![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
166 Cards in this Set
- Front
- Back
|
What is the major findings of a posterior dislocated shoulder on frontal plain film of the shoulder |
-internal rotation |
|
|
What is another name for a trough sign
|
reverse hills sachs
|
|
|
What does a reverse hills sachs sign look like
|
a linear impaction deformity of the anterior medial humeral head
|
|
|
What will you see on a Y-view of the humerus in a patient with a posterior shoulder dislocation
|
the humeral head will be seated posteior to the glenoid
|
|
|
What is the rim sign
|
apparent increase in space between the anterior rim of the glenoid fossa and the medial aspect of the humeral head. This is termed the "positive rim sign." It may be present in posterior dislocation because the normal glenoid fossa faces as much anteriorly as it does laterally. Since the dislocated humeral head rests against the posterior glenoid rim, the space between the anterior rim and the humeral head appears increased.
|
|
|
What is the abscent cresent sign (of posterior shoulder dislocation)
|
Absent crescent sign: seperation of the humeral head and the glenoid such that the normal overlap is lost
|
|
|
Why are posterior shoulder dislocations commonly missed
|
Because there is usually not significant medial, lateral, superior, or inferior displacement, 50% of posterior dislocations are initially missed if only AP radiographs obtained
|
|
|
What are the 2 MCC of posterior shoulder dislocations
|
Because there is usually not significant medial, lateral, superior, or inferior displacement, 50% of posterior dislocations are initially missed if only AP radiographs obtained
|
|
|
What are 4 signs of a posterior dislocation on a AP view of the shoulder
|
Trough sign: vertical compression fx of anteromedial humeral head
Rim sign: widening of glenohumeral joint > 6 mm Absent crescent sign: separation of humerus from glenoid such that normal overlap is lost Humerus fixed in internal rotation |
|
|
Why would a CT be indicated in a posterior shoulder dislocation
|
CT: evaluate complications such as reverse Hill Sachs or reverse Bankart, stripping of posterior periosteum, tear of posterior labrum
|
|
|
If an AP of the shoulder is obtained and you still suspect a posterior dislocation, what is the next step
|
If suspected, get transscapular Y view (axillary view OK, but painful and may dislocate a spontaneously relocated shoulder)
Humeral head lies posterior to glenoid, center of the “Y” |
|
|
Where is the location of a hills sachs deformity from an anterior dislocation
|
posteriorly lateral
|
|
|
What is the orientation of the femoral heads in a posterior hip dislocation
|
posterior and superior with internal rotation
|
|
|
What is the most common cause of a posterior hip dislocation
|
MVA
|
|
|
What percent of posterior hip dislocations will have an associated
|
posterior wall or acetabular fx
|
|
|
What are the potential complications of a posterior hip dislocation
|
sciatic nerve injury (10%), AVN of femoral head, myositis ossificans, DJD, occasional femoral head fx
|
|
|
Where does the femoral head lie following a posterior hip dislocation
|
Femoral head comes to lie superolateral to acetabulum
(correct) |
|
|
What is the reason to order a CT following a posterior dislocation of the hip
|
evaluate for loose bodies in joint (if present, requires operative tx)
|
|
|
When is the blade of grass sign seen
|
this is seen in pagets disease
|
|
|
What is a common appearance of the blade of grass sign
|
V-shaped lucency in metaphysis of femur from the lytic phase of Paget disease.
