![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
|
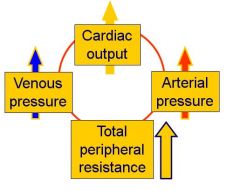
What will happen to the arterial pressure and venous pressure if there is a fall in TPR, but CO remains constant?
|
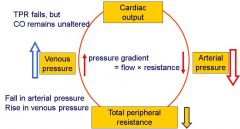
Arterial pressure = CO x TPR
|
|
|
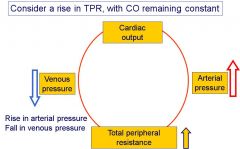
What happens to venous pressure and arterial pressure when TPR rises but CO remains constant?
|
|
|
|
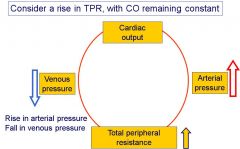
What happens to venous pressure and arterial pressure when TPR rises but CO remains constant?
|
|
|
|
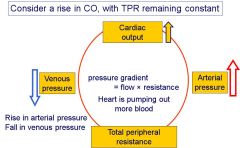
What happens to arterial and venous pressure when CO rises but TPR stays the same?
|
|
|
|
What happens to arterial and venous pressure when CO falls but TPR stays the same
|
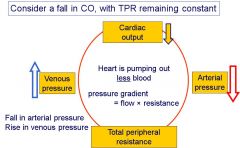
|
|
|
What happens if there is an increase in the demand for blood?
|
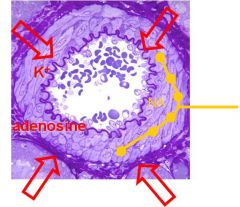
- An increase in need raises the output of metabolites from cells = metabolic demand
- This leads to vasodilation and a fall in TPR - If cardiac output remains the same, this will cause a fall in arterial pressure and a rise in venous pressure - The heart needs to pump more blood to meet the demand which has been expressed in terms of changes in TPR, arterial pressure and venous pressure - The heart responds to these changes to meet the demand, the change in venous pressure being particularly important - The response is partly automatic and intrinsic to the heart itself and involves in changes in stroke volume - The response is aided by reflex action (involving especially the baroreceptor reflex) involving changes in contractility and rate |
|
|
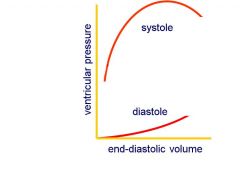
Define the terms pre-load and after-load on the ventricular myocardium
|
- Pre-load = load on the ventricular myocardium during diastole
- After-load = load of the ventricle when is has to eject blood into the circulation during systole |
|
|
What are the factors that determine how much the ventricles fill during diastole?
|
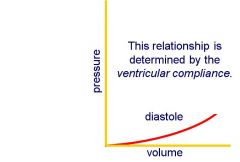
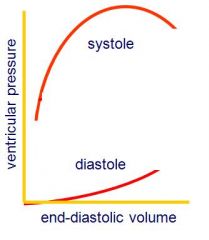
- As the ventricle fills its pressure rises somewhat
- Filling will cease onece the pressure equals venous (filling) pressure - The higher the venous pressure the more the ventricles will fill - The relationship between the end-diastolic volume in the left ventricle and venous pressure is almost linear - However, the relationship is determined by ventricular compliance - Ventricular compliance may be reduced in disease e.g. both in ventricular hypertrophy and in restrictive cardiomyopathy - In these conditions the compliance of the ventricle is reduced and it requires a higher venous pressure to fill the heart = higher slope |
|
|
Describe how changes in end-diastolic volume affect the force of contraction of the myocardium during the following systole
|
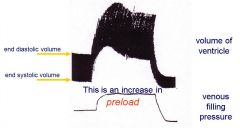
- Starlings law of the heart = the amount of stretch the heart undergoes determines the strength the heart will contract
- Therefore, and increased end-diastolic volume will increase the force of contraction of the myocardium during sytole - Increase of filling pressure → increase in end diastolic volume → increase in stroke volume |
|
|
Describe the relationship between venous pressure and stoke volume at a constant afterload
|
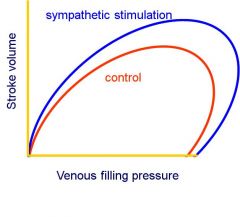
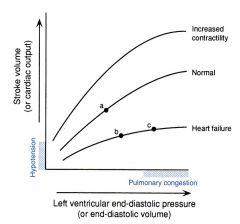
- The Starling curve relates stroke volume to the filling pressure
- In diastole, the ventricle is connected to veins, so venous pressure determines the end-diastolic stretch, or pre-load' on the myocardium - Once systole beins, the ventricles are isolated from the veins but connected to the arteries, and the force necessary to expel blood into the arteries, or the 'after-load', determines what happens during systole - Pre-load and after-load may vary independently - An increase in venous pressure (and therefore end-diastolic volume) will lead to an increase in stroke volume (so more in = more out), at constant afterload - The slope of this relationship gives the contractility of the ventricle - The contractility can be altered by noradrenaline or adrenaline |
|
|
Define contractility and describe how the Starling curve is changed by factors that increase or decrease the contractility of the ventricular myocardium
|
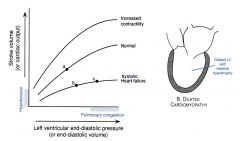
- Increased contractility may cause increased stroke volume at a lower end-diastolic pressure
- Heart failure = reduced contractility so requires a higher pressure to avoid arterial pressure loss |
|
|
How can the heart maintain its output in the face of an increased TPR is venous return is maintained?
