![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
178 Cards in this Set
- Front
- Back
|
What are the infectious causes of bronchiectasis
|
TB, viral, or chronic bacterial, or recurrent aspiration
|
|
|
What is a key feature of bronchiectasis
|
key feature is bronchial diameter > accompanying artery (signet ring)
|
|
|
What is the MCC of bronchiectasis
|
infection
|
|
|
Is there upper lobe bronchiectasis in cystic fibrosis
|
yes
|
|
|
What are the findings of cystic fibrosis
|
hyperinflation
upper lobe bronchiectasis mucus plugging prominent hila |
|
|
Does ABPA cause bronchiectasis
|
yes
|
|
|
What are the other infectious causes of bronchiectasis
|
TB
viral recurrent aspiration chronic bacterial |
|
|
What are the 2 main categories of causes of bronchiectasis so far
|
CF
infectious |
|
|
What are some rare causes of bronchiectasis
|
UIP
sarcoid radiation Immune deficiency in agammaglobulinemia Williams-Campbell Mounier-Kuhn Kartangeners |
|
|
Does mounier kuhns cause an enlarged trachea
|
yes
|
|
|
What is the ddx of a cardiophrenic mass
|
Lipoma/fat pad
Morgagni hernia Nodes Pericardial cyst |
|
|
Where do morgagni hernias tend to occur
|
anteriorly
|
|
|
Do pericardial cyst communicate with the pericardial space
|
Attached to parietal pericardium, do not communicate w/pericardial space
|
|
|
What is the shape of a pericardial cyst
|
Smooth, well-defined oval or round
|
|
|
What side do pericardial cyst most commonly occur
|
right side more than the left
|
|
|
What are the CT and MR findings for a pericardial cyst
|
CT: usually fluid density
MR: bright T2, variable T1 depending on contents |
|
|
If you see epicardial nodes how concerned should you be
|
very, enlarged nodes almost always malignant, due to lymphoma or mets. This is a common site of recurrence in Hodgkin following radiation
|
|
|
What is situs solitus
|
normal anatomic position
|
|
|
What is situs inversus
|
In situs inversus, the morphologic right atrium is on the left, and the morphologic left atrium is on the right. The normal pulmonary anatomy is also reversed so that the left lung has 3 lobes and the right lung has 2 lobes. In addition, the liver and gallbladder are located on the left, whereas the spleen and stomach are located on the right. The remaining internal structures are also a mirror image of the normal.
|
|
|
What is levocardia or levoposition
|
Levoposition/levocardia: heart positioned in left hemithorax/apex left
|
|
|
What is dextrocardia or dextroposition
|
Dextroposition/dextrocardia: heart in right hemithorax/apex right
|
|
|
What are some of the abdominal organ findings in inversus
|
stomach/spleen on R, L liver > R liver, appendix on L, L lung trilobed, morphologic R atrium on L, SVC/IVC on L
|
|
|
What does the term ambigous mean
|
lack of visceral sidedness, liver often midline, R/L isomerism
|
|
|
What are the different connections of the ventricles to the aorta
|
S (normal): LV --> aorta, Ao valve posterior and R of PV
D-TGV: Ao valve anterior and R of PV, RV--> aorta, LV --> PA L-TGV: Ao valve anterior and L of PV, RV --> aorta, LV -->PA |
|
|
What is a heterotaxia syndrome
|
a general term meaning Disturbance of the normal left-right asymmetry in the position of thoracic and abdominal organs. Polysplenia and asplenia are the 2 major syndromes
|
|
|
Are polysplenia and asplenia types of ataxia syndromes
|
yes
|
|
|
What are the chest findings of asplenia
|
Bilateral minor fissures
Symmetrical short mainstem bronchi with right-sided morphology (narrow carinal angle, early take-off of upper lobe bronchus) Pulmonary artery courses anterior to mainstem bronchus (eparterial bronchus) Cardiomegaly, pulmonary edema |
|
|
What are the chest findings of polysplenia
|
No minor fissure on either side
Symmetrical long mainstem bronchi with left-sided morphology (wide carinal angle) Pulmonary artery courses over and behind mainstem bronchus (hyparterial bronchus) Absent IVC shadow on lateral film, prominent azygous shadow on AP |
