![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
89 Cards in this Set
- Front
- Back
|
Acne Vulgaris- general characteristics
1. definition 2. risk factors |

1. inflammatory condition of the skin that is most prevalent during adolescence.
2. Severe acne is more common in men than in women due to higher levels of circulating androgens. other RFs include puberty, Cushing's syndrome, oily complexion and medications. There is NO proven like between acne and diet (chocolate and fatty foods). OCPs do help some women with acne |
|
|
Acne vulgaris- pathogenesis
|
a. obstruction of sebaceous follicles (by sebum) leads to proliferation of propionibacterium acnes (an anaerobic bacterium in the sebum)
b. this obstruction can lead to either noninflammatory comedones (pimples) or if severe, inflammatory papules or pustules c. both noninflammatory and inflammatory lesions are present in most patients with acne |
|
|
Classification of acne vulgaris
1. obstructive acne (2) 2. Inflammatory acne |
1. obstructive- closed comedones (whiteheads) or open comedones (blackheads)
2. inflammatory- lesions progress from papules/pustules to nodules, then to cysts, then scars |
|
|
Acne Vulgaris Treatment -general guidelines
|
1. instruct patient to keep affected area clean (vigorous washing is unnecessary), reduce or discontinue acne-promoting agents (certain make-up, creams, oils, steroids, androgens)
2. It takes about 6 weeks to notice the effects of medications (skin may get worse before it gets better). Start with one drug to assess its efficacy. |
|
|
Treatment of Mild to Moderate Acne
|
1. begin with topical benzoyl peroxide (2.5%) - should be applied once or twice daily. It destroys acne-causing bacteria and prevents plugging of pores by drying the skin
2. add topical retinoids if the above fails. They cause peeling of the skin, which prevents clogging of pores. 3. Add topical erythromycin or topical clindamycin- both to suppress p. acnes |
|
|
Treatment of moderate to severe nodular pustular acne
|
1. prescribe systemic antibiotic therapy- tetracycline, minocycline, doxycycline, erythromycin, clindamycin, and TMP-SMX
2. Add oral retinoids (isotretinoin) for severe, recalcitrate, nodular acne that is not responsive to other treatments. Oral retinoids are extremely teratogenic. All females MUST have two negative pregnancy tests before start this medication. In addition, they should use two forms of birth control for 1 month prior to starting the medication through 1 month after stopping it. |
|
|
rosacea
|

- a chronic condition resulting in reddening of the face (mainly the forehead, nose, and cheeks). If often appears very similar to acne, but unlike acne it first starts in middle age
- mostly affects caucasian women between 30-50 years of age - the most common findings include erythema, telangiectasia, papules, and pustules with redness, typically affecting the face. There are NO comedones - In severe cases, the skin can become thickened and greasy- on the nose, it creates a bullous appearance, this is called rhinophyma and is mostly seen in men |
|
|
Treatment of Rosacea
|
- symptoms may be reduced by avoiding alcohol and hot beverages, as wells as extremes of temperature and by reducing emotional stressors
- treatment: topical metronidazole (gel form) is effective and is applied twice per day for several months. Systemic antibiotics (e.g. tetracycline) are used for maintenance therapy. If the patient does not experience an appropriate response, prescribe isoretrinoin for daily use. |
|

Keratocanthoma
|
- epithelial tumors which clinically resemble squamous cell carcinoma (SCC). Current debate centers on whether this is subtype of SCC or a separate entity altogether.
- Lesions grow VERY quickly. The lesions progress to the typical dome with central crater containing keratinous material over the course of several weeks. This type of growth is very rare for SCC. - Treatment- involves observation, as many of these will regress spontaneously over several months. |
|

Tinea Versicolor
|
- a common superficial fungal infection which is likely caused by several species in the Malassezia group, which are a part of the normal skin flora
- characteristic lesions are well demarcated and most commonly affect the trunk. As the name implies, lesions may be hyper or hypo-pigmented and can range from brown to tan to white - adolescents and young adults are most commonly affected, though almost any age can be affected - hot/humid whether, excessive sweating and skin oils may contribute to transformation from normal skin flora to pathologic condition |
|

Diagnosis and treatment of tinea versicolor
|
- diagnosis should be made with KOH wet prep, which will show the "spaghetti and meatballs" pattern consistent with both hyphae and yeast balls
- treatment consists or oral and topical antifungals, depending on the severity of the disease. Selenium sulfide lotion may also be helpful |
|

