![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
50 Cards in this Set
- Front
- Back
|
What is the etiology of mitral stenosis
|
-Rheumatic
-Prosthetic valve dysfunction -Rare: myoma, mitral annular calcification -Elderly people, esp women, get calcification of the mitral annulus, the fibrous annulus that the mitral valve attaches to the cardiac skeleton with. If that calcification is robust enough it can extend into the leaflets and cause stenosis. Almost all stenosis is related to chronic rheumatic heart disease |
|
|
Describe the pathophysiology of mitral stenosis
|
-High LA pressure is needed to maintain flow across stenotic MV
-This leads to diastolic gradient across MV -Flow and gradient related by: -dP=(Flow/MVA)^2 -Flow=CO/(DFP*HR) DFP=Diastolic filling period |
|
|
Describe how mitral stenosis can lead to RV pressure overload
|
-Increased LA pressure -> increased PCWP -> Increases PAP -> RV pressure overload
-A chronic increase in PCWP -> pulmonary arteriolar constriction -> Increased PVR -> Further increase in PAP -> Increased RV pressure overload |
|
|
What are the symptoms of mitral stenosis?
|
-Dyspnea
-Fluid retention (edema, ascites, liver congestion, increased JVP) |
|
|
How does mitral stenosis lead to dyspnea?
|
-Exercise -> Increased flow
-Increased HR -> Increased flow (due to decreased diastolic time) -Increased flow -> increased gradient -> Increased LAP=Increased PCWP -> dyspnea |
|
|
How does mitral stenosis lead to fluid retention?
|
-Exercise-> Increased flow
-Increased HR -> Increased flow (due to decreased diastolic time) -Increased flow-> Increased gradient-> Increased LAP = Increased PCWP -Increased PCWP and increased PVR -> RV pressure overload -> Decreased RVEF and stroke volume -> decreased CO and increased RA pressure -Increased RA pressure and decreased CO -> fluid retention -> edema, ascites, liver congestion, increased JVP |
|
|
Describe the onset of symptoms with mitral stenosis
|
-Gradual and initially on exertion
-Rapid and abrupt if increased CO and HR Since rheumatic heart disease occurs gradually symptoms occur gradually. There is a gradual decrease in the threshold for dyspnea. That is less and less exertion produces symptoms. Symptom onset can be abrupt when there is a sudden big increase in flow. Here are the things that can produce it. -Fever/infection, pregnancy, anemia, hyperthyroid etc |
|
|
Describe the natural history of mitral stenosis
|
Over a period of 5-40 years there is:
-Acute rheumatic fever -Symptom onset -Severe disability -Death The time course depends on genetic factors and the availability of factors for prevention of recurrent episodes of strep infection. |
|
|
What are the components of the mitral apparatus?
|
-Mitral annulus
-Mitral leaflets-Anterior and Posterior -Chordae Tendineae -Papillary muscles -Left ventricle The mitral annulus has a muscular and a fibrous component, so it changes shape during systole. The mitral annulus is the ring that the leaflets are attached to. Chordaetendinae are fibrous strings that go from each valve leaflet to both papillary muscles. The papillary muscles attach the valve. |
|
|
Describe the etiology of acute MR
|
-Infectious endocarditis
-Spontaneous chordal rupture (myxomatous degeneration) -Papillary muscle rupture (acute MI) -Prosthetic valve failure |
|
|
Describe the etiology of chronic MR
|
-Same as acute
-MVP/Myxomatous degeneration -Rheumatic -Ischemic -Functional (dilated cardiomyopathy) Ischemia can produce regurgitation. If you have a heart attack part of the heart will no longer contract. If that is the part with the papillary muscle attachment then the papillary muscle will be pulled out of position. When the heart muscle is weak the heart muscle changes shape and the papillary muscles move away from each other and the valves can no longer come together. |
|
|
Describe the pathophysiology of acute MR
|
-Regurgitation into normal size and normally compliant LA
-Marked increase in LA pressure -Increased PCWP -> pulmonary congestion -CO =SV(1-RF)*HR; CO decreases because SV increase is limited by normal LV size and compliance -Sudden increase in PCWP may lead to increased PVR-> RV failure |
|
|
Describe the natural history of acute MR
|
-If severe -> pulmonary edema, death
-If LV systolic function abnormal -> shock, pulmonary edema, death If it is due to a heart attack affecting the papillary muscles it usually also involves the inferior wall of the heart. If thesystolic function of the heart is impaired by a heart attack then the stroke volume is diminished. One of the few compensations you have is taken away. If you then get MR you get severe low output. |
|
|
Describe the pathophysiology of chronic MR
|
-Eccentric hypertrophy allows large regurgitant volume to be accommodated at normal LV diastolic pressure (i.e. shift of LV diastolic P-V relationship)
-LA enlargement accommodates regurgitate volume at normal pressure -Ejection into LA provides decrease in afterload (i.e. extra preload is ejected into low pressure LA, no isovolumetric contraction period decreases systolic wall stress) -Usual measures (i.e. EF, ESD) of systolic function may be normal with abnormal contractiliy, and are greater than normal while myocardial contractility is maintained |
|
|
Describe the mechanism of pulmonary congestion in chronic MR
|
When systolic function worsens (decreased LVEF) -> further increase in LVEDV and LA pressure -> pulmonary congestion
|
|
|
What are the symptoms of MR?
|
LAP and CO (and therefore symptoms) are determined by:
1) Degree of MR 2) Rate of development of MR 3) LA compliance 4) LV compliance 5) LV systolic function 6) Afterload 7) Preload The symptoms are related to elevation of LA pressure causing dyspnea and decreases in CO (esp with exertion) causing fatique and exercise intolerance. It is extremely sensitive to loading conditions. |
|
|
Describe the natural history of chronic MR
|
Structural MR
-Onset of symptoms of fall of LVEF into normal range mark transition to development of irreversible LV dysfunction, CHF, and death over several year period Functional MR -National history tied to underlying disease (i.e. dilated CM, ischemic heart disease) The normal range for this lesion is abnormal. That indicates irreversible heart failure and can lead to death. The natural history of function MR is determined not by the mitral regurgitation but the natural history of the heart muscle disease. |
|
|
What predicts long term survival with chronic MR?
|
-EF > 60%
-Class I or II vs II or IV |
|
|
What mechanical treatments are available for valvular disease?
|
Prosthetic heart valves
-Mechanical (durable, thrombogenic) -Tissue (less durable, less thrombogenic) -Repair preferred Percutaneous treatments -Balloon valvuloplasty for MS, PS -Mitral repair -Aortic and pulmonic valve replacement |
|
|
Describe acute rheumatic fever
|
-Immunologically mediated
-Following 1-6 weeks after pharyngitis with Group A Streptococcus in 3% of those infected -Antibodies against streptococcal M proteins cross-react with similar antigenic determinants in joints, heart, skin, CNS |
|
|
What are the major manifestations for acute rheumatic fever?
|
1. Migratory polyarthritis (75%)
2. Carditis (50%) 3. Sydenham's chordia (10% - involuntary, rapid, purposeless movements - caudate) 4. Erythema marginatum of skin (10% - brown/pink with pale center) 5. Subcutaneous nodules (0.5-2cm; extensor surfaces, occur late) |
|
|
What is needed for acute rheumatic fever diagnosis?
|
-2 major manifestations
OR -1 major manifestation and 2 minor |
|
|
What are the minor manifestations of acute rheumatic fever?
|
-Previous rheumatic fever
-Arthralgia -Fever -Increased ESR or CRP -Prolonged P-R interval Supportive evidence of streptococcal infection: ASO Ab, anti-DNAase B, positive throat culture |
|
|
What is the prognosis of acute rheumatic fever?
|
1% mortality due to cardiac issues
|
|
|
Describe the pancarditis of acute rheumatic fever
|
-Pericarditis
-Myocarditis (Aschoff body) -Endocarditis with sterile vegetations |
|
|
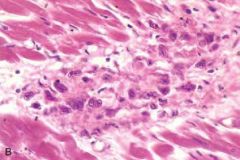
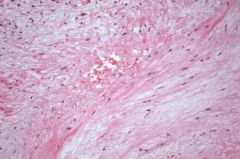
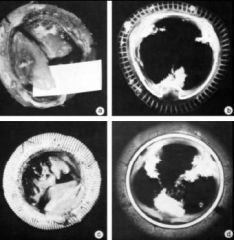
-Aschoff body of acute rheumatic carditis
-A cardiac granuloma -In the myocardium -A nodular aggregate of tissue macrophages (histocytes) -In active phase of disease there can be necrosis |
|
|
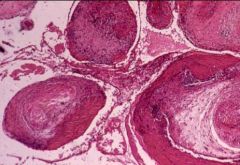
-Mitral stenosis
-Involvement of the endocardium -Mitral valve chordae tendinae cut in cross section -Pink is fibrin -Blue dots are inflammatory cells -Active endocardial inflammation as part of part of this autoimmune attack -This is the active acute rheumatic endocardial involvement. |
|

