostreptococcus) |
|
|
|
Spontaneous pneumothorax occurs due to rupture of _____
|
apical blebs
|
|
|
|
Asthma drugs:
MOA of Theophylline? |
Causes Bronchodilation
-inhibits PDE --> ↓ cAMP hydrolysis (breakdown) **Blocks adenosine actions** |
|
|
|
Asthma drugs:
This drug prevents release of mediators from Mast cells. Prophylaxis for asthma |
Cromolyn
|
|
|
|
Which leukotriene receptor blocker can you use to treat asthma in a patient that is 1 year old?
|
Montelukast
------------------------------- Have to be at least 5 yo for Zafirlukast |
|
|
|
In asthma treatment, corticosteroids block the formation of almost all inflammatory cytokines.
They inactivate ____ the transcription factor for TNF-α |
NF-κB
|
|
|
|
How does Bosentan reduce pulmonary hypertension?
|
Blocks endothelin-1 receptors
-decreased pulmonary vascular resistance |
|
|
|
This drug is a synthetic codeine analog and has antitussive properties by blocking NMDA-glutamate receptors.
Mild opiod effect when used in excess |
dextromethorphan
|
|
|
|
This drug is used as an expectorant in CF patients
|
**N-acetylcysteine**
-also used for acetaminophen overdose --> regenerates glutathione |
|

