![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
Hair
|
transmits sensory information, protection, thermoregulation, secondary sex characteristic
|
|
|
3 types of hairs
|
1. lanugo- fine, long, formed during fetal life, sheds before birth. Develop more in old age.
2. vellus- short fine light colored hair covering most of the body. 3. terminal- longer thicker darker hairs on the scalp and the normal rate of growth is 0.4mm/24hrs |
|
|
Hair growth cycle
|
Anagen- growing phase. may last btw 3-6 years. (1 follicle)
Catagen- transitional phase. 2-3 wks, growth stops, root shrinks, papilla break away. Telogen- shedding phase. 3 mos. |
|
|
Androgenic Alopecia
|
male pattern baldness. Most prevalent type of hair loss in humans. gradual. common progressive balding tha toccurs through the combined effect of a genetic predisposition and the action of androgen on the hair follicles of the scalp.*
|
|
|
Epidemiology of androgenic alopecia
|
begins after puberty- often fully expressed in the 40s (males)
begins in women after menopause (decreased estrogen) |
|
|
Etiology and pathophysiology of androgenic alopecia
|
Dihydrotestosterone causes growth of androgen dependent hairs and loss of the non-androgen dependent scalp hair.
|
|
|
Clinical manifestations of androgenic alopecia for males.
|
Bitemporal recession followed by a bald crown and frontal thinning to lost of all hair except that along the occipital and temporal margins.
|
|
|
Clinical manifestations of androgenic alopecia for females
|
central regression or diffuse thinning maintaining the frontal hairline
|
|
|
Androgen excess in younge women
|
Acne, hirtruism, irregular menses, virilization. Transition of terminal hairs to vellus hairs due to dihydrotestosterone.
|
|
|
Baldness can be an indication of what in males?
|
Prostate disease, benign prostetic hypertropy, heart disease (MI)
|
|
|
Dx of androgenic alopecia
|
Biopsy- hair follicles do decreasing size and eventually nearly complete atrophy.
Hormone studies- total and free testosterone, dehydroepiandosteone sulfate Blood test- TSH test (pituitary gland) |
|
|
Tx of androgenic alopecia
|
Minoxidil, finasteride, antiandrogens, wigs and hair transplantation
|
|
|
Minoxidil
|
5% topical preparation, 1 mL applied BID, topical vasodilator. Increases blood flow to scalp to increase the anagen phase.
|
|
|
Finasteride
|
oral medication competitively inhibits enzyme that converts testosterone into dihydrotestosterone- lower serum and scalp levels.
|
|
|
Anti-androgens
|
may be affective in treating women- contraindicated in men. Used in younger women with hormonal imbalance.
|
|
|
Telogen Effluvium
|
Making hair go into the telogen phase. Major events may precipitate the end of the actively growing phase of the hair cycle for a varying portion of hair folliciles. Hair then shed diffusely from scalp. Will grow back.
|
|
|
Anagen effluvium
|
Abrupt cessation of growth- cuts off anagen phase and causes hair loss. May follow cytotoxic drug ingestion or poison ingestion.
|
|
|
Alopecia areata
|
localized loss of hair in round or oval areas without any visible inflammation or scarring. More common in children.
|
|
|
Pathophysiology of alopecia areata
|
Unknown. Thought to be immune response. T-lymphocytes interaction with aberrant HLA-DR antigens expressed by hair follicles. CD4/CD8 cells around bulbs.
|
|
|
Diseases associated with alopecia areata
|
Hashimoto's thyroiditis (common cause of hypothyroidism), vitiligo, myasthenia gravis
|
|
|
Clinical manefestations of alopecia areata
|
totalis- all head hair and eyebrows
universalis- all body hair gone Gradual hair loss with no pain or inflammation. Absence is weird bc on biopsy always signs of inflammation. |
|
|
If hair grows back, what does it look like?
|
thin, white or grey
|
|
|
Dx of alopecia
|
biopsy- follicles are reduced in size and lie high in the dermis. Peri-follicular lymphocyte infiltrate with dilated vessels followed by degenerative changes in the blood vessels that lead to the hair papillae.
|
|
|
Exclamation point hair
|
club shaped hairs that appear in pts with alopecia, narrower and closer to the scalp.
|
|
|
What tests should be run to rule out other possible causes of hair loss?
|
1. ANA- screening for Lupus
2. RPR- rule out syphilis 3. KOH prep- rule out fungal infx (tinea capitis) |
|
|
Tx of alopecia
|
Spontaneous remission = common. For patchy, immunosuppressants (steroids), topical or intralesional. For extensive, topical immunotherapy, PUVA, oral steroids. Psych consult.
|
|
|
Nail signs
|
1. nail pitting- punctate depressions of nail plate
2. leukonychia- white discoloration 3, Hutchinson's sign- brown-black periungual pigmentation 4. Clubbing- bulbous digits, >180 degrees between proximal end of nail fold and plate |
|
|
Subungual hematoma
|
Crushed nail. Accumulation of blood under the nail. Compression of matrix may cause secondary nail plate dystrophy.
|
|
|
Tx of subungual hematoma
|
Drainage of blood (25%+ full). Digit block. NO epinepherine- vasoconstriction = bad. RICE. To suture, must sew through the nail. Can use nail as bandage.
|
|
|
Splinter hemorrhages
|
