![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
Which layer of skin acts as the primary barrier to absorption?
|
Stratum Corneum
Not all body sites are equally permeable. Variation in sratum corneum thickness can effect absorption. |
|
|
Is absorption faster or slower in cutaneous appendages (e.g. hair follicles, sebaceous glands, eccrine glands and apocrine glands)?
|
FASTER. Areas rich in these appendages will have enhanced absorption.
|
|
|
How does hydration play a role in percutaneous drug absorption?
|
Hydration expands the skin surface area and will therefore enhance absorption.
|
|
|
Order the following from most absorbing to least absorbing regions of skin:
Nail Scrotum Trunk/Extremities Face/Scalp Palm/Sole |
Main point is that not all regions are equal and this should be kept in mind when using dermal patches.
Nail<<Palm/sole<trunk/extremities<face/scalp<<Scrotum |
|
|
What is Fick's Law of Diffusion? Which variable is the only variable can we control?
|
Fick’s law of diffusion J=KpC ; J= rate of absn
Kp = permeability constant C= the concentration of the drug in the vehicle. the only variable we can control is **concentration**!!! |
|
|
What characteristics could give percutaneous drugs more absorotion?
|
small molecular size, small molecular weight, more lipid solubility = greater absorption.
|
|
|
Transdermal delivery provides a controlled rate of delivery, reduces fluctuations in levels and bypasses 1st pass metabolism. What is the downfall of transdermal delivery?
|
Absorption may vary widely
|
|
|
Does the vehicle greatly impact efficacy of the drug?
|
YES- It ties potency to efficacy.
|
|
|
What are some things that can increase the likelihood of drug interactions?
|
POLYPHARMACY (as in elderly, HIV/AIDs), Organ failure, lack of hepatic/renal perfusion (e.g., CHF, third spacing, dehydration) all can increase likelihood of interactions.
|
|
|
How might genetics contribute to variability in drug reactions among patients?
|
**Genetic polymorphisms** may contribute to variability in reactions - for example (FYI) slow acetylators are at higher risk of lupus-like symptoms with hydralazine, procainamide, isoniazid
|
|
|
d
|
d
|
|
|
When evaluating a patient that may have a drug induced skin disease, what questions should you ask the patient?
|
a. Description of lesion
b. Med history c. Chronology of administration d. Previous Hx of drug sensitivity? e. Consider Excipients (e.g dyes, binders, etc. ) Also, Examine rash, describe, record as ADR with details (consider FDA MedWatch reporting) |
|
|
What type of patients are most at risk for Drug induced skin disease?
|
Altered Immune Status
Organ Impairment (renal, hepatic) Genetic Factors (Slow acetylaters) Atopy (maybe, esp in pts with asthma, eczema) |
|
|
Chronology of Administration:
i. Initial dosing related to onset of rash ii. Withdrawal - stop the drug! iii. Rechallenge - not in severe type of reactions |
Chronology of Administration:
i. Initial dosing related to onset of rash*** ii. Withdrawal - stop the drug! iii. Rechallenge - not in severe type of reactions |
|
|
The following 5 classes of drugs might cause adverse skin reactions, but it is very rare and you can often cross these off your list of differentials. What are some possible reasons why these DON'T cause reactions? (don’t memorize, but be able to use common sense- Babos)
Antacids Antihistamines Hormones Steroids Vitamins |
i. Antacids - locally acting (e.g., Mg(OH)2 OR antihistamine (e.g., H2 blockers)
ii. Antihistamines - d/t blocking histamine iii. Hormones: insulin, OC, thyroid - endogenous substances iv. Steroids - endogenous, used to TREAT rxns v. Vitamins, Fe (needed to survive) (niacin can cause PG mediated flushing - prevent with ASA) |
|
|
What type of drug related eruption has a 7-14 onset, starts centrally and spreads outward, and is themost common type?
|
Exanthematous Drug Eruptions
|
|
|
What type of infection may worsen an Exanthematous Drug Eruption?
|
Viral infections may worsen
FYI: Amp- and Amoxicillin not used in mononucleosis |
|
|
How do you treat an Exanthematous Drug Eruption?
|
Less serious reaction, so less intensive Tx
1. Antihistamine 2. Topical steroid 3. Topical antipruritic |
|
|
What are the 5 common causes of Exanthematous Drug Eruptions?
|
1. Allopurinol (Boards: causes MANY types of rash, most seriously SJS/TEN - educate pts to report rash immediately)
2. Antibiotics 3. Carbamazepine 4. Sulfonamide moiety: thiazides, loop diuretics, sulfa antibiotics. (Boards: celecoxib, sulfonylurea insulin secretogogues , dapsone) 5. Gold salts |
|
|
What type of drug related eruption has an onset of 36 hours, is usually hard to distinguish, and is the 2nd most common type of eruption?
|
Urticaria
|
|
|
What type of drug eruption is caused by increased permeability leading to fluid leakage that causes selling of the tongue, lips, eyelids, or genetalia?
