![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
Acne 1. Pathogenesis 2. Describe the different classifications |
1. Increased sensitivity of pilosebaceous unit to circulating androgens -> follicular plugs of sebum and keratin 2. Noninflammatory – open and closed comedonesInflammatory – pustules, red papules, nodules and cysts Resolving – macules or scars |
|
|
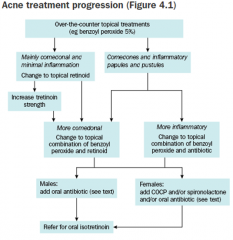
How is acne treated? |
1.Mild Benzoyl peroxide 5 % creams or gels (bleaches fabrics) - If poor response and mainly commedonal add topical retinoid) (eg tretinoincream, adapalene) - If inflammatory papules and pustules as well ascomedones, add topical antibiotic (benzoyl peroxide + clindamycingel) 2.Moderate to severe acne Oral therapy should be started with either topical retinoid or topical combination a) Oral antibiotics - Doxycycline 50 – 100mg OD for 6 weeks b) COPC – takes approx 3 months to work, so give 6month trial c) Spironolactone 25 - 100mg OD 3.Severe, cystic or scarring acne Oral isotrenitoin |
|
|
ETG flowchart |
|
|
|
What is: - a macule - a patch - a papule - maculopapular - a nodule - a plaque |
Macule: Circumscribed area of altered skin colour < 1cm diameter
Patch: Circumscribed area of altered skin colour > 1cm diameter Papule: palpable mass on skin surface <0.5cm Maulopapulae: a raised and discoloured circumscribed lesion Nodule: palpable mass on skin surface >0.5cm Plaque: flat topped palpable mass >1cm diameter |
|
|
What is a:
- wheal - angioedema - vesicle - bulla - pustule - abscess - furuncle - carbuncle |
Wheal: a pale, compressible area of dermal oedema
Angioedema: a diffuse area of oedema extending into subcutaneous tissue Vesicle: fluid filled blister < 0.5cm diameter Bulla: vesicle >0.5cm diameter Pustule: visible collection of pus in skin <1cm Abscess: localised collection of pus in a cavity >1cm Furuncle: a purulent infected hair follicle. Includes folliculitis (small funruncles) and boils (larger furuncles) Carbuncle: A cluster of boils discharging through several openings |
|
|
What is - purpura - Petechiae - ecchymosis - haematoma - telengectasiae - comedo (blackhead, whitehead) |
Purpura: bleeding into skin
Petechiae: purpuric lesions 2mm or less in diameter Ecchymosis: Larger purpuric lesions Haematoma: swelling from any gross bleeding Telengectasiae: visible dilatation of small cutaneous blood vessels Comedo: a plug of keratin and sebum in a dilated pilosebaceous gland - Blackead: open comedo - Whitehead: closed comedo |
|

Due to intolerance to the gliadin fraction of gluten (90% also have enteropathy). |
Ans: dermatitis herpetiformis Diagnosis requires biopsy. |
|

shiny, flat topped firm papules most often found on wrist, lower back and ankles. Can also be found in oral cavity, vulva and penis. |
Ans: lichen planus Longstanding erosive forms can rarely evolve into SCC. Biopsy is often recommended to confirm diagnosis. Treatment is not always necessary. Options include topical steroids, topical retinoids and intralesional steroid injection. |
|

A boggy lump, usually on the scalp, secondary to drammatic immune response to a fungal infection. |
Ans: kerion Rx: oral antifungals +/- PO Abs if infected |
|
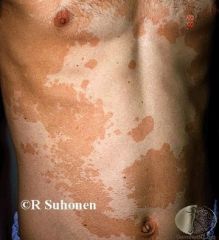
A common yeast infection of the skin |
Ans: Pityriasis versicolour Rx: topical antifungals, oral fluconazole if ineffective |
|
|
Psoriasis: 1. what is it? 2. where is it found? 3. What is the treatment? 4. What are the associated health disorders? |
1. an inflammatory and hyperplastic condition of theskin, characterised by erythema and scale.
2. Commonsites - elbows, knees, sacrum and scalp. Can also affect trunk and limbs, palms and soles,nails, flexures (including genitals) and face. 3a) avoid triggers - stress, sunburn, medication etc b) GP level rx: Tar, steroids, calcipitriol (combos eg ar/steroids, calcipitriol/steroids) c) more complex: methotrexate, UV therapy, cyclosporin, biologic therapy etc d) IBD, inflammatory arthritis, uveitis, cardiovascular disease/metabolic syndrome |
|

What am I? |
Typical plaque psoriasis? |
|

Numeours droplet shaped lesions, often a response to Group A strep infection |
Guttate psoriasis. Common on trunk and proximal limbs. Often responds well to milder corticosteroids. |
|
|
Psoriasis treatment: an overview of primary care management |
Topicalcorticosteroids (anti-inflammatoryand antimitotic).
Tars (anti-inflammatoryand antipruritic) - eg LPC 6% + salicylic acid 3%, icthammol - often used mane with corticosteroids nocte - often need to be made at compounding pharmacy
Calcipotriol (regulatesproliferation and differentiation of keratinocytes) Usually always combined with topical corticosteroid therapy |
|
|
Dermatitis Treatment |
1. Treat dry skin - emollients, oil in baths etc 2. Decrease irritants - avoid soaps, wool, overheating etc 3. Corticosteroids applied liberally OD until skin is clear Mild/face/axilla/groin: Hydrocortisone 1% for one week If fails try methylprdnisolone aceponate 0.1% (Advantan) Mod/Trunk/Limbs: Triamcinolone acetonide (Aristocort) 0.02% ointment OD Severe or in flexures: methylprdnisolone aceponate 0.1% OD (Advantan) mometasonefuorate (elocon) 0.1% OD FINGERS, LICHENIFIED WRISTS OR ANKLES, FEET Betamethasone diproprionate (diprosone) 0.05% Batamethasone valerate (betnovate) 0.1%Mometasone fuorate 0.1% (elocon) |
|

What Am I? A Common, relapsing form of eczema mainly affecting scalp and face |
Seborrhoiec dermatitis Treatment: topical antifungal + topical corticosteroid |
|

What am I? A form of eczema affected hands and fingers characterised by vesicles |
Ans: Pompholyx Eczema. Avoid irritants and use strong steroids to treat. |
|

What am I? |
Discoid eczema |
|

What am I? |
Tinea - a skin infection with a ringworm fungus. Defined by definite edge and central clearing Rx - initially topical terbinafine |