Seborrheic Dermatitis - general characteristics
|
1. A chronic, idiopathic, inflammatory skin disorder which occurs in infants and adults
2. Very common problem (affects 5% of the population), especially in patients with oily skin 3. exacerbating factors: anxiety, stress, fatigue and hormonal factors 4. Common locations: scalp (dandruff), hairline, behind ears, external ear canal, folds of skin around nose, eyebrows, armpits, under breasts, groin area 5. may be complicated by secondary bacterial infection |
|

Seborrheic dermatitis - clinical features
|
1. mild cases manifest as dandruff
2. scaly patches with surrounding areas of mild to moderate erythema 3. usually asymptomatic, but pruritus can occur |
|
|
Treatment of seborrheic dermatitis
|
1. sunlight exposure often helps
2. dandruff shampoo (OTC) is usually adequate 3. Topical ketoconazole (to decrease yeast count on skin) has been found to be effective 4. Topical corticosteroid are appropriate in severe cases |
|

Contact Dermatitis - general characteristics
1. two forms- which is more common - description of each type |
1. Two forms: irritant and allergic
2. Irritant contact dermatitis- more common than the allergic type- results from chemical or physical insult to the skin (e.g. contact with detergents, acids or alkalis from frequent hand washing). A previous sensitizing event is not needed to produce the rash (i.e. it is not an immunologic reaction). The rash begins shortly after exposure to the irritant (in contract to the allergic type, which begins several hours to a few days later-- delayed hypersensitivity) 3. Allergic contact dermatitis is a delayed-type hypersensitivity (type IV) reaction. No history of atopy is necessary for allergic contact dermatitis to occur. It can occur in anyone. |
|
|
Pathogenesis of allergic contact dermatitis
|
- a delayed-type hypersensitivity (type IV) reaction. No history of atopy is necessary for allergic contact dermatitis to occur. It can occur in anyone.
- Sensitization of the skin occurs 1-2 weeks after the first exposure to the allergen. Subsequent exposure leads to dermatitis hours to days after re-exposure. Therefore, dermatitis develops only in patients who have already been sensitized to the allergen. Common allergens include poison ivy, oak and sumac, nickel, rubber, topical medications (neomycin, topical anesthetics and cosmetics) |
|
|
Clinical features of contact dermatitis
|

The appearance of the rash depends on the stage
a. acute stage - erythematous papules and vesicles with oozing, edema may be present b. chronic stage: crusting, thickening and scaling; lichenification - the rash is usually very pruritic - the interval between exposure and appearance of the rash varies, but is usually from several hours to as long as 4-5 days - the rash is found only in exposed areas |
|
|
Diagnosis of contact dermatitis
|
1. Diagnosis is usually made clinically based on history and examination
2. patch testing (to identify the allergen that caused the allergic reaction) is indicated in any of the following cases: the diagnosis is in doubt, the rash does not respond to treatment, the rash recurs. |
|
|
Treatment of contact dermatitis
|
1. avoid the contact allergen
2. apply cool tap water compresses 3. apply topical steroids 4. prescribe systemic corticosteroids (e.g. prednisone 1mg/kg/day) for severe cases. Continue for 10-14 days then taper |
|
|
Pityriasis Rosea
|

- Papulosquamous erruption - initially "herald patches" that resemble ring worm (multiple round/oval patches) appear and then a generalized rash with multiple oval-shaped lesions appear. The rash is typically described as having a Christmas tree-type appearnance
- it is NOT contagious and is possibly related to herpes type 7 - It is common on the trunk and upper arms and thighs and is usually NOT found on the case. Pruritus is often present and varies in severity - It spontaneously remits within a few (6 to 8 weeks) without treatment. There is no treatment other than antihistamines for pruritus. Recurrences are rare |
|
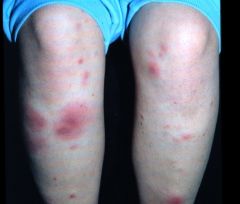
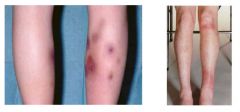
Erythema Nodosum
- appearance and symptoms - course - epidemiology |
- painful, red, subQ, elevated nodules typically located over the anterior aspect of the tibia (less commonly on the trunk or arms)
- it is self-limited and usually resolved within a few weeks. Low-grade fever, malaise and joint pain may precede the rash - it is more common in women- esp young women |
|
|
Erythema Nodosum - causes
|
- streptococcus infection, sarcoidosis, IBD, Behcets disease, fungal infections, pregnancy, medications (OCPs, sulfa drugs, amiodarone, antibiotics), syphilis, tuberculosis
- many cases are idiopathic |
|
|
Determining the underlying cause of erythema nodosum
|
Chest Xray- for sarcoidosis and tuberculosis
- ASO titer - VDRL - syphilis - CBC - ESR - cultures - consider skin biopsy |
|
Treatment of erythema nodosum
|
- treat the underlying cause
- prescribe bed rest, leg elevation, NSAIDs, and heat for symptoms. - Potassium iodide may help |
|

