![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
24 Cards in this Set
- Front
- Back
|
Describe the 5 types of shock
|
- Hypovolaemic
- Cardiogenic - Mechanical - Septic - Anaphylactic |
|
|
Define shock
|
Acute circulatory failure resulting in inadequate or disordered tissue perfusion and insufficient oxygen supply to cells
|
|
|
List some causes of hypovolaemic shock
|
- External blood loss
- Hidden blood loss – intrathoracic, intra-abdominal, retroperitoneal, bony injury (e.g. a fractured femur can lose 4 units of blood with little distention of the thigh) - Other fluid losses • GIT • Urinary • Cutaneous e.g. burns, pyrexia • Into the tissues |
|
|
Describe the pathophysiology of hypovolaemic shock
|
1. Loss of circulating volume
2. Reduced venous return and cardiac filling 3. Reduced stroke volume – Starling’s law 4. Reduced cardiac output ~SVxHR 5. Reduced BP ~COxSVR 6. Reduced oxygen delivery ~COx[Hb]xSaO2 7. Impaired cellular function |
|
|
Describe the sympatho-adrenal response
|
- Reduced stretch of aortic and carotid baroreceptors, and blood flow to chemoreceptors causes reflex increase in sympathetic tone
- Heart – tachycardia and increased contractility - Peripheral vessels – arteriolar and venous vasoconstriction → return from ECF to blood from capillary beds - Release of catecholamines from adrenal medulla → ↑ CO and BP - Kidney - secretion of renin by juxta-glomerular apparatus leading to angiotensin II and aldosterone release; vasoconstriction |
|
|
What are the effects of the sympatho-adrenal response
|
- Reduced capillary hydrostatic pressure leads to fluid moving from ECF to blood
- Venoconstriction increases cardiac filling - Arteriolar constriction maintains blood pressure - Kidney - reduced filtration and increased re-absorption restores circulating volume - Increased contractility and heart rate support cardiac output with moderate hypovolaemia - Blood flow re-distributed to vital organs – brain, heart, kidneys, liver, respiratory muscles |
|
|
What are the clinical features of hypovolaemic shock
|
• Skin
- Cold, clammy, pale, slow capillary refill • Circulation - Tachycardia - Early - maintained systolic pressure + increased diastolic pressure, hence reduced pulse pressure - Late - hypotension - Collapsed peripheral and central veins • Brain - Confusion, restlessness, anxiety, thirst • Kidney - Oliguria, anuria • Respiration - Tachypnoea • Neuroendocrine - Pituitary, adrenal, pancreas, atrium • Inflammatory mediators Complement, cytokines, platelet activating factor, products of arachidonic acid metabolism, lysosomal enzymes • Microcirculatory changes - Early = Fluid returns to circulation due to sympathetic tone and autoregulation - Late = Compensation begins to fail. Fluid loss as vascular tone fails, capillary permeability increases, increased viscosity and intravascular coagulation to control blood loss → DIC |
|
|
What are the metabolic changes that occur due to hypovolaemic shock?
|
- Anaerobic metabolism
• Lactate and H+ production = metabolic acidosis - Hyperglycaemia - Lack of ATP leads to Na-K pump failure, cell swelling, release of K and lysosomal enzymes, entry of Ca and cell death |
|
|
Describe the management of cardiogenic shock
|
- Assessment > treatment > re-assessment
- Attention to • Oxygenation • Replacement of circulating volume (fluids at body temperature) • Diagnosis and treatment of cause of fluid losses |
|
|
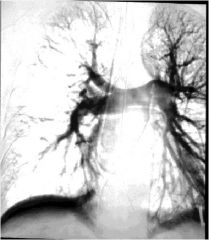
Describe the clinical features of cardiogenic shock
|
- Reduced contractility (usually) due to ischaemia and infarction of myocardium (usually >40% of ventricle effected)
- Pump failure but adequate filling pressure - Low CO • Features of shock - High LVEDP (left ventricular end diastolic pressure) → venous congestion • Pulmonary congestion (due to ↑ pulmonary artery pressure) → Dyspnoea, hypoxaemia, crackles and wheezes in the chest • Pulmonary oedema and pleural effusion • Right ventricular failure → Raised JVP and dependant oedema |
|
|
Describe the management of a patient with cardiogenic shock
|
- Diagnosis
• Hx IHD, chest pain, ECG, troponin, enzymes - Treatment • Thrombolysis and anti-coagulants (as much more serious than an MI alone = 30% mortality) • Angiography → PTCA and stenting • Supportive measures → Oxygenation, analgesia, filling (as can also become hypovolaemic so need invasive monitoring = CVP or PCWP), cardiac support →inotrophic drugs can make situation worse as increase O2 demand for the myocardium but IABP doesn't have this effect and increased both perfusion and CO |
|
|
Describe the supportive measures that should be given in a patient in cardiogenic shock
|
- Oxygenation
• High concentration oxygen mask • (CPAP, IPPV) - Pharmacological – complex and controversial • Opioid analgesia • Diuretics • Drugs acting on vasomotor tone and contractility - Filling • IV fluids, guided by by CVP, PCWP, TOE - Mechanical support - controversial • IABP |
|
|
Give 3 causes of mechanical shock
|
1. Pulmonary embolism
2. Tension pneumothorax 3. Cardiac tamponade |
|
|
How can a pulmonary embolism cause mechanical shock?
