![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
Tumors of the Small Intestine |
1. Account for only 3-6% of GI Tumors 2. Most frequent benign: Adenoma and smooth muscle tumor 3. Malignant tumors are rare w/ adenocarcinomas and carcinoids having equal incidence |
|
|
Hyperplastic Polyps |
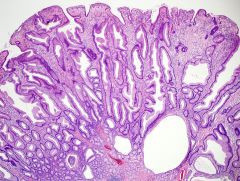
1. Represents 90% of all epithelial polyps and found in over half of all persons > 60 years of age 2. Composed of well-formed glands and crypts lined by crowded epithelial cells giving a serrated or saw-tooth look |
|
|
Juvenile Polyps |
1. Most occur in children < 5 years of age 2. Nearly 80% seen in the rectum (may prolapse and bleed) 3. Large lesions (1 to 3cm in diameter) - Composed of mystically dilated glands in an inflammatory lamina propria 4. May present during defecation |
|
|
Peutz-Jegher Syndrome |

1. Rare Autosomal Dominant disorder 2. Multiple polyps scattered throughout GI (most common-small intestine) 3. Hyperpigmentation of the oral mucosa, lips, face, and genitalia 4. Increased risk of developing carcinoma of breast, pancreas, lung, ovary and uterus |
|
|
Adenomas |
1. Neoplastic lesions ranging in size from small pedunculated polyps to large sessile lesions 2. Prevalence: 20-30% before 40, 40-50% after age 60 3. Three subtypes: -Tubular Adenoma -Villous Adenoma - Tubulovillous Adenoma 4. All arise as a result of epithelial proliferative dysplasia |
|
|
Adenomas: Malignant Risk |
1. Correlated with polyp size, histologic architecture, severity of dysplasia 2. Rare in tubular adenomas < 1cm in diameter 3. High in sessile villous adenomas > 4cm in diameter 4. Severe dysplasia, when present, often found in villous areas |
|
|
Tubular Adenoma |

1. Most (90%) found in the colon and about half in the rectosigmoid 2. Stalk composed of fibrovascular core covered by normal mucosa 3. Raspberry-like head composed of neoplastic epithelium, forming branching glands lined by cells w/ tall, hyper chromatic nuclei |
|
|
Villous Adenoma |
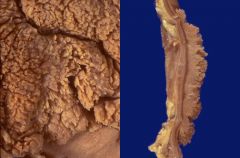
1. Propensity for the rectum and rectosigmoid 2. Large (up to 10cm), sessile, velvety, or cauliflower-like lesions 3. Finger-like papillae covered by dysplastic epithelium 4. May present w/ rectal bleeding or rarely hypokalemia |
|
|
Familial Adenomatous Polyposis (FAP) |

1. Autosomal Dominant disorder characterized by 100s to 1000s of adenomatous colonic polyps - Defect of APC gene on chromosome 5q21 2. Most are tubular adenomas 3. Treatment: Prophylactic colectomy 4. Most patients develop carcinoma by 40 years of age |
|
|
Gardner Syndrome |
1. Variation of FAP w/ fibromatosis , epithelial cysts, & osteomas 2. Osteomas: mandible, skull and long bones in particular 3. Autosomal dominant w/ high risk of developing colon cancer |
|
|
Turcot Syndrome |
1. FAP with CNS tumors (medulloblastoma and glial tumors) 2. Medulloblastoma seen in 2/3 of patients |
|
|
Colorectal Carcinoma |
1. Carcinoma arising from colonic or rectal mucosa 2. Third most common site of cancer and third most common cause of cancer-related death 3. Peak Incidence: 60-79 years of age 4. Risk Factors: Obesity and physical inactivity ** "Apple Core" Lesion |
|
|
Colorectal Carcinoma: Molecular Pathway |

1. Most common: Adenoma-carcinoma sequence 2. Second pathway is Microsatellite instability (MSI) |
|
|
Colorectal Carcinoma: Dietary Factors |
1. Excess energy intake relative to requirement 2. Low content of non-absorbable vegetable fiber 3. High contact of refined carbohydrates 4. Intake of red meat 5. Decreased intake of protective micronutrients |
|
|
Colorectal Carcinoma: Distribution |
1. Cecum/ascending colon-38%, Sigmoid colon-35%, Other-27% 2. Proximal colon tumors grow as polypoid masses 3. Distal colon tumors tend to annular, encircling lesions that reproduce so called napkin-ring constrictions of the bowel |
|
|
Colorectal Carcinoma: Right Sided |
1. Right-sided lesions present with fatigue, weakness, iron deficiency anemia, and vague pain 2. Grows as a raised lesion |
|
|
Colorectal Carcinoma: Left-Sided |
1. Left Sided Lesions present with changes in bowel habits (decreased stool caliber), crampy left lower quadrant discomfort, and blood streaked stool 2. More infiltrative so poorer prognosis than right sided *Spread via direct invasion into adjacent structures and metastasis via lymphatics and blood vessels* Spread to lymph nodes, liver, lungs, bones, etc. |
|
|
Colorectal Carcinoma: Increased risk for.. |
1. Streptococcus Bovis Endocarditis |
|
|
Colorectal Carcinoma: Serum tumor marker |
CEA; useful for assessing treatment response and detecting recurrence *Not useful for screening* |
|
|
Carcinoid Tumors |
1. Malignant proliferation of neuroendocrine cells; low-grade malignancy - Tumors cells contain neurosecretory granules positive for chromogranin |
|
|
Carcinoid Tumors: Morphology |
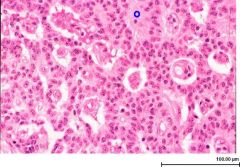
1. Solid, yellow-tan appearance on transection 2. Monotonous w/ scant, pink granular cytoplasm & round-to-oval stippled nuclei |
|
|
Carcinoid Tumor: most common locations |
1. Appendix and small bowel |
|
|
Carcinoid Tumor: Secretory Products |
1. Usually Serotonin (5-HT) w/ elevated levels of its metabolite, 5-HIAA (found in urine) 2. Presents with flushing of face, cyanosis, diarrhea, cramps, nausea, vomiting, etc. 3. May have hepatomegaly and cardiac involvement 4. Elevated levels of 5-HT and 5-HIAA in the blood & urine w/ hepatic metastasis |
|
|
Gastrointestinal Lymphoma |
1. GI most common site other lymph nodes 2. No evidence of liver, spleen, or bone marrow involvement at time of diagnosis 3. Sporadic lymphomas arise from the B cells of gut mucosa-associated lymphoid tissue (MALT) - MALT lymphomas seen in adults t(11:18) |
|
|
Mesenchymal Tumors |
1. Most are of smooth muscle origin and asymptomatic 2. Grouped as GI stromal tumors 3. Gastric lesions may exhibit peptic ulcers like symptoms, particularly bleeding 4. Intestinal lesions may produce bleeding or rarely intussusception 5. Lesions are usually resectable |