|
|
|
Where are the 2 most common locations of pagets diseasee
|
tibia and femur
|
|
|
What is the lytic phase of pagets called when it is in the skull and what part of the skull is most common
|
In skull, lytic defect = osteoporosis circumscripta, most often seen in the frontal bone
|
|
|
Is the lytic phase hot on bone scan
|
yes
|
|
|
can there be a combination of lytic and blastic
|
yes
|
|
|
Do you see coarse trabecuale and cortical thickening in the sclerotic phase of pagets
|
yes
|
|
|
What are some complications of pagets
|
bowing, fx, sarcomatous degeneration (rare)
|
|
|
What is the appearance of the blastic phase of pagets disease when it affects the skull called
|
cotton wool
|
|
|
Will you see the mixed phase of Paget disease of the pelvis with extensive involvement by Paget disease with areas of cortical (iliopectineal and ilioischial lines, arrows) and trabecular (arrowheads) thickening throughout the pelvis
|
yes
|
|
|
True or false; coxa vara of the hip may occur in pagets
|
true
|
|
|
What type of hip deformity looks like a hand grip for a gun
|
coxa vara (smaller angle)
|
|
|
can pagets diseaes form a picture frame or ivory appearance of the vetebral bodies
|
yes
|
|
|
What is the ddx of an ivory vertabrae
|
Blastic mets (prostate, breast)
Infection (TB) Lymphoma Paget disease |
|
|
If you see a coxa vara deformity of the hip with lateral bowing what should be suspected
|
pagets
|
|
|
What are the findings of the hands in a patient with sleroderma
|
acroosteolysis
subcutaneous Ca or joint Ca erosions (late) flexion contractures |
|
|
What erosive feature with subluxation is very suspcicious for scleroderma
|
Very distinctive feature is severe resorption of 1st carpometacarpal joint with radial subluxation of the 1st metacarpal
|
|
|
acroosteolysis ddx
|
PBL Really F=== Sucks Hairy Dick |
|
|
What conditions can cause calcification of the hands and acroosteolysis |
Burns, Scleroderma and hyperparathyroidism all cause calcification and acroosteolysis |
|
|
What causes the salt and pepper appearance of the skull
|
HPTH
|
|
|
Salt and pepper = HPTH
Coton wool and osteoporosis circumscipta=pagets |
yes
|
|
|
Salt and pepper skull
Rugger jersey spine Brown tumor subchondral sclerosis of the distal clavicles |
HPTH
|
|
|
What are the findings of the hand in a patient with HPTH
|
Subperiosteal resorption along radial aspects of middle phalanges, especially 2nd and 3rd |
|
|
Can a patient with HPTH have increased calcification of the hands
|
yes (and also acroosteolysis)
|
|
|
Can HPTH cause diffuse osteosclerosis or osteoporosis
|
yes
|
|
|
When is diffuse vascular calcifications seen
|
Vascular Ca+: usually w/secondary hyperparathyroidism from renal failure
|
|
|
What is a joint finding that may be seen in a patient with renal failure and HPTH
|
Amyloidosis can be seen in pts undergoing dialysis, leading to findings in joints and spine that can appear similar to infection |
|
|
If a dialysis patient has large erosive changes to the hip what should be suspected
|
erosive changes secondary to amyloid deposition
|
|
|
Do patients with renal failure have either osteoslerosis or osteopenia
|
yes
|
|
|
what is the appearance of tumoral calcinosis
|
multifocal, large, amorphous calcific deposits (seen in patients on dialsys with HPTH)
|
|
|
What syndrome is associated with primary HPTH
|
MEN 1 |
|
|
What is a looser fx
|
Considered to be a type of insufficiency fracture.
|
|
|
What is looser fx sometimes called
|
pseudofx
|
|
|
When are looser fx seen
|
Osteomalacia
Chronic renal disease Fibrous dysplasia Hyperthyroidism Paget's disease Renal osteodystrophy X linked hypophosphataemia |
|
|
What is the ddx of distal clavicle resorption
|
RA, hyperparathyroidism, trauma (osteolysis), cleidocranial dysplasia, mets/myeloma
|
|
|
What is the ddx of bilateral distal clavicle resorption
|
RA, hyperparathyroidism, cleidocranial dysplasia
|
|
|
What is cleinocranial dysplasia
|
Delayed ossification of midline structures formed through intramembraneous ossification |
|
|
What are the imaging findings of cleinocranial dysplasia
|
Clavicles: Absent, hypoplastic or loss of central 1/3 |
|
|
Should you get a hand Xray if you see distal clavicle resorption
|
yes (RA and HPTH)
|
|
|
What is a rugger jersey spine
|
Sclerosis of vertebral body endplates
|
|
|
What should rugger jersey spine be differentiated from
|
Differentiate from osteopetrosis (“bone in a bone” or sandwich vertebrae) and Paget (“picture frame,” enlarged vertebrae)
|
|
|
What is erosive OA
|
Inflammatory form of OA that affects postmenopausal middle-aged women |
|
|
What age and sex is most commonly affected by erosive OA
|
post menopausal middle-aged women
|
|
|
What joints of the hand are commonly affected by erosive OA
|
PIP and DIP, and 1st carpometacarpal and STT joints
|
|
|
Can erosive OA effect the PIP and DIP
|
yes
|
|
|