|
|
What are the findings of both asplenia and poly splenia
|
Cardiac malposition (40%: Mesocardia, dextrocardia)
Transverse liver Right-sided stomach bubble with levocardia, left-sided stomach bubble with dextrocardia, or midline stomach |
|
|
General overview of asplenia
|
Absence of a spleen
IVC and aorta on same side Bilateral superior vena cavae (SVC, 36%), absent coronary sinus Right isomerism of atrial appendages Common atrium with band-like remnant of septum crossing atria in anteroposterior direction Bilateral tri-lobed lungs Bilateral eparterial bronchi Associated with severe cyanotic CHD (atrioventricular septal defect, common atrioventricular valve, DORV, TGA, pulmonary stenosis/atresia) Abnormalities of pulmonary venous connections: TAPVR (> 80%); often obstructed, below diaphragm (type III) |
|
|
General overview of polysplenia
|
Multiple spleens, anisosplenia, multilobed spleen
Abnormalities of systemic venous connections: Azygous continuation of IVC (>70%), hepatic veins drain separately into common atrium Bilateral SVC (41%), one or both may connect to coronary sinus Left isomerism of atrial appendages Common atrium or large ostium primum ASD Bilateral bi-lobed lungs Bilateral hyparterial bronchi Associated with less severe CHD [common atrium, ventricular septal defect (VSD)] |
|
|
What is considered double left sidedness
|
polysplenia
|
|
|
What is considered double right sidedness
|
asplenia
|
|
|
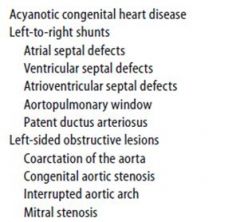
What are the causes of acyanotic heart disease
|
|
|
|
What are the causes of congenital heart disease with decreased flow
|

|
|
|
What are the cause of congenital cyanotic heart disease with increased pulmonary flow (last slide is cyanotic also)
|

|
|
|
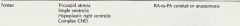
What are the indications and function of a fontan procedure
|
|
|
|
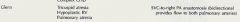
What are the indications and function of a Glenn
|
|
|
|
What are the procedures used to repair transposition of the great vessels
|

|
|
|
What is a norwood procedure
|

|
|
|
What are the CXR findings of a pleural effusion
|
Frontal XR: “water bottle”
Lateral XR: sometimes nl pericardium visible b/w epicardial and pericardial fat as a thin linear opacity in retrosternal region If opacity > 4 mm --> pericardial effusion |
|
|
Is a tracheal tumor worrisome in adults
|
yes, in adults, 90% of primary tracheal tumors are malignant, 90% benign in peds
|
|
|
What is the ddx of benign appearing endotracheal masses
8 |
hemangioma
papilloma hamartoma lipoma chondroma fibroma granular cell myoblastoma |
|
|
What is the ddx of malignant endotracheal masses
8 |
squamous cell CA
adenoid cystic CA econdary involvement by esophageal or thyroid CA mucoepidermoid CA, carcinoid, adenoCA lymphoma small cell CA mets (melanoma, breast, RCC) |
|
|
If a child has an endotracheal mass is it malignant
|
no, up to 90% are benign
|
|
|
What should be known about laryngeal papillomatosis
|
Laryngeal nodules due to human papilloma virus, usually self-limited infection
< 1% seed the lung, known as invasive papillomatosis At risk to develop squamous cell carcinoma (2%) |
|
|
2/3 either of tracheal neoplasm are squamous cell carcinoma or adenoid cystic carcinom
|
yes
|
|
|
Do mucoepidermoid, carcinoid and adenoid cystic neoplasm occur in the trachea or bronchi
|
yes
|
|
|
What are the findings of a VSD
|
pulmonary arteries are enlarged with shunt vascularity
LA enlargement |
|
|
What are the findings of ebsteins anomaly
|
enlarged heart
increased pulmonary vasc cyanotic (type 3 lesion from UCSF) |
|
|
What is the main abnormality of ebsteins anomaly
|
Malposition of septal and posterior leaflets of tricuspid valve resulting in severe tricuspid insufficiency
|
|
|
What happens to a large portion of the RV in ebsteins
|
