![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
134 Cards in this Set
- Front
- Back
|
What is the normal platelets and acceptable levels for patients prior to IR procedurs
|
Platelet count: 150,000-450,000/uL (> 50,000/uL sufficient for procedures)
|
|
|
What are the normal PT/INR and acceptable levels for patients prior to IR procedurs
|
PT (INR): 11-14 s (0.9-1.1) (PT < 1.5x midpoint of nl range sufficient for procedures)
|
|
|
What is the normal level of PTT
|
Activated PTT: 25-35 s
|
|
|
When should Antiplatelet agents (ASA, Plavix) be stopped
|
5-7d
|
|
|
When should lovenox be stopped
|
12-24h
|
|
|
When should heparin be stopped
|
less than 6 h
|
|
|
When should coumadin be stopped
|
7 days
|
|
|
How much FFP is needed to reverse an INR of 2.5
|
in general, 2 units FFP will reverse INR 2.5
|
|
|
How are platelets usually dosed
|
often dosed as 4-6 units (random donors) or as one single donor unit
|
|
|
What is the dosage of protamine to reverse heparin
|
: 50 mg slow IV push dose will reverse common intraprocedural doses of heparin (3,000-5,000 IU
|
|
|
What is given to reverse INR
|
vit k and FFP
|
|
|
Should INR be measured in all patients with on warfarin or liver disease
|
yes
|
|
|
When is PTT definitely measured
|
pts recieving heparin
|
|
|
What procedures have a low risk of bleeding
|
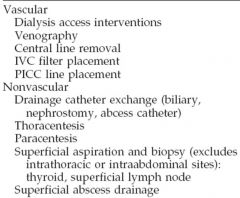
|
|
|
What procedures have a high risk of bleeding
|
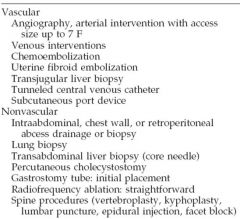
|
|
|
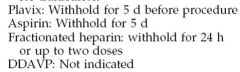
What are the major differences in high risk bleeding pts meds and labs
|
INR threshold is <1.5 (2 in low risk)
plavix should be withheld in high risk |
|
|
What procedures have a significant risk of bleeding
|
|
|
|
What should be known about anticoagulation meds for significant risk of bleeding
|
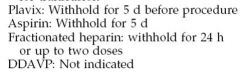
|
|
|
What is the only categories of risk of bleeding that aspirin is held
|
significant
|
|
|
What is the general rule of thumb for injection rate into an artery
|
the diameter of the artery
|
|
|
What is the general rule for filming rate
|
the larger the vessel the faster the filming rate
|
|
|
What is the injection and filming rates for various blood vessels
|
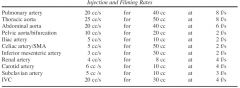
|
|
|
What vessels tend to get fast film rates
|
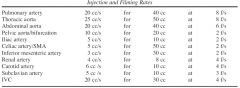
aorta, pulm art, renal artery, carotid artery, IVC
|
|
|
General diameters of various vessels
|
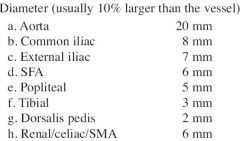
|
|
|
General diameters of various vessels
|
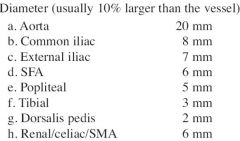
|
|
|
What 2 types of vasodilators are used and what are the doses
|
Nitroglycerin: 100 ug doses
Papaverine: 30-60 mg/h IA |
|
|
What type of vasoconstrictor is used and what is the dose
|
Vasopressin: 0.1-0.4 U/min
|
|
|
What 3 analgesics are used and what are the doses
|
Morphine: 1 mg bolus, 1 mg maintenance
Versed (midazolam): 1 mg bolus, 1 mg maintenance Fentanyl: 50 ug bolus, 50 ug maintenance |
|
|
What are the drugs used for reversal
2 |
Naloxone (opioid antagonist): 1 mg IV
Flumazenil (benzodiazepine antagonist): 0.2 mg IV |
|
|
What is the most common cause of an aortic pseudoaneurysm
|
deceleration injury from MVA
|
|
|
What are the 3 MC sites for traumatic pseuodaneurysm
|
MC at ligamentum arteriosum, next MC aortic root and diaphragm level
|
|
|
What are 6 cxr findings of traumatic pseudoaneurysms
|
Wide mediastinum