|
The heart may also maintain its output in the face of an increased TPR or if the aortic pressure is increased, if venous return is maintained:
an increase in after-load. - If the resistance is raised, it becomes harder to eject blood → immediate effect is a reduction in stroke volume - If stroke volume is reduced (and the ventricle empties less) → once it has filled again, end-diastolic volume will have increased - An increase in end-diastolic volume enables the heart to do more work. - Stroke volume then recovers, but end diastolic volume has increased (and the ejection fraction has fallen) - If TPR increases, an increased end-diastolic volume will permit ventricular pressure to rise further in systole maintaining stroke volume. - Stroke work will increase due to an increased afterload, provided venous return is maintained - However, a rise in TPR might also be expected to reduce venous pressure (and increase arterial pressure) – and this will reduce EDV and stroke work, helping correct the rise in arterial pressure that would otherwise occur - Conversely, a fall in TPR is also likely to raise venous pressure – and this will increase EDV and stroke work, helping correct the fall in arterial pressure that would otherwise occur |
|
|
Consider the consequences of a fall in arterial blood pressure
|
- Increase in venous pressure and therefore stroke volume
- In addition, through reflex action • Increase the heart rate reducing the vagal (sympathetic) tone to the heart and increasing sympathetic activity • Increase the contractility of the heart increasing sympathetic activity → pump more blood • Effects of blood vessels as well – vasoconstriction will raise TPR and this rise will help restore blood pressure. |
|
|
How do arterial receptors detect changes in arterial changes
|

- These afferent nerve fibres respond to changes of blood pressure through stretch of the walls of the carotid sinus and aortic arch.
- Impulses are conducted at lower frequency at low pressures and at raised frequency at high pressures. |
|
|
Describe the effects of a fall in arterial pressure, detected by the arterial baroreceptors, upon heart rate and ventricular contractility
|
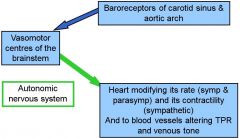
- Overrides any intrinsic effects of the heart
- Baroreceptors are blunted in people with hypertension = sensitized to a high range of pressures |
|
|
Decribe the effects of rises of venous pressure on heart rate
|
- Both atria contain stretch receptors that sense filling pressure – at the atrio-venous junctions
- Their principal function is to control extracellular fluid and blood volume (regulates Na+ excretion from the body) (see Urinary module) - But they also have an effect on heart rate at high end diastolic volume = puts out hormones allowing pressure etc to change |
|
|
What occurs at high end-diastolic volumes?
|
At high end-diastolic volumes two things happen:
1. The diastolic pressure becomes high – venous pressure will be high – increasing the chance of oedema 2. The heart responds less well with an increase in stroke work to a further increase in end-diastolic volume |
|
|
What are the effects on venous and arterial pressures if the heart stops?
|
- Arterial pressure will fall
- Venous pressure will rise - They will come to be equal if the heart stops and will be determined by: • the blood volume • the compliance of the circulation = the mean filling pressure of the circulation |
|
|
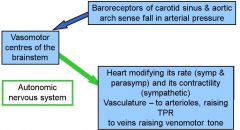
Describe the intrinsic reflex mechanism of the heart
|
- An increase in venous pressure – an increase in filling pressure – will increase the stroke volume
- Intrinsic mechanism – through Starling’s Law of the Heart - A decrease in arterial pressure will reduce the work the heart has to do to pump out the same volume of blood. - If venous return remains the same, the same stroke volume will be ejected at a lower end diastolic volume. - However this response to a change in arterial pressure principally depends on a reflex mechanism, responding to altered information from baroreceptors in the carotid sinus and aortic arch, altering cardiac contractility |
|
|
Describe the reflexes mechanisms associated with arterial pressure
|
- A fall in blood pressure risks supply to the brain (and may cause syncope)
- The resistance to flow must therefore rise elsewhere in the circulation (eg skin, gut) - Principally through a reflex response to information from the baroreceptors in the carotid sinus and aortic arch - So falls in arterial pressure lead to vasoconstriction - A fall in arterial pressure will also lead to venoconstriction, increasing the return of blood to the heart |
|
|
What drives the cardiac output - the heart or the circulation?