Erythema multiforme
|
- inflammatory skin condition characterized by erythematois macules/papules that resemble target lesions "bull's eye lesions" that can become bullous
- skin lesions may be pruritic and painful - EM can be caused by medications and may follow and infection by HSV. Many cases are idiopathic. - Medications implicated include sulfa drugs (most common), penicillin, and other antibiotics, phenytoin, allopurinol and barbiturates - if initiated early when the first symptom of HSV infection appears, acyclovir can help to prevent HSV-associated EM. For recurrent and debilitating EM, acyclovir may be given prophylactically for prolonged periods - antihistamines or analgesics for symptomatic relief |
|
|
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis
- definition - areas involved - systemic manifestations |
- No precise definition exists, but SJS is considered the most serve form of erythema multiforme. TEN is considered the most severe form of SJS
- In SJS and TEN, skin involvement is extensive and severe, with possible detachment of areas of epidermis - the eyes and mouth may also be involved - systemic manifestations include fever, difficulty eating, renal failure and sepsis |
|
|
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis - course, diagnosis and treatment
|
- Potentially LIFE-THREATENING (mortality rate is 5% for SJS and 30% for TEN)
- half of all cases are due to medications (e.g. sulfa drugs, penicillins, barbiturates, phenytoin, allopurinol, carbamezapine, vancomycin, rifampin). In many cases, no specific cause is identified - Admit the patient to an ICU - the burn unit is often the most appropriate setting. Withdraw the suspected medication - give aggressive rehydration and symptomatic management - urgent derm and ophtho consults |
|

Lichen Planus
|
- chronic inflammatory lesions of unknown etiology
- 4Ps- pruritic, polygonal, purple, flat-topped papules - most common seen on wrists, shins, ORAL MUCOSA, and genitalia - treat with glucocorticoids |
|

Bullous Pemphigoid
|
- multiple subepithelial blisters on abdomen, groin and extremities
- elderly people are the most commonly affected - blisters are less easily ruptures than in pemphigus vulgaris - autoimmune condition with no malignant potential. - may be persistent - treat with systemic or topical glucocorticoids |
|

Pemphigus Vulgaris
|

- autoimmune blistering condition resulting in loss of normal adhesion between cells (acantholysis)
- starts in oral mucosa, may become generalized - blisters rupture, leaving painful erosions - most commonly affects elderly people, often FATAL if untreated - Autoantibodies (usually IgG) directed against the adhesion molecule DESMOGLEIN - treat with systemic glucocorticoids and other immunosuppressants - pemphigus may be the presenting symptoms of malignancies such as non-Hodgkin lymphoma, CLL and Castleman's disease - positive Nikolsky sign on exam |
|
|
Warts- general characteristics
|
1. warts are caused by HPV and are transmitted via skin-to-skin contact. For genital warts, transmission is via intimate sexual contact
2. Types a. The common wart - verucca vulgaris- most common type. b. The flat wart (verucca plana) c. the plantar wart (veruruca plantaris) d. anogenital wart (condyloma acuminatum)- most common STD |
|
|
Verruca vulgaris
|
- most common type of wart
- may occur anywhere, but the most common sites include elbows, knees, fingers and palms - appearance: flesh-colored or whitish with a hyperkeratotic surface |
|
|
Verruca plana
|
the flat wart
- common sites include the chin/face, dorsum of hands, and legs - appears flesh-colored with smooth papules and a flat surface |
|
|
Plantar wart
|