Indistinct arch contour Filling in of AP window Depressed L main stem bronchus Rightward shift of trachea or NG tube Left apical cap Left pleural effusion Upper rib fxs |
|
|
Where is the AP window
|
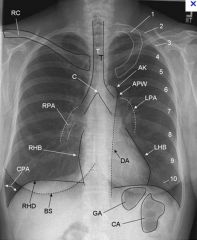
|
|
|
What does digital subraction imaging look like
|

case of brachiocephalic artery injury
|
|
|
What is a common cause of intramural hematoma
|
Usually elderly hypertensive pt
|
|
|
Can a intramural hematoma progress to a dissection
|
yes
|
|
|
What is an intramural hematoma
|
Thought to represent a rupture of vasa vasorum resulting in hematoma within aortic media. I have read it could also be a dissection without a entery point seen
|
|
|
What are the indications for TIPS
|
Refractory variceal hemorrhage despite adequate endoscopic treatment
Refractory ascites Hepatic hydrothorax Budd-Chiari |
|
|
What are the absolute contraindications for TIPS
|
Primary prevention of variceal hemorrhage
Congestive heart failure Severe pulmonary hypertension Severe tricuspid regurgitation Active biliary obstruction Sepsis Multiple hepatic cysts or Caroli disease |
|
|
If a pt has severe tricuspid regurgitation should a TIPS procedure be done
|
no
|
|
|
Should a TIPS ever be done for primary prevention of variceal bleeding
|
no
|
|
|
What is the first step in performing a TIPS procedure
|
Preprocedure US, coags checked and corrected, broad spectrum antibiotics
|
|
|
After obtaining venous access through the right jugular what is the next step for TIPS
|
Place small catheter into RHV and obtain wedged HV pressure (= PV pressure)
|
|
|
After venous access and wedge pressure what is the next step
|
Perform venogram: opacify portal vein via wedged contrast injection
(they can also inject CO2 to make a roadmap) |
|
|
What to vessels is the puncture suppose to connect
|
Using direct puncture, create a connection between RHV and RPV and place a wire into the portal system
|
|
|
Once the parenchymal tract is created what is the next step
|
Dilate parenchymal tract with 10 mm balloon angioplasty
|
|
|
What is correct placemtn of the viatorr stent
|
Place Viatorr stent so that one end is within 3 cm of portal bifurcation, and other within 3 cm of IVC
|
|
|
What r 2 things to be sure to do before finishing a TIPS procedur
|
Completion portal venogram, determine postprocedure gradients
|
|
|
What is the appropiate gradient for after TIPS
|
Completion portal venogram, determine postprocedure gradients
|
|
|
What is a Viator Stent
|
Expanded polytetrafluoroethylene (ePTFE)-covered nitinol stent-graft consisting of two parts: a distal 2-cm-long uncovered portion that lies in the portal vein and an inner covered portion (4-8 cm long) for the tract and hepatic side of the TIPS
|
|
|
Does a Viator stent have a covered and uncovered portion
|
yes
|
|
|
What does a viator stent look like
|

the uncovered portion lies in the portal vein
|
|
|
What is the effectiveness of a TIPS
|
TIPS patency is 50% at 1 y, 30% at 2 y
|
|
|
What is the primary assisted patency
|
this is the patency after a procedure
Primary assisted patency 90% at 1 y, 87% at 3 y |
|
|
What percent will have recurrent variceal bleeding
|
Rebleeding in 15% at 6 m, 30% later
|
|
|
Is TIPS effective for treating ascites
|
Cures ascites in 50-75%
|
|
|
Where does most stensosis occur
|
Most stenoses occur at hepatic venous outflow or within stent
|
|
|
What is the survellaince regime for TIPS