|
- Cardiac output = heart rate × stroke volume
- If the heart rate is raised → initially the cardiac output will increase but the venous pressure with fall as a result → reduced end-diastolic volume → reduced stroke volume, correcting CO - The heart does not drive the circulation, but is driven by it = the output of the heart meets the demands of the circulation |
|
|
Describe the effects of ingestion of food on the circulation
|
- Expect, and can show, that blood flow increases
→ Increasing GI motility, secreting endocrine and exocrine factors, absorbing products of digestion → Postprandial hyperaemia - Number of factors cause increased flow: • Metabolic factors (adenosine, CO2, hypoxia) • Effects of absorbed substances • Vasoactive GI hormones • Neural effects - GI tract circulation important element in TPR – these changes will reduce TPR - This must be corrected across the system - Rise in venous (filling) pressure increases stroke volume (Starling’s Law) - Fall in arterial pressure means that contractility of the heart is increased by reflex means. - Also then gives an increase in CO - Tending to correct both arterial and venous pressure |
|
|
Describe the cardiovascular response to exercise
|
- Requires a large increase in blood flow to skeletal muscle
• Vasodilatation in skeletal muscle reduces TPR • Movements of skeletal muscle will increase venous return and raise venous pressure - Might envisage exercise as a situation where the required increase in CO can be met through an increase in stroke volume - But if end-diastolic volume becomes very large: • End diastolic and therefore venous pressure becomes high, increasing likelihood of pulmonary oedema • The stroke volume ceases to increase with end-diastolic volume - So another mechanism dominates • Cardiac output rises – usually up to 3× ( but can rise 5×) • Principally through an increase in heart rate (from 60 to 180 beats per min) • Relatively little increase (10 – 20%) in stroke volume |
|
|
Describe the cardiovascular response to stading from a lying position
|
- Gravity has effects on the circulation – and particularly on venous return
- Lying down – lower extremities are at the same level as the heart - On standing - adding the column of blood below the heart to the pressure - Need muscle pump etc to return blood to the heart – a particular problem for superficial veins - Blood will be pooled in the superficial veins of the legs - Central venous pressure falls - End-diastolic volume will fall and cardiac output will go down - If the TPR is unchanged, arterial pressure will FALL too - Difficult situation for the heart to respond to through Starling's Law - This must be corrected through reflex action (see diagram) - If this compensation is insufficient (or not fast enough) may lead to fainting = postural hypotension - If other physiological responses are reducing TPR the response to a change of posture may be compromised (i.e. enhances chances of failure) • after eating a meal → vasodilatation in GI tract • in hot environment → vasodilatation in skin • If there is pharmacological blockage of a1 receptors for example → can't constrict blood vessels in response so are difficult for patients to take as can't respond to changes in blood pressure |
|
|
What occurs in the cardiovascular system due to hemorrhage?
|
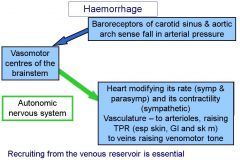
- Dangerously rapid loss of blood
- Fall in central venous pressure - Causes a reduction in stroke volume and so a reduction in cardiac output - Unless there is a change in peripheral resistance arterial pressure will FALL - The heart cannot itself respond to correct these changes • May become self-reinforcing owing to reduced blood flow → build up of vasodilator metabolites, which reduces TPR • Leading to a further fall in blood pressure to haemorrhagic shock and death = can be sudden so must treat rapidly and give fluids to restore volume - The immediate response to haemorrhage is principally through reflex responses to the change in blood pressure - And subsequently through restoration of blood volume at the expense of interstitial fluid - Recruiting from the venous reservoir is essential (see diagram) |
|
|
Describe the effects on hydrostatic pressures during hemorrhage
|
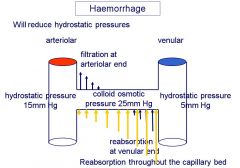
- Recruiting from the venous reservoir is essential, since increasing the cardiac output would tend to lower venous pressure further.
- The heart rate can become very high – and the pulse weak - At blood pressures below ~40mm Hg, the cerebral ischaemia that ensues stimulates an intense sympathetic discharge - Fluid is transferred from the extracellular space – from interstitial fluid – into the vasculature - This will reduce hydrostatic pressure, so that oncotic pressure is always higher - This causes increased reabsorption throughout the capillary bed and blood volume is corrected within 1/2 hour - Reabsorption of interstitial fluid restores blood volume • though at the expense of haematocrit and of plasma proteins (colloid osmotic pressure will fall) - Other longer term physiological mechanisms will: • restore extracellular fluid volume – for example, angiotensin II will stimulate secretion of aldosterone, & haematocrit through increased red cell production. |
|
|
Describe a situation with long-term increases in blood volume and their effect on the cardiovascular system
|
- Occasionally changes in renal function or in diet – perhaps a high Na+ diet - may lead in increases in extracellular fluid volume
- Increase in blood volume will raise venous pressure → increased end-diastolic volume → increased cardiac ouput increasing arterial pressure - Increase in flow may lead to autoregulatory increases in TPR - These changes lead to hypertension - Reversible in the short term = aided by the use of diuretics favouring the excretion of salt and water - But in the longer term changes in the walls of blood vessels make reversal more difficult and blunt the baroreceptor reflexes - A similar situation is seen in Eisenmengers syndrome = changes in blood vessel histology makes them less compliant → blunted reflexes. This can be picked up in the eyes = silver-wiring |