induce by trauma, also occur in infective endocarditis* (bacteria on heart valves that float around and infect). Thin longitudinal dark red subungual lines (petechiae under nail)
|
|
|
Beau's lines
|
transverse depression more eviden in central portion of the nail. Traumatic. Presensce of Beau's lines in all nails at same level = systemic illness
|
|
|
Ingrown toenails
|
Improper or aggressive nail cutting or trauma; ill-fit shoes. Usually affects hallus of young adults. Congenital misalignment.
|
|
|
Clinical manifestations of ingrown toenail
|
Generally laterally ingrowing. Painful. Inflammed granulation tissue- exudate, abscess, crusting possible.
|
|
|
Tx of ingrown toenail
|
removal of piece embedded. Flat object to lift edge of toenail, soak, cut to proper length and educate patient to cut straight across.
|
|
|
Onycholysis
|
detatchment of nail from its bed at distal and/or lateral attachments creating a subungual space that collects dirt and keatinous debris. Nail develops grayish white color due to presence of air under toenails.
|
|
|
Onychomycosis
|
chronic progressive infx of nail apparatus caused by dermatophytes most commonly and less often by candida and molds- tinea unguium. Onycholysis. 80% on big toe. Painful- ulcerations under nail bed lead to 2nd infx
|
|
|
Etiology of onychomycosis
|
dermatophytes = 95-97%
yeast = 2% |
|
|
Risk factors for onychomycosis
|
immunocompromised individuals, HIV infx, diabetics
|
|
|
Pathophysiology of onychomycosis
|
Increased fungal invasion with defective vascular blood supply. Post trauma states or nerve damage. Nail bed produces soft keratin stimulated by fungal infx* that accumulates under the nail plate causing it to rise. Causes nail to be cream color.
|
|
|
Clinical presentation of onychomycosis
|
Classified by groups- DLSO, PSO, CO
|
|
|
Distal lateral subungual onychomycosis (DLSO)
|
Most common. Usually associated with tinea pedis (invades underside of nail). Originating in distal nail bed, spreads proximally (can involve entire nail). Appears white or yellow-brown hyperkeratotic, cracked nail with crumbling debris.
|
|
|
Proximal subungual onychomycosis (PSO)
|
Rare. Immunosuppressed pts. Begins with fungal invasion of the proximal nail fold by invasion of the nail plate and then distal invovlement. Appears sharply defined white area on the nail surface that moves distally to involve much of the undersurface of the nail plate.
|
|
|
White superficial onychomycosis (PSO)
|
Direct invasion into the superficial nail plate. Infection to nail bed that is milky white speckled. Powdery patches on surface of nail plate.
|
|
|
Candidal onychomycosis
|
Yeast infx under the nail. Begins with proximal and lateral paronychia which appears clinically as edema, erythema and pain of the nail fold at times pus can be expressed. Having paranychial inflammation distinguishes it from DSO. Note color change.
|
|
|
Appearance of onychomycosis
|
nail plate becomes dystrophic with areas of opacification, white, yellow, green, or black discoloration with transverse furrowing (Beau's lines)
|
|
|
Dx of onychomycosis
|
nail biopsy with KOH prep.
|
|
|
Tx of onychomycosis
|
Will not spontaneously resolve. Limited to outer layer of skin, hair, nails.
1. debridement 2. topical antifungals 3. systemic agents |
|
|
Debridement of onychomycosis
|
Dystrophic nails must be removed. Oral medications taken with removal of subungual pockets of hyphae
|
|
|
Topical anti-fungal agents used for onychomycosis
|
Available as lotions/lacquer.
1. amorolfine nail lacquer 2. ciclopirox 8% nail lacquer. *ALMOST USELESS. Long term treatments. |
|
|
Systemic agents used for onychomycosis
|
1. Terbinafine *superior treatment
2. Fluconazole 3. Itraconazole 4. Griseofulvin (long term tx) |
|
|
Patient education for onychomycosis
|
Protective footwear, cotton socks.
antifungal/absorbent powders. |
|
|
Will nails appear normal after the recommended dose of tx?
|
NO nail regrowth is slow- fungal infx may be gone but nails will not immediately look better
|
|
|
Paronychia
|
tissue infx of nail fold usually caused by staph aureus or candida.
|
|
|
acute paronychia
|
inflammation of the nail fold produces erythema, swelling, and throbbing pain. may extend into the proximal nail fold. Manicure is common cause.
|
|
|
chronic paronychia
|
inflammatory disorder of the proximal nail fold occuring in individuals whose hands are constantly in a wet environment.
|
|
|
Dx of paronychia
|
gram stain and culture
|
|
|
Tx of paronychia
|
responds to removal or protection of the nail apparatus from the chronic condition. Systemic antibx, systemic antivirals, topical application of antifungal cream to nail fold and weekly antifungal PO
|
|
|
Felon
|
subQ infx of the distal pulp space of the phalanx of a digit usually caused by staph or strep- granulation growth.
|
|
|
What type of an infx is a felon considered to be?
|
closed space infx- contained by unyielding skin of the finger tip, the infx creates tension with the microvascular compromise, necrosis and abscess formation.
|
|
|
Tx of felon
|
incision and drainage, oral antibx x 10 days, naph, ox, clox, diclox
|
|
|
Complications of felon
|
osteomyelitis, tenosynovitis, or septic arthritis
|
|