|
Requires surveillance with US at 1 day post procedure, 1 m, 3 m intervals in 1st year, 6-12 m subsequent
|
|
|
What are the signs of failure of TIPS on US
|
No flow
Rise or fall > 50 cm/s c/w postprocedure study Peak < 90 cm/s, > 190 cm/s Return of antegrade flow in intrahepatic PVs and reversed flow in draining hepatic vein |
|
|
What are the signs of restenosis on angiograms
|
Gradient > 12
Stenosis > 50% Variceal filling |
|
|
What is the tx of TIPS failure
|
balloon angioplasty +/- additional stent
|
|
|
What does MELD stand for
|
Model for End-Stage Liver Disease
|
|
|
What parameters does a MELD score measure
|
Scoring system for assessing severity of chronic liver disease
Serum bilirubin Serum creatinine INR |
|
|
Why was the MELD score developed
|
Initially developed to predict death within 3 m of surgery in pts undergoing TIPS
|
|
|
When are you considered to have a poor outcome
|
Poor outcomes for MELD > 24
|
|
|
What is the MELD score now used for
|
Also used for prioritizing allocation of liver transplants
|
|
|
What is a penetrating aortic ulcer
|
Ulceration of atherosclerotic plaque into the media
|
|
|
What demographic MC gets penetrating aortic ulcers
|
Usually elderly hypertensive pt w/marked atherosclerotic disease
|
|
|
What a re the CT findings for penetrating aortic ulcers
|
CT: contrast material-filled outpouching in aorta in absence of dissection flap or false lumen, often extensive aortic calcification, frequently assoc w/intramural hematoma
|
|
|
What are 3 potential serious outcomes that may result from a penetrating aortic ulcers
|
May precipitate localized intramedial dissection, may break through into adventitia to form a pseudoaneurysm, or may rupture completely into right or left hemithorax
|
|
|
What is a bovine arch
|
Bovine arch: common origin of brachiocephalic and L CCA
|
|
|
What is a ductus diverticulum
|
Ductus diverticulum: occurs at same place as a tear, but is smooth, has continuous edges with the aorta, no flap and rapid (normal) washout of contrast
|
|
|
How often does an abberant right subclavian vessel occur
|
Ductus diverticulum: occurs at same place as a tear, but is smooth, has continuous edges with the aorta, no flap and rapid (normal) washout of contrast
|
|
|
What is a diverticulum of Kommerel
|
Often arises from a dilated portion called the diverticulum of Kommerell
|
|
|
If the right subclavian branch is aberrant where does it arise
|
it is the last branch off the aorta
|
|
|
is an abberant right subclavian posterior to the trachea
|
yes
|
|
|
Abberant right subclavian
|

|
|
|
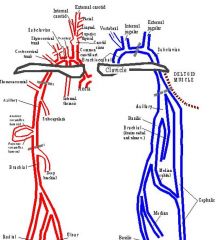
Vessels of the leg
|
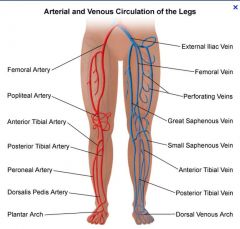
|
|
|
where do most arterial vessel emboli lodge
|
Most macroemboli lodge in femoral or popliteal arteries
|
|
|
What is the MCC of embolus
|
a-fib
|
|
|
What are the findings specific to acute emboli
|
Creates a meniscus
Minimal or no vascular disease No contralateral leg abnormalities Poorly developed collaterals Other emboli elsewhere |
|
|
What are the findings of acute limb ischemia
|
Pain, pulselessness, pallor, paresthesia, paralysis
|
|
|
What are 5 causes of acute limb ischemia
|
native/graft thrombosis, embolism(a-fib), trauma, peripheral aneurysm w/embolus or thrombosis
|
|
|
Is heparin indicated for acute limb ischemai
|
Immediate parenteral anticoagulant therapy (heparin) indicated in all pts with ALI