-verucca plantaris
- solitary or multiple warts found on the plantar side of the foot, can cause foot pain if located on pressure areas (e.g. metatarsal head, heel) - appearance: flesh-colored with rough, hyperkeratotic surface |
|
|
Anogenital wart
|

- most common STD, commonly associated with HPV 6 and 11
- HPV (types 16,18) infection can lead to cervical cancer in women (pap smear is important) - Vaccines which protect against HPV 16 and 18 are now available. These vaccines have been shown to prevent HPV infection as well as adenocarcinoma and precancerous lesions associated with these HPV types. This is the first vaccine approved to prevent cancer - appearance: single or multiple, soft, fleshy growths on the gentialia, perineum, and anus |
|
|
Clinical features of warts
|
- most warts are asx unless "bumped".
- plantar warts can be painful during walking - some warts may bleed - warts may be disfiguring |
|
|
Treatment of warts
- general - flat warts - genital warts |
- freezing lesion with liquid nitrogen (applied on a cotton swab)- multiple treatments may be necessary
- salicylic acid (compound W)- applied daily for several weeks - 3-FU cream or retinoic acid cream for flat warts - surgical excision or laser therapy - podophylin for genital warts |
|
|
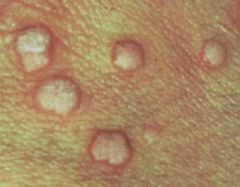
Molluscum contagiosum
|

- a common, self-limited viral infection caused by a poxvirus, common in sexually active young adults and in children
- it manifests as small papules (2-5 mm) with CENTRAL UMBILICATION. Lesions are asymptomatic. In HIV-positive patients, lesions can be extensive - It is transmitted via skin-to-skin contact (sexual contact can lead to genital involvement) and is HIGHLY contagious. - child abuse should be ruled out when a young child presents with molluscum - It persists up to 6 months, but spontaneously regresses with time. In immunosuppressed individuals (HIV positive patients), the lesions can progress to grown quite large and often refractory to treatment - multiple treatment modalities are effective (e.g. curettage, drops containing podophyllin and cantharidin, cryosurgery), but scarring is also a risk |
|
|
Herpes Zoster - Shingles - general characteristics
|
- caused by re-activation of the varicella-zoster virus, which remains dormant in the dorsal root ganglia and is reactivated in times of stress, infection or illness, only occurs in those who have previously had chickenpox
- It is typically seen patients over 50 years of age. In patients less than 50 years of age, suspect an immunocompromised state - contagious when open vesicles present and only for those who have never had chickenpox or are immunocompromised (or newborns). Zoster is not as contagious as chickenbox |
|
|
Herpes Zoster - clinical features
|
- severe pain and rash in a dermatomal distribution. Pain comes before the rash. Rash is characterized by grouped vesicles on an erythematous base. If severe, low grade fever and malaise may be present
- the most common sites of involvement are the thorax (most cases) and trigeminal distribution (especially ophthalmic division). Affected sites can also include other cranial nerves, as well as arms and legs - rarely life threatening, even if dissemination occurs. Herpes zoster is more severe, however, in immunocompromised patients |
|
|
Herpes Zoster - treatment
|
- keep lesions clean and dry
- prescribe analgesics for pain relief (aspirin or acetaminophen; codeine if needed). In severe cases, administer a local injection of triamcinolone in lidocaine. - prescribe antiviral agents (acyclovir, famciclovir, valacyclovir) to reduce the pain, decrease the length of illness and reduce the risk of postherpetic neuralgia - the use of corticosteroids to decrease the incidence of postherpetic neuralgia remains controversial |
|
|
Herpes Zoster vaccine
|
- live vaccine has been shown to be effective in reducing the number of cases of shingles in patients over the age of 60, in addition to reducing the severity and duration of postherpetic neuralgia in patients who do end up with the disease.
- The vaccine should be recommended to all patients over 60 who do not have contraindications |
|
|
Dermatophytes
|
- dermatophytes are superficial fungi that infect cutaneous epithelium, nails and hair
- the three main genera of dermatophytes are Tricophyton, microsporum, and epidermophyton - scrape lesions and use KOH preparation to visualize the fungus |
|
|
Scabies - general characteristics
|