Large portion of RV lies above the valve, within the RA (“atrialized”)
|
|
|
What are the CXR findings of ebsteins anomaly
|
decreased pulmonary blood flow (severe TR and R to L shunt via ASD), small PAs, huge heart due to enlarged RA/RV
(correct prior slide there is decreased vascularity) |
|
|
What is the ddx of ebsteins anomaly
|
Pulmonary atresia with intact septum (also cardiomegaly and oligemia)
|
|
|
What is the difference between ebsteins and TOF/pulmonary atresia with VSD
|
TOF and pulm atresia with VSD are type 2 lesions and will have decreased pulmonayr vascularity
|
|
|
Where does congenital partial absence of the pericardium MC occur
|
Most pericardial defects are partial and occur over left atrial appendage and adjacent pulmonary artery
|
|
|
What percent of pt with partial congenital absence of the pericardium have associated anomalies
|
20% have assoc abnormalities (ASD, PDA, TOF, bronchogenic cysts, sequestration)
|
|
|
What is a potential complication of partial absence of the pericardium
|
Risk of strangulation of portion of heart protruding through defect
|
|
|
What are the findings of partial absence of the pericardium
|
abnl convexity b/w PA and left atrial appendage, concave AP window
|
|
|
What is the ddx of bilateral hilar lymphadenopathy
|
sarcoid
lymphoma mets infection castlemans |
|
|
What type of infections cause bilateral enlarged LN
|
TB and fungal
|
|
|
Where do the enlarged LN of sarcoid occur
|
paratracheal
hilar |
|
|
Do castlemans LN tend to avidly enhance
|
yes
|
|
|
What are the findings of stage 1 sarcoidosis
|
bilateral hilar and paratracheal LN
|
|
|
What are the lung findings of stage 3 sarcoidosis
|
The most common parenchymal pattern of sarcoidosis is a reticulonodular configuration, correlating with the non-caseating granulomas noted at pathology. Slightly less common is alveolar pattern made up of diffuse, small, indistinct opacities due to the alveolar filling with mononuclear cells
|
|
|
What are the stages of sarcoid
|
Stage 0: Normal chest radiograph (50%, at presentation)
Stage 1: Lymphadenopathy (45-65%) Stage 2: Lymphadenopathy and lung opacities (30-40%) Stage 3: Lung opacities (10-15%) Stage 4: Fibrosis with or without lymphadenopathy (5-25%) |
|
|
What are the radiographic findings of complete lung atx
|
Completely opaque hemithorax with ipsilateral shift of heart and mediastinum
Compensatory hyperinflation of contralateral side, which crosses over midline, especially anteriorly, producing large retrosternal space on lateral |
|
|
What is the ddx of oppacifiction of a hemithorax
|
atx
consolidation post pneumonectomy congenital pulm agenesis |
|
|
What are the CXR findings of a Zenkers diverticulum
|
Retroesophageal superior mediastinal mass containing an air-fluid level (on upright)
Best seen on lateral esophagram extending posteriorly at the C5/6 level On frontal, it protrudes laterally (usually left) when it is large |
|
|
What are the CXR findings of NF1 (changes from masses only)
|
Multiple spherical paravertebral masses which may erode ribs, widen rib spaces, and widen neuroforamina
Look for posterior vertebral body scalloping and wide neural foramina |
|
|
Can the neurofibromas arise from the intercostal nerves
|
yes, can arise from intercostal nerves resulting in multiple pleural-based opacities with ribbon ribs
|
|
|
What are the parenchymal changes that may be seen in NF1
|
Upper lobe cystic and bullous disease, lower lobe fibrosis
|
|
|
Can NF1 result in kyphosis
|
yes
|
|
|
What are the finding of neurofibromas in NF1 on CT (enhancement characteristic and calcifications)
|
neurofibromas homogeneous or heterogeneous enhancement, with punctate Ca+ in 10%
|
|
|
What are the signal characteristics of neurofibromas on MR
|
low to intermediate T1 and high T2
|
|
|
Does NF1 result in fibrotic changes to the lower lung fields
|
yes
|
|
|
What are the causes of pneumomediastinum
|