|
Angioedema
Treatment - systemic treatment needed 1. Resuscitation if needed (relatively rare) 2. Oral antihistamine 3. Oral corticosteroid if needed |
|
|
What are the most common causes of Angioedema?
|
1. **ACEI** !!!→↑bradykinin levels
2. NSAIDS→↓COX activity→↑leukotriene production 3. Contrast media → mast cell degranulation 4. Monoclonal antibodies (e.g, infliximab, muromonab, abciximab) |
|
|
What type of eruption is characterized by a 7-10 day onset (duration may be lengthy), raised pupuric lesions on the legs, fever, utricaria, arthralgia, lymphadenopathy, maculopapular rash, & ↑PMNs near vasculature?
|
Vasculitis
|
|
|
How do you treat vasculitis?
|
Treatment: systemic corticosteroids and/or NSAIDs (if not NSAID induced, of course)
|
|
|
What drugs can cause vasculitis?
|
1. Allopurinol
2. Antibiotics 3. Carbamazepine 4. NSAIDs 5. Sulfonamide moiety 6. Gold salts 7. Propylthiouracil |
|
|
Exfoliative dermatitis is a severe type of reaction that is characterized by exfoliation, fever, lymphadenopathy, edema.
What are come common causes of Exfoliative dermatitis? How do you treat it? |
Causes
1. Penicillins 2. Isoniazid (? More likely in slow acetylators) 3. Gold salts 4. Phenytoin 5. Sulfonamides Treatment- antipyretics and fluids |
|
|
Stevens-Johnson and Toxic epidermal necrolysis (TEN) are EMERGENCIES and occur 1-3 weeks post exposure. Mortality can be high so proper treatment is imperative. How do you treat these?
|
Treatment - give it your all! Corticosteroids, fluids, immunosuppressives, IVIG, etc.
|
|
|
What are some common causes of SJS and TEN?
|
1. Allopurinol
2. Anti TB drugs (isoniazid) 3. Antiepileptics (Barbiturates, carbamazepine, lamotrigine, phenytoin) 4. Gold 5. Sulfonamides 6. Tetracyclines |
|
|
< 10% epidermal detachment = _____
more severe = _______ Choose SJS or TEN |
< 10% epidermal detachment = SJS
more severe = TEN |
|
|
3 Common causes of Erythema Multiforme?
How do you treat it? |
1. PCN
2. Barbiturates 3. NSAIDs Tx: stop drug, systemic steroids?, watch for progression |
|
|
Fixed drug eruptions - not a high morbidity/mortality, caused by numerous agents (Allopurinol is always a good guess…)
|
Fixed drug eruptions - not a high morbidity/mortality, caused by numerous agents (Allopurinol is always a good guess…)
|
|
|
What are the most common causes of Angioedema?
|
1. **ACEI** !!!→↑bradykinin levels
2. NSAIDS→↓COX activity→↑leukotriene production 3. Contrast media → mast cell degranulation 4. Monoclonal antibodies (e.g, infliximab, muromonab, abciximab) |
|
|
What type of eruption is characterized by a 7-10 day onset (duration may be lengthy), raised pupuric lesions on the legs, fever, utricaria, arthralgia, lymphadenopathy, maculopapular rash, & ↑PMNs near vasculature?
|
Vasculitis
|
|
|
How do you treat vasculitis?
|
Treatment: systemic corticosteroids and/or NSAIDs (if not NSAID induced, of course)
|
|
|
What drugs can cause vasculitis?
|
1. Allopurinol
2. Antibiotics 3. Carbamazepine 4. NSAIDs 5. Sulfonamide moiety 6. Gold salts 7. Propylthiouracil |
|
|
Exfoliative dermatitis is a severe type of reaction that is characterized by exfoliation, fever, lymphadenopathy, edema.
What are come common causes of Exfoliative dermatitis? How do you treat it? |
Causes
1. Penicillins 2. Isoniazid (? More likely in slow acetylators) 3. Gold salts 4. Phenytoin 5. Sulfonamides Treatment- antipyretics and fluids |
|
|
Stevens-Johnson and Toxic epidermal necrolysis (TEN) are EMERGENCIES and occur 1-3 weeks post exposure. Mortality can be high so proper treatment is imperative. How do you treat these?
|
Treatment - give it your all! Corticosteroids, fluids, immunosuppressives, IVIG, etc.
|
|
|
What are some common causes of SJS and TEN?
|
1. Allopurinol
2. Anti TB drugs (isoniazid) 3. Antiepileptics (Barbiturates, carbamazepine, lamotrigine, phenytoin) 4. Gold 5. Sulfonamides 6. Tetracyclines |
|
|
< 10% epidermal detachment = _____
more severe = _______ Choose SJS or TEN |
< 10% epidermal detachment = SJS
more severe = TEN |
|
|
3 Common causes of Erythema Multiforme?
How do you treat it? |
1. PCN
2. Barbiturates 3. NSAIDs Tx: stop drug, systemic steroids?, watch for progression |
|
|
Fixed drug eruptions - not a high morbidity/mortality, caused by numerous agents (Allopurinol is always a good guess…)
|
Fixed drug eruptions - not a high morbidity/mortality, caused by numerous agents (Allopurinol is always a good guess…)
|
|
|
What type of drug induced skin reaction is more common in drugs with aromatic ring structures/unsaturation?
