![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
What are the members of Enterobacteriaceae?
|
E Coli*
ETEC EPEC EHEC EIEC Shigella dysenteriae Shigella flexneri Shigella boydii Shigella Sonnei Salmonella enterica Salmonella typhi Other (klebsiella/enterobacter/Yersinia) *Can be found in normal flora *Most common |
|
|
What are the properties of Enterobacteriaceae?
|
Large
Cocci-bacillus to bacillus Gram (-) Grow rapidly in aerobic/anaerobic conditions |
|
|
What type of disease do Enterobacteriaceae produce?
2 groups 5 and 3 diseases |
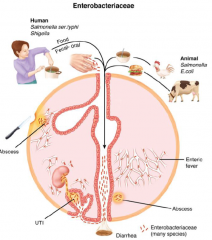
A. Opportunistic Infection in normally sterile environments listed below:
1. UTI 2. Wounds 3. Soft Tissue infection 4. Pneumonia 5. Meningitis B. Diarrhea - of 3 types 1 - Dysentry - Inflammatory diarrhea with WBCs, &/or blood in stool. Caused by invasive & cytotoxic strains 2 - Watery Diarrhea - Dominated by fluid loss. Caused by enterotoxins. 3 - Enteric Fever - Febrile, the GI tract is simply the port of entry for a systemic disease. |
|
|
What are the 3 types of diarrhea and what are their mechanisms of pathology?
|
1 - Dysentry - Inflammatory diarrhea with WBCs, &/or blood in stool. Caused by invasive & cytotoxic strains
2 - Watery Diarrhea - Dominated by fluid loss. Caused by enterotoxins. 3 - Enteric Fever - Febrile, the GI tract is simply the port of entry for a systemic disease. (may be constipated or 1/3 have mild diarrhea) |
|
|
What are the antigenic structures of Enterobacteriaceae?
|
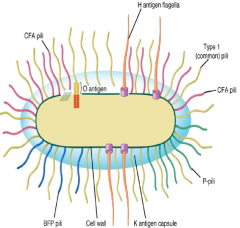
O - cell wall LPS (outer membrane)
K - Surface polysacchraride (capsule/amorphous slime) H - Flagellar protein (pertrichous arrangement) Pilli - are antigenic but not part of a formal typing scheme. General: Type 1 bind to mannose (common) Specialized: CFA binds enterocytes, BFP binds enterocytes, & P binds uroepithelium |
|
|
What does it mean if the serotype has a K?
|
It is capsulated.
|
|
|
Why is it important to know the 3 antigenic structures of Enterobacteriaceae?
|
Allows for further serotyping. In the case of E Coli where some strains are benign, being able to serotype allows isolation of the pathogenic strain.
|
|
|
What toxins are produced by E Coli (all strains)?
What type of toxin are they? |
Alpha hemolysisin - pore forming (cell death)
Shiga toxin (Stx) - AB toxin that blocks ribosome 60s (cell death) Labile toxin (LT) - AB toxin that increases cAMP (enterotoxin) Stable toxin (ST) - AB toxin that increases cGMP (enterotoxin) |
|
|
Who produces LT & ST?
What is MOA of the enterotoxins, LT, & ST? |
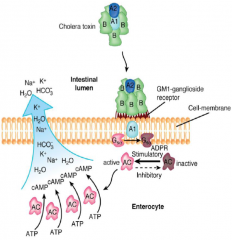
Similar to cholera toxin. Found in ETEC
LT - AB toxin that A catalyzes ADPR rxn of Gs to activate cAMP formation. Result is secretion Cl & lack absorption Na. (watery diarrhea) ST - Same MOA except with cGMP. Decrease cotransport NaCl into cell. |
|
|
What is function of Alpha Hemolysin?
What are the names of the analogues in other species? (5 total) |
Pore forming - aggressive pathogens (Staph Aureas, GAS, E Coli)
Staph aureas - secretes Alpha Toxin GAS - Streptolysin O Streptoccocus Pneumoniae - Pneumolysin Listeria Monocytogenes - listeriolysin O (LLO) |
|
|
What are the 4 classifications of E Coli? How are they divided?
|
ETEC - enterotoxigenic
EPEC/EAEC - enteropathogenic/enteroaggregative EIEC - enteroinvasive EHEC - enterohemorrhagic They are classified by their virulence patterns. |
|
|
What type of diarrhea do each of the 4 E Coli cause?