alveolar rupture
tracheal rupture esophageal rupture iatrogenic pneumoperitoneum pneumoretroperitoneum |
|
|
What are the causes of alveolar rupture
|
usually from asthma, but also from mechanical ventilation with air dissecting into mediastinum via interstitium
|
|
|
What are the causes of esophageal and tracheal rupture resulting in pneumomediastinum
|
trauma
|
|
|
how does a pneumoperitoneum or retroperitoneum result in pneumomedistinum
|
tracking up of air
|
|
|
What is the continous diaphragm sign
|
continuous diaphragm sign.” The entire diaphragm is visualized from one side to the other because air in the mediastinum outlines the central portion which is usually obscured by the heart and mediastinal soft tissue structures that are in contact with the diaphragm. This is from a pneumomediastinum
|
|
|
What are some associated findings besides pneuomomediastium if a patient has a ruptured esophagus
|
Air next to esophagus
+/- Abscess Leak on water soluble esophagram Left effusion and mediastinal widening |
|
|
Do you see a widened mediastinum, left effusion and pneuomomedistinum in a esophageal rupture
|
yes
|
|
|
What are assoiciated findings of a tracheal rupture
|
Persistent, severe pneumomediastinum, subcutaneous emphysema and PTX
Does not resolve with chest tube placement Fallen lung sign: lung falls inferolateral instead of the usual medial collapse Ectopic ETT or balloon cuff |
|
|
What it the fallen lung sign
|
lung falls inferolateral instead of the usual medial collapse
|
|
|
What is a rare but serious complication from histoplasmosis
|
fibrosing mediastinitis
|
|
|
What will you see in fibrosing mediastinitis
|
fibrosis encasing the mediastinum
|
|
|
Can fibrosing mediastinitis cause SVC syndrome
|
yes
|
|
|
What is another cause of fibrosing mediastinitis
|
mediastinal fibrosis from malignancy
|
|
|
What are the clinical SS of SVC syndrome
6 |
Facial & neck swelling, cyanosis, venous distension, SOB, HA, and hoarseness
|
|
|
What are the findings of a pneumomediastinum on abdominal X-ray
|
Linear lucency extending from aortic knob down left heart border
Continuous diaphragm sign underlying the cardiac silhouette Outlining of descending aorta and pulmonary arteries Subcutaneous emphysema Air may also outline SVC and great vessels |
|
|
What are the findings on decubitus film if a pt has pneumomediastinum
|
Decubitus: pneumomediastinum does not change
|
|
|
Can SVC syndrome be life threatening
|
yes, may be life threatening if untreated due to laryngeal edema or CNS congestion
|
|
|
What are the findings in CT and MR in a pt with SVC syndrome
|
SVC stenosis, thrombosis, occlusion, cause (mass of tumor or calcified nodes in histoplasmosis with fibrosing mediastinitis)
|
|
|
What is the tx for SVC syndrome
|
emergent radiation or chemo (if due to malignancy), percutaneous thrombolysis, balloon angioplasty, stent (large wallstent, 16 mm)
|
|
|
What are the radiographic findings of fibrosing mediastinitis
|
Deposition of fibrous tissue, collagen
Encases and obliterates vessels, airway, esophagus Infiltrative Frequently calcifies |
|
|
What is the most common cause of mediastinitis
|
MC due to histoplasmosis
|
|
|
Does fibrosing medistinitis calcify
|
yes
|
|
|
What is a simple pulmonary AVM
|
this is one feeding artery and one feeding vein
|
|
|
What percent of pulmonary AVMs are simple
|
80%
|
|
|
What percent of patients with pulmonary AVMs have osler-weber-rendu
|
70% have Osler-Weber-Rendu, a syndrome of cutaneous and mucosal telangiectasias and AVMs in other organs
|
|
|
What is a potential major complication of a pulmonary AVM
|
R to L shunt, which may lead to stroke, brain abscess, cyanosis
|
|
|
What part of the lung does a pulmonary AVM most commonly occur
|
the lower lung fields
|
|
|
What are the findings on plain film in a pt with AVM
|
Single or multiple nodules, typically in medial third of lung