What carpometacarpal joint is most commonly affected in erosive OA
|
1st |
|
|
What is the classic appearance of the erosions of erosive OA
|
seagull appearance
|
|
|
What causes the wings of the seagul
|
osteophytes at the margins
|
|
|
Can ankylosis occur in severe erosive OA
|
yes, ankylosis of IP joints is a feature which does not occur in routine OA but can occur
|
|
|
Is errosive OA associated with osteopenia
|
yes
|
|
|
What soft tissue features is sometimes seein in patients with erosive OA
|
osteopenia
|
|
|
Do patients with erosive OA sometimes go on to develop rheumatoid arthritis
|
yes, 15% of patients will eventually have rhematoid arthritis
|
|
|
What are some features of regular osteoarthritis
|
joint space narrowing
sclerosis osteophytes (PIP,DIP and 1st MCP joint) |
|
|
Do patients with psoariatic arthritis sometimes have periosteal rxn
|
yes, and this is not seen in erosive arthritis
|
|
|
If psoariatic arthritis is severe enough can it lead to athritis mutilans
|
yes
|
|
|
What type of arthrits may eventually lead to a pencil in cup deformity of the distal phalanx
|
psoaritic
|
|
|
What is a major difference between the arthritis of the erosive arthritis and psoariatic
|
psoriatic arthritis will have a wisp of periostitis surrounding erosions
|
|
|
What joint spaces are predominately affected in psoriatic arthritis
|
DIP (erosive OA is DIP and PIP)
|
|
|
Can ankylosing occur in late stages of psoriatic arthritis |
yes (correct prior slide bc anklyosing doesnt typically occur in erosive OA) |
|
|
What is a classic soft tissue finding in a patient with psoriatic arthritis
|
sausage fingers
|
|
|
How does the bone density in psoriatic arthritis compare to erosive arthritis
|
osteopenia is more diffuse in erossive arthritis where as in psoriatic it will be juxtaarticular
|
|
|
Can acroosteolytisis occur in psoriasis
|
yes
|
|
|
What is the general rule for reactive arthritis and psoriatic arthritis
|
they are very similar but reactive will favor the feet and psoriatic the hands
|
|
|
What are the important clinical findings of reactive arthritis
|
Urethritis (85%)
Conjunctivitis (60%) Arthritis (> 60%) Young adults, M:F > 5:1 |
|
|
If there is erosive arthritis in one hand what should be suspected
|
infectious etiology
|
|
|
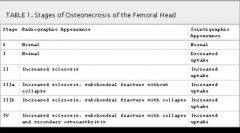
What are the stages of AVN of the hip
|
|
|
|
What are the findings of the nuclear scan during stage 1 of AVN of the hip
|
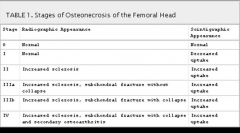
increased uptake
|
|
|
What are the nuclear scan findings of stage 2 and up for AVN of the hip
|
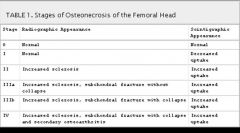
increased uptake (stage 1 is decreased) |
|
|
What is the difference between stage 3a and 3b
|
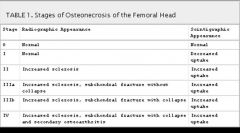
subchondral collapse
|
|
|
What stage do you start to see osteoarthritic changes of the hip
|
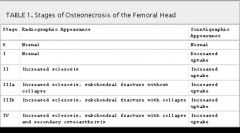
stage 4
|
|
|
What is the mitchel classification
|
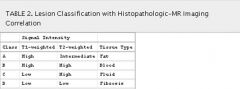
this is a classification of AVN of the hip for MR |
|
|
What are the categories of the mitchel classification
|
A-D
|
|
|
What is the best way to remember the mitchel classification
|
remember the evolution of tissue and then infer the signals for T1 and T2 |
|
|
Is the mitchel classification similar to the modic for the spin
|
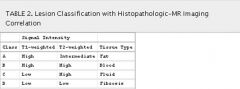
no (that is fluid fat then fibrosis)
|
|
|
What stage of AVN of the hip will you see decreased uptake on nuclear scan
|
stage 1 (no radiographic findings)
|
|
|
What is the ddx of AVN of the hip
7 |
trauma
medication (steroids) sickle cell anemia alcoholism barotrauma (Caisson disease), Gaucher disease radiation therapy idiopathic |
|
|
What is the most sensitive modality for detecting AVN of the hip
|
MR
|
|
|
What is seen in the acute phase of AVN on MR
|
bone marrow edema (which doesnt make sense according to the mitchel classification
|
|
|
What is a classic sign of AVN that is often seen later on MR of the hip
|
Later, “double line sign” in anterosuperior femoral head
|
|
|
What does the double line sign look like on T1 and T2
|
irregular/serpentine rim of low signal on T1, and paired high and low signal on T2
|
|
|
What causes the paired high and low signal that is seen on T2 (double line sign of AVN)
|
(inner granulation tissue, outer fibrous tissue and cellular debris)
|
|
|
What are the classic findings of psoariatic or reactive arthritis of the sacroiliac joints
|
Asymmetric sacroiliitis and bulky syndesmophytes suggest either psoriatic or reactive arthritis
|
|
|
What is the appearance of the sacroilititis that is associated with IBD and AS
|
sacroiliitis tends to be more symmetric, syndesmophytes are delicate and involve the annulus fibrosis, mostly anterior location
|
|
|
What are some features that help distinguise reactive arthritis from psoriatic arthritis
|
primarily young men, favors feet, plantar or Achilles enthesopathies, retrocalcaneal bursitis or calcaneal erosion