|
|
|
What are the classes of ischemia
|

|
|
|
What are the treatment guidelines for the classes of limb ischemia
|
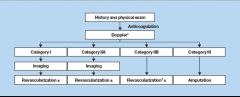
|
|
|
What is the difference in management between 2a and 2b ALI
|
Category I, IIA: catheter-directed thrombolysis +/- percutaneous aspiration/mechanical thrombectomy
Category IIB: immediate revascularization (surgical, endovascular) |
|
|
What are the indications of thrombolysis
|
Acute or subacute (< 2 w) thrombus in native vessels or grafts
Clotted grafts (dialysis) Embolic occlusions (alternative is surgical embolectomy |
|
|
What is the the first step in the procedure for thrombolyisis
|
contralateral femoral access
|
|
|
After obtaining femoral access what is the next step
|
cross the occlusion with a guidewire
|
|
|
Are there cases where you are unable to get the guidewire across
|
yes, and this is a bad prognostic indicator
|
|
|
What type of catheter is used across the occlusion
|
Place multisidehole catheter across occlusion
|
|
|
What is the dosing regime for heparin in a patient undergoing thrombolysis
|
Heparin given before thrombolysis, 5,000 U bolus, then low dose (100 U/hr) during tPA infusion
|
|
|
What is the dosage of TPA
|
2 mg initial bolus tPA, followed by infusion of 0.5-1 mg/h (average total dose 10-20 mg; do not exceed 40 mg)
|
|
|
Where does the patient go after the catheter is placed
|
Pt monitored in ICU, f/u angiogram at 12 h
|
|
|
What is done for lysis of a clot that is not complete
|
When lysis complete or near complete (~24-48 h), tx any remaining stenosis with angioplasty
|
|
|
What happens when the fibrinogen level drops below 150
|
Risk of hemorrhage increases when fibrinogen level drops below 100-150 mg/dL
|
|
|
What is fibrinogen
|
Fibrinogen (factor I) is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulatio
|
|
|
What are the complications of thrombolysis
|
Bleeding (10%)
Distal embolization of clot (advance infusion catheter to level of distal clot) Revascularization syndrome: necrotic tissue revascularized and lactic acid/myoglobin released |
|
|
What is revascularization syndrome
|
: necrotic tissue revascularized and lactic acid/myoglobin released
|
|
|
What are the absolute contraindications to thrombolysis
|
Absolute: active internal bleeding, irreversible limb ischemia, recent stroke, brain tumor, left heart thrombus
|
|
|
What are the relative contraindications to thrombolysis
|
Relative: h/o GI bleeding, major surgery within 10 d, diabetic hemorrhagic retinopathy, coagulopathy, embolus of cardiac source
|
|
|
Are the result good when trying to open up a long segment femoropoptieal occlusion with tpa
|
no, For long segment fem-pop occlusions, percutaneous tx results not good
|
|
|
What is the treatment for shorter segment occlusions (less than 10cm
|
Short occlusions < 10 cm
< 3 cm, may be able to do PTA w/o thrombolysis For longer occlusion, thrombolysis prior to PTA |
|
|
What are the findings in a pt with portal htn on an SMA/celiac angiogram
|
Hepatic arteries have corkscrew appearance because of increased arterial flow and liver shrinkage
Enlarged spleen and splenic artery Arterioportal shunting may be seen Flow in GDA may be reversed |
|
|
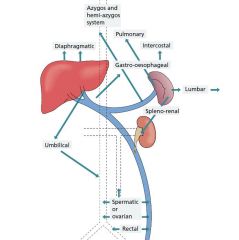
Normal flow in portal system
|
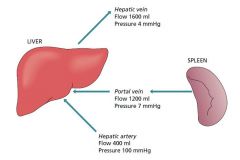
|
|
|
Flow in portal hypertension
|
|
|
|
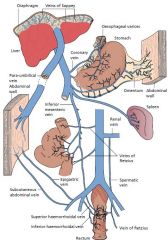