Feeding artery often seen as dilated vessel originating in hilum, and draining vein heading toward left atrium |
|
|
Does a pulmonary AVM look like a nodule on plain film
|
yes
|
|
|
What are the angiogram and CT findings of a pulmonary AVM
|
CT: enhancing feeding and draining vessels
Angio: feeding and draining veins and nidus |
|
|
What is the treatment of an pulmonary AVM
|
Coils (1-2 mm larger than artery being embolized) placed proximal to nidus or glue
|
|
|
What type of pleural fluid collection occurs in pts with TB
|
empyema
|
|
|
What are the CXR findings in a patient with TB empyema
|
loculated lenticular collection, forms obtuse angles with chest wall, does not change with pt positioning, air-fluid level if bronchopleural fistula
|
|
|
What are the CT findings in a patient with TB empyema
|
split pleura sign (enhancement of both visceral and parietal pleura around loculated effusion), increased adjacent extrapleural fat
|
|
|
Is there increased adjacent extrapleural fat in a pt with TB empyema
|
yes
|
|
|
What is a fibrothorax
|
Circumferential pleural thickening causing decreased lung volume
|
|
|
What are the causes of a fibrothorax
|
TB
hemorrhagic effusion pyogenic empyema asbestos malignancy (mesothelioma, metastatic adenoCA) |
|
|
What types of metastatic dz will cause a fibrothorax
|
mesothelioma
metastatic adenocarcinoma |
|
|
If there is a fibrothorax with calcification what should be strongly suspected
|
When Ca+, TB is almost always the cause (NOT asbestos, the fibrothorax of asbestos does not calcify)
|
|
|
What is a characteristic of a fibrothorax that should make you highly suspicious for a malignancy
|
thickened, malignancy is lumpy/nodular/masslike, circumferential, > 1 cm thick
|
|
|
What are the 4 MC cardiac diseases with a right aortic arch
|
4 MC CHD with right arch: truncus arteriosus, TOF, transposition, tricuspid atresia
|
|
|
What 2 of the previous slide will have increased pulmonary flow
|
truncus, TOF
|
|
|
What is the major finding in truncus arteriosis
|
Single vessel arising from heart giving rise to systemic, pulmonary and coronary circulation
|
|
|
Is truncus arteriosis always associated with VSD
|
yes
|
|
|
What are the subtypes of truncus arteriosis based on
|
Subtypes based on origin of PA from truncus
|
|
|
What percent of patients with a truncus arteriosus have a right aortic arch
|
33%
|
|
|
What is the radiographic appearance of truncus arteriosis
|
increased pulmonary flow, right arch, cardiomegaly (biventricular)
Although pulmonary flow is increased, main pulmonary artery area is often concave b/c PA is not arising in its normal location from the RVOT |
|
|
What are the radiographic findings of an intracardiac lipoma
|
Bright on T1 and bright on FSE T2, dark on FS and no enhancement
|
|
|
What side are intracardiac lipomas most common
|
right
|
|
|
What is the course of a parenchymal contusion of the lungs
|
Usually evident on XR by 6 h post trauma
Clears rapidly, within 72 h |
|
|
What is the appearance of a parenchymal contusion on CXR
|
XR: usually nonsegmental, homogeneous opacities, frequently peripheral in location, +/- associated fractures
|
|
|
What should be considered if the pulmonary contusions do not clear within 72h
|
If parenchymal opacity does not resolve post trauma, consider pneumonia, ARDS, or pulmonary edema
|
|
|
What are the indications for mitral valve replacement
|
CHF with mitral stenosis or insufficiency, deteriorating LV function indices (EF) with mild or moderate symptom
|
|
|
What are the 3 types of mechanical heart valves
|
St Jude: bileaflet configuration
Bjork-Shiley: tilting disk Starr-Edwards: caged ball |
|
|
What are 2 prosthetic heart valves
|
Homograft from cadaver
Porcine xenograft |
|
|
Where is a mitral valve seen on the lateral films
|
valve projects posterior to line drawn connecting point where sternum touches diaphragm anteriorly and tracheal bifurcation posteriorly