Where do they each bind & and do they invade? |
ETEC - adhere jejunum/ileum - watery diarrhea (travelers diarrhea)
EPEC/EAEC - adhere ileum - watery diarrhea (infant diarrhea) EIEC - adhere colon & invade! - dysentery + WBC (mild) EHEC - adhere colon - dysentery ***Only EIEC invades |
|
|
What is the relationship between site of binding and quality of diarrhea?
|
A relationship exists between the site of adherence and the quality of the diarrhea
Large intestine/distal small intestine - Inflammatory/bloody diarrhea Small intestine - non inflammatory/watery diarrhea |
|
|
How does ETEC bind to GI and MOA disease?
|
ETEC: adherence to microvilli mediated by CFA (colonizing factor antigen) class of pili required for effective toxin delivery to target gut cells; genes encoding ST, LT, CFA on plasmids
|
|
|
What is the MOA of EPEC?
|
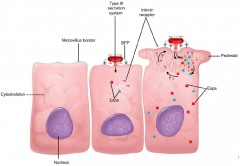
EPEC: Attach/Effacement lesion in ILLEUM (PAI). Attaches to enterrocyte w/ BFP (bundle forming pili). Colony forms on enterrocyte surface. Type 3 secretion injects Esps (exporting secretion proteins) which includes intimin. Intimin facilitates tight binding, other esps form the pedestal. Result is malabsorption.
|
|
|
Where would one generally get Vibrio Cholera?
|
contaminated water in the setting of poor sanitation (Indian subcontinent and Africa- endemic); can be found in inadequately cooked crab and shrimp
|
|
|
What is a major cause of death for EHEC?
|
10% hemolytic uremic (HUS) syndrome (5% mortality)
A/E lesions – secretion Stx production – hemolytic uremic syndrome (HUS) |
|
|
What is the MOA of EHEC?
|
A distinguishing feature: produces both Stx (Shigatoxin) AND A/E lesions. Do NOT invade.
Attach/Effacement lesion in COLON (PAI). Attaches to enterrocyte w/ BFP (bundle forming pili). Colony forms on enterrocyte surface. Type 3 secretion injects Esps (exporting secretion proteins) which includes intimin. Intimin facilitates tight binding, other esps form the pedestal. Result is malabsorption. Secretes AB Stx which causes inflammation & bleeding (dysentery). When Stx/LPS become bacteremic then they can cause HUS & kidney damage (swelling/clogged w/ fibrin/platelets) |
|
|
What is HUS?
|
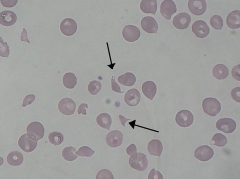
Triad of
1-hemolytic anemia 2-Acute kidney failure 3-thrombocytopenia 90% cases are from E. Coli Fragmented RBC is a Schistocyte. |
|
|
Where would one generally get Salmonella typhi?
|
strictly human disease; reservoir is chronic human carrier (Typhoid Mary); transmission is fecal-oral when carriers contaminate food/water
|
|
|
Time course of Salmonella induced Typhoid Fever
|
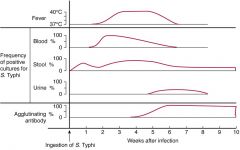
Insidious onset and can last for weeks if left untreated the fever is predominate feature – stepwise
•Bacteremia starts disease –Bowel reseeded (diarrhea 1-2x if at all) –Other organs •Hemorrhage and perforations gradually resolves (if humoral Ab and activated macs can clear infection) or death due to rupture of intestine (occurs necrotic Peyer’s patches l ileum) or spleen rupture & death |
|
|
Progression Salmonella Typhi into person?
|
1. bacteria bind M cells using Capsular Vi and get delivered to Peyer’s patches (ILLEUM). Uses ruffles to bind/enter
2. S. Typhi invades macrophages and multiplies in membrane-bound vacuole that fails to fuse with host's organelles & macrophage dies 3. survival in phagocytes is due to inhibition of oxidative burst 4. Multiplication occurs and spread through lymphatic system, spleen, liver & bone marrow. Eventually bacteremia occurs to and LPS endotoxin 5. Fever onset and bacteremia can spread to biliary tree reinfecting the GI tract (2 week cycles) and ERS system |
|
|
Where would one generally get Salmonella enterica?
|
animal reservoir (poultry, exotic pets like turtles, raw milk); mishandling of food allows transfer to humans; chronic carriers who are food handlers.
picnics, restaurants, potato salad, turkey dressing |
|
|
Progression of Salmonella Enterica into a person?
|
Surface adhesins react with host to rearrange actin to form ruffles leading to pinocytosis and type 3 injection of effector protein into enterocytes of lg/sm bowel, transcytose through basolateral membrane into lamina propria causing profound inflammation
|
|
|
How does EIEC bind to GI?
|
Identical to Shigella except:
higher infecting dose More mild symptoms Adheres to COLON M cells -> invades mucosa causing inflammation, ulceration, abcess formation ->Secretion Stx causing fever, inflammation, bleeding |
|
|
What are the 2 virulence factors of cholera?
|
TCP - toxin coregulated pilus
CT - an AB toxin that ADPR GM1-ganglioside receptors. A1 then enters and turns on cAMP formation to cause hypersecretion CL, K, HCO3, H2O |
|
|
What is Febrile Dysentery syndrome?
|
Fever in addition to triad of cramps, tenesmus (painful straining to pass stool), and frequent, small-volume, bloody, mucoid discharge
|
|
|
What are symptoms of UTI? Where can it be located?
What are the SE of UTIs? |
Frequent urination that are of painful burning quality.
cystitis - bladder - self limiting but risk bacteremia pyelonephritis - kidney - additional sx are fever, malaise, flank pain. Again risk bacteremia UTI and UPEC are the most common cause gram (-) sepsis & shock |
|
|
What is the significance of the P and type 1 pilli?