Sites of collateral circulation in portal htn
|
|
|
|
Is aterioportal shunting often seen in phtn
|
Arterioportal shunting may be seen
|
|
|
portal htn
|
reverse flow in the GDA
|
|
|
What are the collateral vessels seen in portal htn
|
Left gastric (coronary) to azygous through esophagogastric varices
Left PV to abdominal wall via paraumbilical Inferior mesenteric to internal iliac via hemorrhoidal Splenic to left renal through retroperitoneal veins (splenorenal shunt |
|
|
What are the indications for transjugular liver biopsy
|
Indication: diffuse liver disease + contraindication to percutaneous biopsy (massive ascites, coagulopathy)
|
|
|
What is the technique for a transjugular liver biopsy
|
Right IJ vein access
Catheter in right hepatic vein Obtain sample directing anteriorly |
|
|
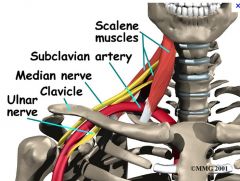
What are te 3 types of TOS
|
neurologic
arterial venous |
|
|
What is the MC type of TOS
|
neurologic (95%)
|
|
|
What is compressed in neurologic type of TOS
|
Compression of brachial plexus at point where nerves pass b/w anterior and middle scalene muscles
|
|
|
What is compressed in venous TOS
|
Subclavian or axillary vein compressed
|
|
|
What is another name of venous TOS
|
Paget-Schroetter disease
|
|
|
What is the treatment of TOS
|
thrombolysis, balloon angioplasty residual stenoses, anticoagulation and delayed surgery to correct anatomic cause
|
|
|
What is the cause of arterial TOS
|
Chronic compression leads to intimal and medial injury, can lead to occlusion or aneurysm
Mostly affects young adults |
|
|
What are the findings of arterial TOS during angiogram
|
Angio: normal or minimal stenosis in adduction, narrowing evident with provocative maneuver such as hyperabduction
|
|
|
What is the tx of arterial TOS
|
conservative if mild, surgical correction of anatomic abnormality if severe or complicated, thrombolysis if completely occluded
|
|
|
Vessesl of upper arm
|
|
|
|
Anatomy of thoracic outlet
|
|
|
|
Can thoracic outlet syndrome occur becaue of an cervical rib
|
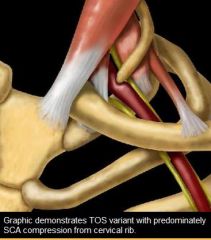
yes
|
|
|
What is the cause of VENOUS TOS
|
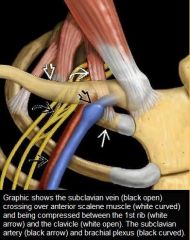
Graphic shows the subclavian vein (black open) crossing over anterior scalene muscle (white curved) and being compressed between the 1st rib (white arrow) and the clavicle (white open). The subclavian artery (black arrow) and brachial plexus (black curved)
|
|
|
Venous TOS
|
clavicle and first rib
|
|
|
Arterial TOS
|
scalene muslce and 1st rib or cervical rib (elongated transverse process)
|
|
|
What is the protocol for CT Chest Angio
|
120 cc Omnipaque 350 at 3 cc/s via antecubital vein
30 s delay Slice thickness 3 mm with reconstruction interval of 2 mm |
|
|
What are secondary findings for a PE with angiograpy
|
abrupt vessel cutoff, regional hypoperfusion, pruning of vessels, slow flow, filling of collaterals
|
|
|
What are the 3 medications used for tx of PE
|
TPA, heparin and coumadin
|
|
|
When is fibrinolytic therapy used
|
Almost always. Fibrinolytic therapy (tPA 100 mg IV over 2 h) has replaced surgical embolectomy as primary tx for hemodynamically unstable pts (hypotension, significant hypoxemia, evidence of right heart strain)
|
|
|
When is embolectomy used
|
Surgical thromboembolectomy now reserved for pts in whom fibrinolysis has failed or cannot be tolerated
|
|
|
Another way of naming the pulmonary arteries
|

|