- causes by the human skin mite sarcoptes scabiei var hominis
- highly contagious- transmitted via skin-to-skin contact or through towels, bed linens, or clothes - pathogenesis- the mites tunnel into the epidermia, lay eggs, and deposit feces (called scybala). A delayed type IV hypersensitivity reaction develops toward the mites, eggs, and feces, causing intense pruritus - common locations include: fingers, interdigital areas, and wrists. Elbows, feet, ankles, penis, scrotum , buttocks and axillae. - head, neck, palms and soles are typically spared (except in infants, the elderly or immunosuppressed) |
|
|
Scabies- clinical features
|
1. severe pruritus - this is often the most severe during the night. The head and neck are usually spared
2. burrows- linear marks (several millimeters in length) represent the tunneled path of the mite. There is typically a dark dot at one end, representing the female mite 3. scratching may lead to excoriations 4. eczematous plaques, crusted papules, or secondary bacterial infection may develop |
|
|
Diagnosis of scabies
|
- look for characteristic burrows on hands, wrists and ankles, and in the genital region
- confirm the diagnosis by scraping the burrow with a scalpel and examining it under a microscope to detect the present of mites, ova and scybala |
|
|
Treatment of scabies - medications
|
1. permethrin 5% cream (elimite)
- first-line treatment; causes paralysis of the parasite (acts on nerve cell membrane) - should be applied to every area of the body (head to toe), even under fingernails and toenails, around the genital area and in cleft of the buttocks - patients should leave cream on overnight (>8 to 10 hours) and wash it off the next morning - LINDANE (y-benzene-hexachloride) lotion- second-line treatment which should not be used unless permethrin is not available, is contraindicated or has failed - contraindicated in children under 2 years of age, as well as in pregnant or lactating women, due possibility of severe seizures |
|
|
Treatment of scabies- general recommendations
|

- treat all close contacts of the patient simultaneously (even in asymptomatic) with permethrin 5% cream
- the patient is no longer contagious after one treatment, although pruritus may continue for a few weeks as dead mites are shed from the skin. Use topical corticosteroids and oral antihistamines to control pruritus during this time - thoroughly wash all underwear and bed linens |
|

Actinic Keratosis
|
-aka solar keratosis
- small, rough, scaly lesions due to prolonged and repeated sun exposure - most commonly seen in fair-skinned people. Lesions are typically on the face - prevention: advise patients to avoid excessive sun exposure and to use sunscreen - although the risk of malignant transformation is low (1 in 1,000) biopsy is still recommended for hyperkeratotic actinic keratosis lesions to exclude SCC. Additionally, lesions which become indurated, tender, or bleed spontaneously must be biopsied to exclude SCC - treatment options include surgical removal (scraping), freezing with liquid nitrogen or application of 5-FU for multiple lesions (destroys sun-damaged skin cells) |
|

Basal cell carcinoma
|
- the most common skin cancer - account for 60-75% of all skin cancers
- it arises from the basal layer of cells in the epidermis - the most important risk factor is sun exposure - It occurs most frequently in fair-skinned individuals who burn easily and involves sun-exposed areas, such as the head and neck (the nose is the most common site) - the classic experience is a pearly, smooth papule with rolled edges and surface telagiectasias (3 Ps: pearly, pink, papule) - mets are extremely rare, but it can be locally destructive - surgical resection is curative |
|