|
- Large clot in pulmonary artery causes acute overloading of RV and hypovolaemia of LA and LV
- Features of shock with high venous pressure - Crushing central chest pain - Evidence of DVT may be present - May be very similar to cardiogenic shock but venous pressure increased only on the right side → increased JVP but no lung symptoms - ECG may help – SI QIII TIII - Diagnose with pulmonary angiography - Treatment – full resuscitation, anticoagulation, thrombolysis, surgery |
|
|
How may a tension pneumothorax cause mechanical shock?
|

- Valve mechanism allows air into pleural space but not out
• Increasing pressure collapses lung, then pushes mediastinum and heart to other side • Raised intrathoracic pressure and kinked great veins prevent cardiac filling • Features of shock with high venous pressure → high JVP - Diagnosis • Often young patient with history of sudden shortness of breath, possibly associated with trauma or asthma • Examination of the affected side shows poor expansion, absent breath sounds and tympanic percussion note; trachea and apex beat are shifted to opposite side - Treatment • immediate decompression with needle then chest drain with underwater seal |
|
|
How might cardiac tamponade cause mechanical shock?
|
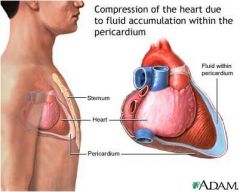
- Fluid collecting within indistensible pericardial sac compresses heart
- Heart cannot fill, so (again) features of shock with high venous pressure - Diagnosis • History of trauma or cardiac surgery, myocardial infarction, uraemia • Onset may be insidious causing heart failure • May be difficult to distinguish from cardiogenic shock • Echocardiography may help, exploration is definitive - Treatment • Sub-xiphoid pericardiocentesis, ideally with fluoroscopic (imaging) control • Surgical exploration |
|
|
Describe the pathophysiology of septic shock
|
- Inflammatory mediators associated with endotoxin release due to overwhelming sepsis (usually gram-negative) cause vasodilation, intravascular coagulation and loss of circulating volume through leaky capillaries
- Blood pools in dilated peripheries, reducing venous return and cardiac output (but CO may be normal or high) - Blood pressure (~CO x SVR) is reduced; particularly diastolic pressure, hence pulse pressure (difference between systolic and diastoloic pressure) may be increased - Myocardial depression and pulmonary hypertension may occur - Translocation of bacteria from ischaemic gut may occur |
|
|
Describe the early and late features of septic shock
|
- Early – warm shock
• Oxygen delivery may be adequate, but consumption may be low as disordered utilisation → SvO2 higher than normal • Vasodilated warm peripheries with rapid capillary refill, low venous pressure • Bounding or collapsing pulse • Tachycardia may be less marked than in hypovolaemic shock • Pyrexia and rigors - Late – cold shock • As for hypovolaemic shock • Myocardial depression (high venous pressure with fluid replacement) • Right heart failure as cytokines release cause vasodilation but bronchoconstriction → high pulmonary venous pressure → ARDS (adult respiratory distress syndrome) = very hard to breath |
|
|
Describe the management of septic shock
|
- General supportive measures
• Oxygenation – ARDS is common • Fluid replacement • Inotropic and vasoconstrictor support (adrenaline etc) - Early specific measures • Bacterial cultures • Antibiotics and surgical drainage - MOF (multi organ failure) is common and mortality is high |
|
|
What are the types of anaphylaxis?
|
1. Allergic
- IgE mediated - Non IgE mediated 2. Non-allergic |
|
|
Describe IgE mediated anaphylaxis
|
- Immediate or Type I hypersensitivity
- Foreign substance stimulates binds to IgE bound to mast cells and basophils - Further exposure causes de-granulation – release of mediators including histamine - These cause vasodilation and increased capillary permeability |
|
|
Describe the pathophysiology of anaphylaxis
|
1. Vasodilation
2. Capillary leak causing hypovolaemia 3. Myocardial depression may occur |
|
|
Describe the clinical presentation of anaphylaxis
|
- Usually within 30 min of exposure
- Cutaneous • Erythema, urticaria, oedema, pallor or cyanosis - Cardiovascular • Tachycardia • Hypotension - Respiratory • Rhinitis, bronchospasm, laryngeal obstruction, pulmonary oedema - GIT • Vomiting, diarrhoea, cramps |
|
|
Describe the managemet of anaphylaxis
|
- Oxygen
- Adrenaline - Fluids - CPR - Steroids, antihistamines |