|
|
|
Where are mitral valves seen on the frontal film
|
harder to distinguish different valves, but long axis of mitral valve will parallel line drawn from right heart border through cardiac apex, whereas long axis of an aortic valve is angled more toward the right neck
|
|
|
What are 2 other names for schimitar syndrome
|
hypogenetic lung syndrome, congenital pulmonary venolobar syndrome
|
|
|
What are the findings of schimitar syndrome
|
There is hypoplasia of the right lung and PA. There is also anomalous venous drainage of R lung by single vein which runs inferiorly parallel to R heart border to join IVC below diaphragm
|
|
|
Where does the anomalous draining vein of schimitar syndrome connect with the IVC
|
below the diaphragm
|
|
|
How is the right lung supplied in schimitar syndrome
|
Usually systemic arterial supply to the right lung from a vessel off the aorta
|
|
|
What are the findings of schimitar syndrome
|
Small R hemithorax with small R PA and decreased pulmonary vascularity
Shift of heart and mediastinum to right Curvilinear opacity (scimitar vein) heading toward diaphragm |
|
|
What are the 2 types of pectus deformities
|
excavatum and carinatum
|
|
|
What is the shape of the sternum in pectus excavatum
|
Inward depression of sternum
|
|
|
What is pectus excavatum associated with
|
Assoc w/Marfan, Poland, OI, congenital scoliosis
|
|
|
What are the chest x ray findings of pectus excavatum
|
Leftward shift of heart and loss of right heart border
Posterior ribs are horizontal and anterior ribs are vertical Lateral shows inward depression of sternum LV displaced posteriorly, even though heart is not enlarged Very narrow AP diameter of chest and loss of normal thoracic kyphosis |
|
|
What is pectus carnivatum
|
outward bowing of the chest
|
|
|
What are the findings of RML atx
|
Frontal radiograph of the chest will demonstrates indistinctness of the right heart border and elevation of the right hemidiaphragm from volume loss. The lateral view of the chest will show downward displacement of the minor fissure and slight upward bowing of the major fissure, both bordering the increased triangular density of the atelectatic middle lobe.
|
|
|
What is RML syndrome
|
the right middle lobe is susceptible to chronic collapse secondary to prior inflammatory episodes. This is especially true in children.
|
|
|
What are the CXR findings of RML syndrome
|
RML volume loss with tubular lucencies and tram tracking
|
|
|
What are the CT findings of RML syndrome
|
RML bronchus patent but narrowed and bronchiectasis present in collapsed RML
|
|
|
What is the clinical presentation of RML syndrome
|
May be asymptomatic or have recurrent pneumonias
|
|
|
What infection will produce similar findings to RML
|
Chronic MAC infection produces similar findings
|
|
|
What patients tend to get MAC
|
Usually in elderly females with systemic symptoms such as weight loss, and in pts with COPD, asthma, CF, steroid use, and AIDS
|
|
|
What is worrisome about a traumatic diaphragmatic hernia
|
Assoc w/severe injury and high mortality due to assoc injuries
|
|
|
Where do traumatic diaphragmatic injuries tend to occur
|
Tear typically in central tendon or musculotendinous junction, and 70% are left-sided
|
|
|
What is a potential major complication of a traumatic diaphragmatic hernia
|
Delayed diagnosis may result in bowel strangulation and obstruction
|
|
|
What is the ddx to a unilateral hyperlucent lung
|
POEMS
Poland Syndrome Pneumothorax Oligemia/Obstruction (PE) Emphysema Mastectomy Swyer James |
|
|
What is poland syndrome
|
is a rare birth defect characterized by underdevelopment or absence of the chest muscle (pectoralis) on one side of the body and (but not always) webbing of the fingers (cutaneous syndactyly) of the hand on the same side (ipsilateral hand) mostly common on the right side of body and found more in males than females.