Squamous cell carcinoma
|
- SCC is less common than basal cell carcinoma (SCC accounts for less than 20% of all skin cancers)
- it arises from epidermal cells undergoing keratinization sunlight exposure is the most important risk factor. Concomittant actinic keratoses, chronic skin damage and immunosuppressive therapy are also risk factors. - It is typically described as a crusting, ulcerated nodule or erosion - the likelihood of metastasis is higher than with basal cell carcinoma, but much lower than melanoma - the prognosis is excellent if it is completely excised (95% cure rate). Lymph node involvement, however, carries a poor prognosis |
|
|
Melanoma - general characteristics
|
- most aggressive form of skin cancer and the number on caused of death due to skin cancer
- increasing incidence worldwide |
|
|
Risk factors for melanoma
|
fair complexion (primarily affects Caucasian patients, especially those of the following - inability to tan, easily sunburned, red hair and/or freckles, numerous moles),
- sun exposure (patients with a history of a severe sunburn before age 14, patients living in a sunny climate, family history of melanoma in a first-degree relative, - genodermatoses (e.g. xeroderma pigementosa), - increasing age - large number of nevi (moles) - although most melanomas arise de novo, they may arise from pre-existing nevi in up to 50% of cases. Any change in a nevus is concerning because it may indicate malignancy or malignant transformation. Look for color change, bleeding, ulceration or a papule arising from the center of an existing nevus |
|
|
Dysplastic nevus syndrome
|
- numerous, atypical moles- these tend to be large with indistinct borders and variations in color. The chances of a single dysplastic nevus becoming a melanoma are small
- if dysplastic nevus syndrome and family history of melanoma are present, the risk of developing melanoma approaches 100% |
|
|
Giant congenital nevi
|
- the risk of melanoma is about 5-8%
- prophylactic excision is recommended |
|
|
Melanoma growth phases
|
1. radial (initial) growth phase - growth is predominantly lateral within the epidemis. there is a good prognosis with surgical resection because metastasis is unlikely
2. vertical (later) phase - growth extends into the reticular dermis or beyond. Lymphatic or hematogenous mets may occur. DEPTH of invasion is the most important indicator of prognosis |
|
|
What is the most important indicator of prognosis in melanoma?
|
DEPTH of invasion
|
|
|
Clinical features of melanoma
|
- asymmetry may present with some or all of the following features
- border irregularity - color variation - ranging for pink to blue to black - diameter gram than 6 mm - elevation - typically has raised surface - changing mole- most common presentation - the most common site is the back - advanced lesions often present with itching and bleeding |
|
|
Diagnosis of malignant melanoma
|
- excision biopsy is the standard of care for diagnosis of any suspicious lesion
- shave biopsy and punch biopsy are less accurate than excision biopsy is assessing the depth of invasion - lymph node dissection if appropriate if nodes are palpable |
|
|
Treatment of malignant melanoma
|
- early detection is the most important way to prevent death, because the prognosis is directly related to depth of invasion
- perform lymph node dissection if nodes are involved. this is controversial because of the risk of lymphedema and the little benefit gained in patients with distant mets |
|
|
Decubitus ulcers
- pathogenesis - risk factors - where are they most common |
- also called pressure sores
- they result from necrosis of tissue that becomes ischemic and ulcerated and they are causes by prolonged weight of the patient - risk factors include immobilization for any reason, peripheral vascular disease and dementia. Those at increased risk include debilitated or paraplegic people, nursing home residents, and people with neurologic disorders - they typically occur over bony prominences. The sacrum, greater tuberosity and ischial tuberosity are the most common sites. Other sites include the calcaneus, malleoli occiput, elbows and back |
|
|
Decubitus ulcers - complications and prevention
|

- if unrecognized and untreated, tissue can become necrotic and secondary bacterial infection can occur.
- cellulitis, osteomyelitis, sepsis, necrotizing fasciitis, gangrene, tetanus and wound botulism are all potential consequences - prevention is most important: patients should be turned and repositioned every 2 hours. Special mattresses and beds are designed to reduce local tissue pressure by distributing it more evenly |
|
|
Treatment of decubitus ulcers
|
- local wound care (e.g. for more superficial ulcers)
- wet-to-dry dressings or wound gel for deeper ulcers - surgical debridement of necrotic tissue - antibiotics if evidence of infection (e.g. surrounding cellulitis) |
|
|
Psoriasis - general characteristics
|
- psoriasis is due to abnormal (markedly accelerated) proliferation of skin cells. Because of this, the skin does not have time to mature normally. This leads to defective keratinization, which causes the scaling
- the cause is unknown - this is chronic condition characterized by exacerbations and remissions - it improves during the summer (sun exposure) and worsens in the winter (dries skin) - trauma to the skin in any form (e.g. infection, abrasion) can cause exacerbations, as can psychosocial stress - up to 3/4 of patients have somewhat localized disease (<20% to 25% of body surface area). Nevertheless, clinical features vary and some patients have generalized skin involvement - less than 10% of patients develop psoriatic arthritis |
|