What disorder of the hair is presented here?
|
Adnrogenetic alopecia
|
|

What disorder of hair is this?
|
Alopecia areata
|
|
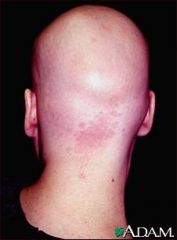
What hair disorder is this?
|
Alopecia areata totalis
|
|
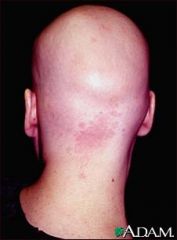
What hair disorder is this?
|
Alopecia areata totalis
|
|
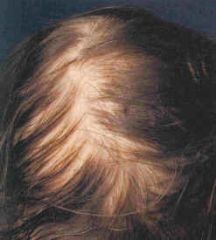
What disorder of the hair is this?
|
Telogen effluvium
|
|

What disorder of the nail is this?
|
Nail pitting
|
|
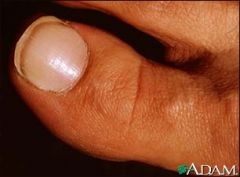
What nail sign is this?
|
Leukonychia
|
|

What nail sign is this?
|
Hutchinson's sign
|
|

What nail sign is this?
|
clubbing
|
|

What nail trauma is this?
|
Subungual hematoma
|
|

What nail trauma is this?
|
splinter hemorrhage
|
|

What nail trauma is this?
|
Beau's lines
|
|

What kind of nail trauma is this?
|
Ingrown toenail
|
|

What kind of nail abnormality is this?
|
Onycholysis
|
|

What kind of nail infection is this?
|
Onychomycosis
|
|

What kind of nail infection is this?
|
Onychomycosis
|
|

What kind of nail infection is this?
|
DLSO (distal lateral subungual onychomycosis)
|
|

What kind of nail infection is this?
|
PSO (proximal subungual onychomycosis)
|
|

What kind of nail infection is this?
|
Candidal onychomycosis
|
|

What kind of nail infection is this?
|
Paronychia
|
|

What kind of nail infection is this?
|
felon
|