|
PHOTOSENSITIVITY
- electron cloud absorbs UV radiation |
|
|
What 4 classes of drugs commonly cause photosensitivity?
|
i. Sulfonamide moiety
ii. Tetracyclines iii. Fluoroquinolones iv. Phenothiazines |
|
|
What are the most common causes of Angioedema?
|
1. **ACEI** !!!Most common→↑bradykinin levels (don't re-challenge the pt)
2. NSAIDS→↓COX activity→↑leukotriene production 3. Contrast media → mast cell degranulation 4. Monoclonal antibodies (e.g, infliximab, muromonab, abciximab) |
|
|
What type of eruption is characterized by a 7-10 day onset (duration may be lengthy), raised pupuric lesions on the legs, fever, utricaria, arthralgia, lymphadenopathy, maculopapular rash, & ↑PMNs near vasculature?
|
Vasculitis
|
|
|
How do you treat vasculitis?
|
Treatment: systemic corticosteroids and/or NSAIDs (if not NSAID induced, of course)
|
|
|
What drugs can cause vasculitis?
|
1. Allopurinol
2. Antibiotics 3. Carbamazepine 4. NSAIDs 5. Sulfonamide moiety 6. Gold salts 7. Propylthiouracil |
|
|
Exfoliative dermatitis is a severe type of reaction that is characterized by exfoliation, fever, lymphadenopathy, edema.
What are come common causes of Exfoliative dermatitis? How do you treat it? |
Causes
1. Penicillins 2. Isoniazid (? More likely in slow acetylators) 3. Gold salts 4. Phenytoin 5. Sulfonamides Treatment- antipyretics and fluids |
|
|
Stevens-Johnson and Toxic epidermal necrolysis (TEN) are EMERGENCIES and occur 1-3 weeks post exposure. Mortality can be high so proper treatment is imperative. How do you treat these?
|
Treatment - give it your all! Corticosteroids, fluids, immunosuppressives, IVIG, etc.
|
|
|
What are some common causes of SJS and TEN?
|
1. Allopurinol
2. Anti TB drugs (isoniazid) 3. Antiepileptics (Barbiturates, carbamazepine, lamotrigine, phenytoin) 4. Gold 5. Sulfonamides 6. Tetracyclines |
|
|
< 10% epidermal detachment = _____
more severe = _______ Choose SJS or TEN |
< 10% epidermal detachment = SJS
more severe = TEN |
|
|
3 Common causes of Erythema Multiforme?
How do you treat it? |
1. PCN
2. Barbiturates 3. NSAIDs Tx: stop drug, systemic steroids?, watch for progression |
|
|
Fixed drug eruptions - not a high morbidity/mortality, caused by numerous agents (Allopurinol is always a good guess…)
|
Fixed drug eruptions - not a high morbidity/mortality, caused by numerous agents (Allopurinol is always a good guess…)
These are solitary, sometimes multiple well demarcated lesions, can develop blisters in the center. Color varies. Appropriate to orally challenge to confirm is appropriate. |
|
|
Take home points for DI Skin disease
|
recognize severity; think about mechanism to help remember (e.g., angioedema, which drugs aren’t likely to cause eruptions, etc), for TEN/SJS: allopurinol, sulfonamide moiety drugs, isoniazid, tetracyclines are always good board guesses. Drug induced SLE is a likely board question, too. PTU causes ↑ANCA in up to 50% of patients, so remembering this cause of vasculitis might be a good idea. DON”T MEMORIZE THIS CHART or lists of drugs, but get a feel for which drugs are likely culprits, and keep your eye on the biggies, especially any you see emphasized in your board reviews.
|
|
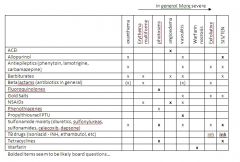
Don't memorize, good for reference and boards
|
Don't memorize, good for reference and boards
|
|
|
What type of skin reaction occurs commonly with drugs that have an aromatic ring/unsaturation?
|
Photosensitivity
- electron cloud absorbs UV radiation |
|
|
What drugs commonly case photosensitivity?
|
i. Sulfonamide moiety
ii. Tetracyclines iii. Fluoroquinolones iv. Phenothiazines |
|
|
What drug induces skin necrosis and causes "purple toe"?
|
Warfarin induces skin necrosis = “purple toe” - Boards: mechanism: Factors II, VII, IX, and X and Proteins C and S require reduced vitamin K to be activated; when vitamin K epoxide reductase is inhibited by warfarin, proteins C and S do not get activated; persons with deficiencies of C and/or S will get CLOTTING and subsequent necrosis when warfarin is initiated
|
|
|
BOARDS
What drugs can cause Systemic Lupus Erythematosus-like syndrome (SLE)? |
1. Drugs that undergo N-acetylation, more common in slow acetylators
2. Isoniazid, hydralazine, procainamide |