Clinical features of psoriasis
|
- well, demarcated erythematous papules and plaques that are covered by thick, silvery scaling
- pruritus is rare - Auspitz's sign- removal of the scale causes pinpoint bleeding - it can involve any part of the body, but the most common areas are the EXTENSOR surfaces of extremities (knees, elbows), scalp, intergluteal cleft, palms and soles - pitting of the surface of nails, or onocholysis (distal separation of nails from the nail bed) |
|
|
Treatment for psoriasis - topical therapy
|
- corticosteroids are the most commonly prescribed first-line agents, but they have adverse side effects with prolonged use
- calcipotriene and calcitriol ar vitamin D derivatives that have become first or second-line agents. They are very effective in most patients - tars have an unpleasant odor, so they are less desirable to use. Patients should use tars for 4-6 weeks before expecting to see benefit. Tars are more effective in combination therapy and are associated with an 80-90% remission rate - other options include tazarotene (vitamin A derivative) and anthralin - combination therapy (e.g. steroids and calcipetriene) is more effective than either agent alone |
|
|
systemic treatment of psoriasis
|
- this is indicated in patients with severe psoriasis
- options include: immune-modulating therapy - e.g. methotrexate, infliximab, cyclosporine - photochemotherapy - acitretin (a systemic retinoid) - acitretin plus phototherapy - UV light has been shown to be very effective in some patients |
|

Seborrheic keratosis
|
- these are very common skin lesions that begin to appear after the age of 30.
- hereditary- probably autosomal dominant, and are harmless growths with no malignant potential - there is NO association with sunlight - they can be located anywhere, but most commonly on the face and trunk - the increase in number with time and some patients have many of them - they are slightly elevated plaques, gradually turn darker in color and have a "STUCK ON" appearance - treatment is not necessary and is only for cosmetic reasons. Liquid nitrogen cryotherapy or curettage is effective and easily performed |
|
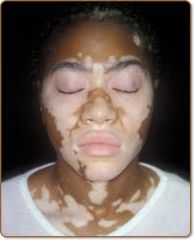
Vitiligo
|
- chronic, depigementing condition due to unknown cause
- hereditary component is suspected - sharply demarcated areas of skin become amelanotic- most common on the face - associated with diabetes mellitus, hypothyroidism, pernicious anemia, and Addison's disease (autoimmune) -topical glucocorticoid and phototherapy are used to promote repigmentation with varying degrees of success |
|
|
Urticaria
|
- aka hives
- caused by the release of of mediators from mast cells, with a resultant increase in vascular permeability - can be precipitated by foods, drugs, latex allergy, animal dander, pollen, dust, plants, and infection, or cold/heat. It can also be idiopathic |
|
|
urticaria findings and treatment
|
- edematous wheals (hives) that are fleeting nature i.e. they disappear within hours only to return in another location. They blanch with pressure and may cause intense pruritus or stinging. Lesions get worse with scratching.
- treatment involves the removal of the offending agent. Antihistamines are effective for symptomatic relief. Systemic corticosteroids may help in more severe cases |
|
|
Angioedema
|
- the mechanism is similar to that in urticaria, though angioedema occurs deeper in the skin (i.e. fluid extravasation occurs in deeper layers of skin/subQ tissue)
- angioedema and urticaria can occur simultaneously or independently - angioedema can be caused by any of the precipitants of urticaria. ACE inhibitors are a specific cause (reaction occurs within 1 week of initiating drug) - unlike urticaria, which can occur anywhere, angioedema effects the eyelids, lips and tongue, genitalia, hands or feet |
|
|
clinical features of angioedema
|