|
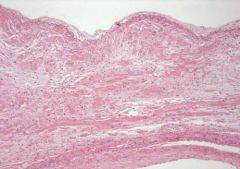
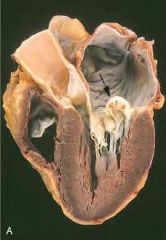
-Mitral stenosis
-How you heal after active acute rheumatic endocardial involvement. -Healed after an active endocardial inflammation as part of this autoimmune attack -The chordae tendanae are bound together by all this extra tissue. -When it repairs it heals with this fibrosis. In the acute reaction these things get stuck together and when it heals they all end up fused together. |
|
|
Describe chronic rheumatic heart disease
|
-Follows acute rheumatic heart disease by decades
-MV 65-70% -MV and AV 25% -Mitral stenosis, aortic stenosis -Arrhythmias (A. fib with left atrial enlargement) -Heart failure -Predisposed to infective endocarditis -People who have repeated bouts of acute rheumatic fever are more likely to have rheumatic heart disease -People who had very severe attacks are more likely to develop chronic heart disease -Penicillin prophylaxis against rheumatic fever can be effective |
|
|
Describe the relationship between mitral stenosis and atrial fibrillation
|
-With mitral stenosis the LA enlarges
-Frequency of atrial fibrillation is directly related to the size of the LA |
|
|
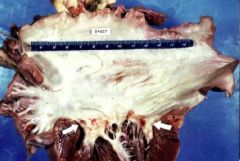
-Severe form of chordae tendinae thickening
-Massive dilation of the LA -White tissue is a massive fusion of all the tendinae -Fused, thickened, shortened tendinae are the classic presentation of rheumatic heart disease -No Aschoff bodies |
|