|
|
|
What is swyer james syndrome
|
Swyer-James syndrome is a manifestation of postinfectious obliterative bronchiolitis. In SJS, the involved lung or portion of the lung does not grow normally and is slightly smaller than the opposite lung. The characteristic radiographic appearance is that of pulmonary hyperlucency, caused by overdistention of the alveoli in conjunction with diminished arterial flow and has been linked to adenovirus type 2
|
|
|
What is bronchial atresia
|
Congenital bronchial atresia is a rare anomaly that results from focal obliteration of a proximal segmental or subsegmental bronchus that lacks communication with the central airways
|
|
|
What happens to the bronchus distal to the stenotic bronchus
|
The bronchi distal to the stenosis become filled with mucus and form a bronchocel
|
|
|
What happens to the alveoli that are supplied by the stenotic bronchus
|
The alveoli supplied by these bronchi are ventilated by collateral pathways and show features of air-trapping, resulting in a region of hyperinflation around the dilated bronchi
|
|
|
Where is the MC location of bronchial atresia
|
The upper-lobe bronchi are more frequently affected; middle and lower lobes are rarely affected.
The abnormality is an incidental finding in approximately 50% of cases, mostly in young men, and generally produces no symptoms or signs |
|
|
What does bronchial atresia look like in a newborn and a child
|
In the newborn period, bronchial atresia is seen as a water-density mass.
Later in childhood, the fetal lung liquid escapes and bronchial atresia is found because of focal air trapping. |
|
|
What is the appearance of bronchial atresia in an adult
|
In adults, bronchial atresia characteristically is seen as a solitary pulmonary nodule due to a mucus plug and less frequently as congenital lobar emphysema.
|
|
|
What is the ddx of a pleural mass
|
lipoma
solitary fibrous tumor of pleura |
|
|
Can a solitary fibrous tumor of the pleura be malignant
|
yes
|
|
|
What are the characteristics of a solitary fibrous tumor of the pleura
|
Circumscribed
1-40 cm Ca+ 7-26% Effusion 17-37% Usually enhances HPOA 1/3 Hypoglycemia 5% MR: low T1, T2 Malignant 7-60% |
|
|
Can a solitary fibrous tumor be malignant
|
yes, up to 60%
|
|
|
Do solitary fibrous tumors of the pleura enhance
|
yes, usually they do
|
|
|
Do solitary fibrous tumors of the pleura have associated effusions
|
yes up to 30%
|
|
|
What is the MR characteristics of a solitary fibrous tumor of the pleura
|
low on T1 and T2
|
|
|
What 2 diseases that occur in the upper lungs can both progress and cause fibrosis of the lung parenchyma
|
Occurs in complicated silicosis, endstage sarcoid
|
|
|
Can coal workers pneumiconisis cause progressive massive fibrosis
|
yes
|
|
|
What two conditions may have egg shell calcifications of the LN
|
CWP and silicosis
|
|
|
What infection often occurs simultaneously with silicosis
|
TB, superimposed TB may occur (silicotuberculosis) (25%)
|
|
|
What suggest a silicosis disease that is superinfected by TB
|
Suggested by asymmetric nodules/consolidation, cavitation, rapid disease progression
|
|
|
What are the CXR findings of a paraspinal abscess
|
posterior mediastinal mass, vertebral body lytic changes, widening of paravertebral stripe
|
|
|
What is rule of thumb for differentiating vetebral body related masses from other posterior mediastinal masses
|
Unlike other posterior mediastinal masses, vertebral body related ones (infection, trauma, tumors) often produce bilateral fusiform findings
|
|
|
What may be seen in Potts disease (TB)
|
Pott disease may show paraspinal abscesses in the psoas
|
|
|
What are the CT findings of malignant melanoma
|
Nodular, circumferential pleural thickening, involves mediastinal pleura, > 1 cm thick, thick fissures, pleural effusion, loss of volume, pleural Ca+, invasion of chest wall
|