localized edema of the subQ tissue, resulting in non-pitting, puffy skin with firm sweeling that is more tender and burning than pruritic (because there are fewer mast cells/sensory nerve endings in deeper tissues)
- severe angioedema can be LIFE-THREATENING by causing airway obstruction - it can involve the GI tract, causing n/v and abd pain (can mimic acute abd) |
|
|
treatment of angioedema
|
- Give subQ epi for laryngeal edema or bronchospasm
|
|
|
Drug allergy vs adverse reaction to drug
|
- an adverse drug reaction is not necessarily an allergic drug reaction.
- adverse drug reactions include side effects, drug-drug interactions, drug toxicity and associated illnesses and drug allergy. Only 10% of drug adverse reactions are true allergies - many patients who state they are "allergic" to a medication believe this because they have been incorrectly labelled as such without immunologic evidence. - however, given the serious risks of true drug allergy, one should avoid the medication |
|
|
Drug allergy- type of hypersensitivity
|
All four types of hypersensitivity reactions severe as the underlying mechanism of drug allergies.
- in many causes, however the mechanism is unknown |
|
|
What drugs account for more than 80% of all drug allergies
|
Beta-lactam antibiotics (penicillins), aspirin, NSAIDs, and sulfa drugs
- other causes include: insulin, local anesthetics, ACE inhibitors, and radiocontrast agents |
|
|
Clinical features of drug-induced hypersensitivity reactions
|
- dermatologic eruptions (most common) - e.g. urticaria or angioedema, allergic contact dermatitis, EM-like eruptions, erythema nodosum
- pulmonary findings (e.g. asthma, pneumonitis) - renal manifestations (e.g. interstitial nephritis, nephrotic syndrome) - hematologic manifestations (thrombocytopenia, hemolytic anemia, eosinophilia, agranulocytosis) |
|
|
Treatment of possible drug allergies
|
- inquire about any recent changes in the patient's medications. Allergic reactions typically appear within 1 month of initiating the drug.
- it is uncommon for a drug reaction to occur within less than 1 week of initiating a drug - Treatment- discontinue the drug (if known). give antihistamines from symptomatic relief. Treat as for anaphylaxis if severe |
|
|
Food allergies
|
- can be due to true food allergies, food poisoning, metabolic conditions (e.g. lactose intolerance, phenylketonuria), malabsorption syndromes (celiac disease) or pre-existing illnesses (e.g. ulcer)
- as with drug allergies, people generally tend to believe they are allergic to food based on an adverse reaction, even when they may not have a true food allergy - hypersensitivity reactions to foods are usually due to IgE mediated reactions to food and/or additives |
|
|
What are the most common foods that people have allergies to?
|
eggs, peanuts, milk, soy, tree nuts, shellfish, wheat, chocolate, legumes, and some fruits (e.g. kiwi).
- there are others and preservatives or additives may be responsible |
|
|
Clinical features of food allergies
|
- dermatologic manifestations (most common)- e.g. pruritus, erythema, urticaria, angioedema
- GI manifestations (second most-common) - e.g. n/v, abdominal pain, diarrhea - anaphylactic reactions - can affect the respiratory system and can be fatal - cutaneous manifestations (e.g. angioedema, urticaria) |
|
|
Treatment for food allergies
|
- mild reactions- supportive, with administration of antihistamines to lessen the symptoms
- if the reaction is more severe, treat as for anaphylaxis. - avoid the offending agent |
|
|
Insect sting allergy
|
- insects responsible include yellow jackets, honeybees, wasps, and yellow and bald-faced hornets
- local (nonallergic) reaction is localized swelling, pain, pruritus, and redness, all of which subside in several hours. This is the NORMAL reaction to an insect sting - large local (allergic) reaction is marked swelling and erythema over a large area around the sting site. Can be confused with cellulitis. It may last for several days, and sometimes present with mild, systemic manifestations (malaise and nausea) |
|
|
treatment of insect sting allergies
|
- prescribe antihistamines and analgesics for symptoms (should course of prednisone for severe cases)
- anaphylaxis may occur and can be fatal - treatment: ice and oral antihistamines for mild local reactions. If severe, treat as for anaphylaxis |
|
|
Anaphylaxis
|
- most severe form of allergy
- this is a systemic allergic reaction -- usually a type I IgE reaction that may be life-threatening - It occurs within seconds to minutes after exposure to antigen. Numerous causes have been identified, including foods (most common cause), medications, radio-contrast agents, blood products, venoms (e.g. from snakes), insect stings, latex, hormones, ragweed/molds, and various chemicals |
|
|
clinical course of anaphylaxis
|
- it can progress within seconds to minutes to a life-threatening situation characterized by shock or respiratory compromise (airway obstruction, vascular collapse)
- typically, the initial findings are cutaneous, followed by respiratory symptoms |
|
|
Treatment of anaphylaxis
|
- ABCs- secure the airway- intubate if necessary
- give epinepherine immediately. Give IV if severe (1:10,000), subQ if less severe (1:1,000) - give antihistamines (both H1 and H2 blockers) and corticosteroids as well (although they have minimal effect in a hyperacute condition) - supportive care (IV fluids, oxygen) |
|
|
Clinical features of anaphylaxis
|
- cutaneous findings- pruritus, erythema, urticaria, angioedema
- respiratory findings- dyspnea, respiratory distress, asphyxia - CV findings- hypotension, shock, arrhythmias, - GI findings- abd pain, n/v, severe diarrhea |