|
"Fishmouth" deformity from chronic rheumatic heart disease of the mitral valve disease
|
|
|
Describe mitral valve prolapse
|
-Most are asymptomatic
-Mid-systolic click -Rarely: chest pain, dyspnea, fatigue, or psychiatric manifestations -~3% have complications: Infective endocarditis Mitral insufficiency Thrombus formation with embolization Arrhythmia/sudden death (unknown mechanism) |
|
|
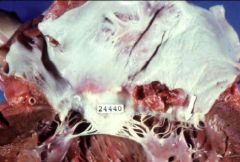
-Myxomatous, prolapsing mitral valve
-The disturbance in this myxoid degeneration or mitral prolapse is that it never formed properly -Pale stuff is irregularly distributed -Valve leaflet is markedly thickened and not organized -Valve is weaker, stretches, and prolapses |
|
|
-"Myxomatous" mitral valve
-There are spindle cells -The blue-gray substance of abnormally formed mitral valves is present |
|
|
-Valve is prolapsing into the atrium
-Myxoid degeneration can extend down into the chordae and weaken them -The pressure with valves snapping out in mid-systole can cause them to rupture - The abrupt onset of severe mitral regurgitation in someone who had a mid-systolic click and was asymptomatic is usually due to a rupture of the chord because of the same abnormal morphology. |
|

|
-Bacterial Endocarditis
-Abnormal valves can have sterile platelet fibrin thrombi -Bacteria can seed previously sterile platelet thrombin -Tissue destruction and large vegetations form -Valve destruction leads to insufficiency |
|

|
-Bacterial endocarditis
-Destroys underlying valves -Vegetations can embolize to other organs -Antibody-antigen immune complexes can deposit in organs such as skin and kidneys |
|
|
Bacterial endocarditis lesions can heal. These vegetations have coalesced and firmed
|
|
|
Describe non-bacterial thrombotic endocarditis (NBTE)
|
-Small (1-5mm) sterile masses of fibrin on lines of closure
-Hypercoagulable state: patients are often debilitated ("marantic" endocarditis) or may have malignancy (mucinous adenocarcinoma), renal failure, sepsis -May embolize to brain, kidney, heart -With bacteremia, may be converted to infectious endocarditis |
|

|
-Non-bacterial thrombotic endocarditis
-Tiny lesions are much smaller than the big lesions of infective endocarditis |
|
|
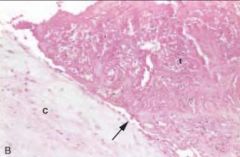
-Non-bacterial thrombotic endocarditis (NBTE)
-This is the valve and thrombin -No organism and no inflammation -Thrombin can break off and embolize |
|

|
-Rupture of mitral valve papillary muscle causing MR
-There is a break where the myocardium has weakened due to infarct and has just ruptured |
|
|
What are the complications of heart valve prostheses?
|
-Mechanical: component failure
-Bioprosthesis: degeneration with calcification -Both: paravalvular leak, endocarditis Thrombosis and tissue overgrowth are less common in bioprostheses tan in mechanical valves |
|

|
-Bioprosthetic valve
-Degeneration and tissue overgrowth |
|
|
-Valve has ruptured
-X-ray shows calcification |
|

|
-AV prosthesis with thrombus (from aortic side)
|
|

|
-Tissue overgrowth of MV prosthesis
|
|

|
Tissue overgrowth of MV prosthesis (from atrial side)
|
|

|
Endocarditis of ball valve prosthesis
|