|
|
|
What are some features that help differentiate psoriatic from reactive arthritis
|
psoriatic favors hands, tends to be more severe and mutilating
|
|
|
What are features that are common to both psoriatic and reactive arthritis
|
: fluffy erosions, periostitis (mixed erosive and productive), mostly normal bone density
|
|
|
What type of Sacroilitis will have thin flowing syndesmophytes
|
AS or IBD
|
|
|
What age and sex will AS predominately effect
|
young males
|
|
|
What is the direction of spread of AS
|
Lumbosacral spine to the C-spine
|
|
|
What causes the bamboo spine appearance on AP plain film of AS
|
“bamboo spine” from extensive syndesmophyte formation |
|
|
What causes the trolley track sign of AS on AP plain film
|
“trolley track sign” (3 parallel white lines, ossification of interspinous ligament and apophyseal joint capsules)
|
|
|
What is the cause of the dagger sign that is seen on AP plain film
|
ossified interspinous ligament
|
|
|
What happens to the pelvic tilt in patients with severe AS
|
abnormal angle of pelvic inlet (pelvic tilt) from loss of lumbar lordosis
|
|
|
What is a romanus lesion of AS seen on lateral plain film
|
this is osteitis and is also known as shiny corners
|
|
|
After romanus lesions (shiny corner sign) are seen on lateral plain film what is the next change that you will expect to see
|
squaring of the vetebral bodies bc of loss of the normal anterior concavity from erosion of the corners
|
|
|
What are the classic distinguishing features of ABC
|
cystic
expansile fluid fluid level |
|
|
What age group are ABCs typically seen
|
under 30
|
|
|
Describe the typical zone of transition for a ABC
|
narrow zone of transition
|
|
|
How is an ABC differentiated from a simple bone cyst
|
it is usually cortically based which is different from an SBC which is medullary based
|
|
|
Where are the most common locations for ABC
3 |
metaphysis of long bones
pelvis posterior element of the spine |
|
|
What do 50% of ABCs arise from
|
another lesion (GCT, NOF, Chondroblastoma, Osteoblastoma, Trauma)
|
|
|
What is the DDX of a ABC in a long bone
|
SBC
NOF Fibrous dysplasia |
|
|
What is the DDX of a lytic lesion in the posterior element
|
GO APE
GCT Osteoblastoma ABC Plasmacytoma EG |
|
|
What is the tx of an ABC
|
curettage and possible cryosurgery, low dose radiation |
|
|
What is the characteristic appearance of an ABC on CT/MR
|
Characteristic feature is fluid/fluid levels from hemorrhage
|
|
|
When you see expansile cystic lesion on CT or MR what must be ruled out
|
telangiectatic osteosarcoma
|
|
|
What is a telangiectatic osteosarcoma
|
Osteosarcoma variant without any bone matrix, and often without periosteal reaction
|
|
|
What are some plain film findings that can help to differentiate an ABC from telangiectatic osteosarcoma
|
at least a portion of the margin has a wide zone of transition, usually cortical destruction and soft tissue mass
|
|
|
What is the combination of findings if a patient has the unhappy triad
|
Combination of ACL tear, MCL tear, posterior horn of medial meniscus tear
|
|
|
What is the cause of the unhappy triad
|
planted foot is hit from the lateral side at the level of the knee resulting in Valgus stress
|
|
|
Does the ACL attach to the tibia on the medial or lateral aspect
|

medial (lateral for the femur)
|
|
|
Where is the bone bruise seen in patients with ACL tear
|
Bone bruise involving lateral tibial plateau, lateral femoral condyle (kissing contusions)
|
|
|
What is the ddx of a hip effusion in a child
6 |
septic arthritis
toxic synovitis LCP (hip) hemophilia JRA trauma |
|
|
What are subtle findings that may be seen in a pediatric patient with a septic hip
|
cartilage loss and indistinct cortex
|
|
|
Do all pediatric hip effusions get tapped
|
yes, Any effusion must be tapped to r/o septic joint, which can rapidly destroy a joint
|
|
|
What is LCP of the hip
|
disease is a childhood condition associated with an inadequate blood supply to part of the hip joint results in AVN. Without adequate blood flow, a process can occur in which the bone becomes unstable, and may break easily and heal poorly. |
|
|
What age group is typically affected by transient synovitis of the hip
|
Develop limp over few days, often h/o recent viral illness
|
|
|
What is the typical clinical presentaton of transient synovitis of the hip
|
Develop limp over few days, often h/o recent viral illness
|
|
|
What is the X-ray finding of a pt with transient synovitis of the hip
|
usually shows effusion, regional osteoporosis
|
|
|
How doe MR help to differentiate transient synovitis of the hip from septic joints
|
septic joints often have altered bone marrow signal (femoral head or juxta-articular), whereas transient synovitis does not |
|
|
Are sacral insufficiency fxs commonly seen on plain film
|
no, very difficult to see.