How does it produce injury? |
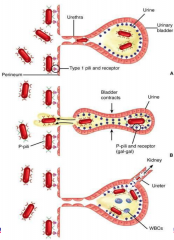
Strain specific E Coli (UPEC - uropathic E Coli)
Type 1 pilli - important for periurethral adherence P Pilli - important for binding uroepithelium and resisting flushing effect with urination. (These ONLY bind to uroepithelium) >90% UTI are E Coli! They secreted alpha hemolysin causes injury. May lead to LPS endotoxin (septic shock) and bacteremia |
|
|
What are steps of E Coli UTI infection, using virulence factors?
|
UPEC - Uropathic E Coli
Minor trauma/mechanical (sex/catheters/obstruction) -> E coli gain access to urethra via the type 1 and P pilli. Type 1 pilli aid in initial colonization but P pilli are required to resist flushing -> May ascend up to kidney and become bacteremic. Gram negative toxic shock may occur. |
|
|
How are each of the E coli Variants acquired and Who gets infected?
|
ETEC - travelers & indigenous infants (<2yo) get from contaminated food/water. T is for travelers & toddlers.
EPEC - Bottle fed infants (<1yo) get from asx parents or infant cases. P is for pampers EHEC - Industrialized derived from cattle. Outbreaks assoc w/ unpast. juice/veg & hamburger. Has low infecting dose to allow human2human transmission. Ironic the hamburger kids meal has juice? EIEC - <5yo in developing nations. Humans are only reservoir so human2human transmission is a must. (Almost identical to shigella)EIEC |
|
|
How is the Shigella species differentiated?
Which is most severe, least, common? |
Differentiated by the O antigen (no H/flagella)
In order worse to most mild (DFBS) A – S. dysenteriae Type 1 Shiga bacillus B – S. flexneri C – S. boydii D – S. sonnei S. dysenteriae, type 1 most severe infection (largest production Stx) most often found underdeveloped tropical S. Sonnei may be watery diarrhea S. Flexneri & S. Sonnei are most common |
|
|
How is Shigella acquired and Who gets infected?
|
In undeveloped nations (esp tropical) person-to-person (no animal reservoir) with poor sanitary conditions or by contaminated food/water (fecal-oral)
Also, wars, natural disasters, toddlers |
|
|
Who produces STx?
What is the MOA? |
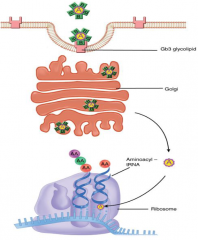
Most shigella and some E Coli produce this A/B toxin
AB toxin - B binds Gb3 to cause formation endocytic vacuole formation. Crosses the trans-golgi and modifies 60s ribosome to prevent primed tRNA from binding. |
|
|
What is the MOA of Shigella moving into the cells? Cause of cell death?
|
Acid resistant to reach COLON. Invades M cells & phagocytes and induce apoptosis. Now invade enterocytes via type 3 secretion of invasins which aid in attachment, actin reorganization & endocytosis. Now in enterocytes use actin to transport via "comet" -> now invades adjacent cells in finger like projections that will pinch off (rarely becomes bacteremic) -> Produces Stx.
In this adjacent manner causes ulcers/bleeding in COLON which decreases absorption leading to dysentery. Cell death partially occurs via Stx which inhibits the 60s. |
|
|
Is Stx required for Shigella to cause disease?
|
No, but it does contribute to severity
|
|
|
What is the clinical presentation of Shigella?
|
Begins as watery diarrhea but becomes intense colitis with triad of sx: frequent, small volume dysentery & cramping & tenesmus (and fever)
May cause HUS Triad is termed febrile dysentery syndrome Tenesumus is pain with straining to pass stools |
|
|
How are Shigella and Salmonella Typhi common and different in invasion of M cells?
|

|
|
|
How is E Coli diagnosed?
|
Issue is virulent compared to benign strains (commonly found)
Isolated in culture, the most virulent O157:H7 serotype fails to ferment sorbitol. Sorbitol negative colonies are verified by O157:H7 antisera. |
|
|
How is Salmonella diagnosed?
|
Cultured from blood or stool. (same medium as shigella)
Enteric fever is MOST likely to give a positive blood culture |
|
|
What is the infecting dose in Salmonella compared to shigella? What implications does this have on transmission route?
|
Shigella = 200 organisms
Salmonella = 10K organisms Shigella is human2human and salmonella is animal to human or human2human (typhi). General rule is infecting dose must be less for human2human spread. |
|
|
What are the "other" Enterobacteriaceae? Which is most virulent and what type of infection do they cause?
|
Klebsiella, Enterobacter, Yersinia Pestis causes mostly oppurtuinistic infections.
Klebsiella most virulent, (rarely) causes classical lobar pneumonia (like other encapsulated bacteria). Enterobacter - less virulent then klebsiella, outbreak assoc. w/ parenteral fluid casuing a mixed infection |