|
|
|
If a sacral insufficiency fracture is seen on plain film what is the common appearance
|
Subtle increased sclerosis with vertical orientation, or smudging of trabeculae |
|
|
What is the classic appearance of bilateral sacral insufficiency fx on nuclear scans
|
the honda sign
|
|
|
Hip arthroplasty
|

The femoral component has a several millimeter wide lucency surrounding most of it. The acetabular component has subsided superiorly by approximately 1.5 cm, with lateral displacement, and also has several fractured screws.
|
|
|
Hip Arthroplasty
|

The patient has had two reconstruction plates placed, one anterior (the lower one) and one posterior, in an attempt at reconstruction of the acetabulum. There is superior subsidence and lateral displacement of the right acetabular component with fracture of several screws and a very wide lateral opening angle. |
|
|
What is the criterial for hardware loosening
|
Lucent zone > 2 mm at cement-metal or metal-bone interfaces (some say > 1 mm) |
|
|
What are some findings of hardware loosening
|
Lucent zone > 2 mm at cement-metal or metal-bone interfaces (some say > 1 mm) |
|
|
What is particle disease
|
Osteolysis (lytic lesion) due to granulomatous reaction by body to particles of cement, metal, silastic, bone, or polyethylene which shear off hardware |
|
|
Can particle disease lead to hardware loosening
|
yes
|
|
|
cementless left total hip arthroplasty
|

|
|
|
Migration of femoral component
|

eccentric femoral component from polyethylene wear. If there was adjacent lytic lesion it would probably be from particle disease
|
|
|
What are 3 causes of prosthetic loosening
|
natural wear and tear
particle disease infection |
|
|
How do you diagnose infection of a prosthesis
|
tap it
|
|
|
What are some clues that loosening of hardware may be the result of infection
|
Rapidly developing wide cement-bone lucent zone in 1st postop year
Endosteal scalloping and periosteal reaction On arthrogram, irregular contour to joint capsule and filling of cavities, sinus tracts, and abscesses |
|
|
What should be the first thing that comes to mind when you see an aggresive pediatric lesion
|
ewings sarcoma
|
|
|
What is the general radiographic pattern of a ewings sarcoma
|
moth eaten or permiative
|
|
|
Do ewings sarcoma have a wide or narrow zone of transition
|
narrow zone
|
|
|
Describe the periosteal reaction of a ewings sarcoma
|
Aggressive periosteal reaction (onion skinning, sunburst, Codman triangle)
|
|
|
Do ewings sarcomas often have an associated ST mass
|
yes
|
|
|
What is the ddx of an aggressive appearing pediatric lesion
|
Ewing sarcoma, osteosarcoma, EG, infection > lymphoma/leukemia, mets (neuroblastoma, rhabdomyosarcoma), PNET
|
|
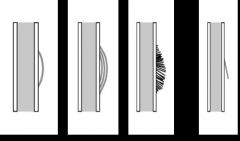
Periosteal rxn
|
Solid periosteal, onion skining (lamellated), sunburst (hair on end), codman triangle.
|
|
|
What dol does ewings sarcoma tend to occur
|
first 2 decades
|
|
|
What are the clinical SS of a ewings sarcoma
|
pain
swelling fever increased ESR |
|
|
What 5 locations do ewings sarcoma tend to occur
|
diaphyseal or metadiaphyseal in long bones, but also in pelvis, scapula, sacrum
|
|
|
Can ewings sarcoma occur in the pelvis, sacrum and scapula
|
yes
|
|
|
Are ewings sarcomas central or eccentric
|
tend to be central
|
|
|
Describe an osteosarcoma
|
Mostly permeative, without a matrix, but can be partly sclerotic (resembling osteosarcoma) or patchy
|
|
|
What is the MC malignant bone tumor in a young person
|
osteosarcoma
|

