![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
What percentage of adult population has a mental disorder?
|
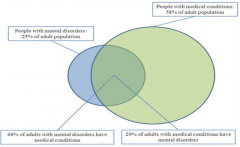
25%
|
|
|
What percentage of adult population has a medical condition?
|
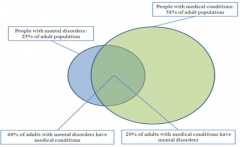
58%
|
|
|
What percentage of adult population with a mental disorder, also has a medical condition?
|
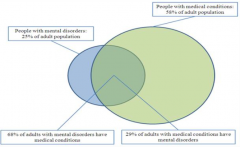
68%
|
|
|
What percentage of adult population with a medical condition, also has a mental disorder?
|
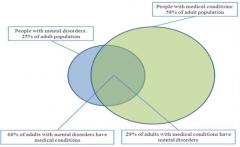
29%
|
|
|
How does depression relate to cardiac disease?
|
- Depression is associated w/ higher numbers of cardiac risk factors
- Associated w/ increased mortality post-MI |
|
|
What are some causes of increased morbidity and mortality from CVD in patients w/ depression?
|
Behavioral Risk Factors:
- Treatment non-adherence - Lifestyle factors (smoking, lack of exercise, diet, etc.) - Personality types (A and D) Physiologic Risk Factors: - ANS dysfunction (loss of HR variability) - Inflammation / platelet reactivity - Hypothalamic Pituitary Adrenal (HPA) axis dysregulation (chronically elevated cortisol) |
|
|
How does depression compare to LVEF and prior MI as a predictor of morbidity and mortality?
|
Impact of depression on prognosis was as relevant as LVEF and prior MI (3-4x adjusted relative risk)
|
|
|
How does depression affect a patient without CAD?
|
Presence of depression in individuals without CAD may lead to the development of CAD in the future (1.5-2x adjusted relative risk)
|
|
|
What are the cause of Takotsubo CM? Outcomes?
|
- Triggered by emotional or physical stress
- In absence of significant CAD - Transient apical and mid-ventricular LV dysfunction |
|
|
What are the clinical findings of Takotsubo CM?
|
- Sudden onset chest pain or shortness of breath
- ECG changes suggest MI along w/ mild to moderate elevation of cardiac biomarkers - No evidence of obstructive CAD on cath - "Octopus pot" morphology on echo - Complete resolution of LV dysfunction weeks after event |
|
|
How common is Takotsubo CM? Mortality? Who is more likely to get it?
|
- ~2% of suspected ACS
- In hospital mortality ranges 0-8% - More common in women (~90%), especially post-menopausal women (>80%) - Mean age: 58-75 years |
|
|
What are the triggers of Takotsubo CM? What does this cause?
|
- Death of loved one
- Devastating financial losses - Natural disasters - Physical illness / ICU - Leads to excess Catecholamines (NE elevated ~75%) - May induce microvascular spasm or dysfunction → myocardial stunning or direct myocardial toxicity |
|
|
Which β-blockers can pass the BBB? Significance?
|
- Lipophilic drugs: Carvedilol, Metoprolol, Propranolol
- May be linked to depression (although more studies fail to find an increase in rates of depression) - Other CNS adverse events have been linked to them: drowsiness, fatigue, lethargy, and sleep disorders |
|
|
What is the concept of Metabolic Syndrome?
|
Group of cardiometabolic risk factors associated with insulin resistance
|
|
|
What are the criteria for diagnosis of Metabolic Syndrome?
|
3 of 5 criteria:
- Waist: M > 40 inches, F >35 inches - BP: ≥ 130/85 mmHg - HDL: M <40 mg/dl, F <50 mg/dl - TG: ≥ 150 mg/dl - Glucose: ≥ 100 mg/dl |
|
|
How prevalent is Metabolic Syndrome by gender?
|
- Much more common in females (50%)
- 35% of males |
|
|
How does schizophrenia relate to post-MI mortality? Why might this be?
|
- 34% increased risk of mortality following MI
- Schizophrenic patients do not receive adequate treatment of dyslipidemia, HTN, DM |
|
|
What features of schizophrenia make them at increased risk for metabolic syndrome?
|
- Suspicion
- Stigma - Negative symptoms - Executive dysfunction - Anti-psychotic medications - Sedentary lifestyle - Lack of regular physical activity - Poor food intake - Substance use - High rates of smoking |
|
|
Which anti-psychotics cause the greatest increase in proportion of patients meeting criteria for metabolic syndrome?
|
- Olanzapine
- Clozapine |
|
|
How do anti-psychotics affect weight?
|
Some (especially Olanzapine and Clozapine) tend to show weight gain that slows after first year of treatment
|
|
|
What are the risk factors for anti-psychotic induced weight gain?
|
- Younger age
- Lower initial BMI - Personal or family history of obesity - Non-white ethnic background - Cannabis use |
|
|
What are the potential mechanisms of weight-gain due to anti-psychotics?
|
Receptors most frequently associated with weight gain:
- Serotonin 2C (5HT2C) - Histamine 1 (H1) |
|
|
Which anti-psychotic drug is best in terms of not causing weight gain?
|
- Ziprasidone
- Aripiprazole |
|
|
What modifiable risk factors should be evaluated in patients at risk of CV and metabolic diseases?
|
- Weight
- BMI - Waist circumference - Fasting lipids - Fasting glucose - BP |
|
|
What is the overall incidence rate of new onset Diabetes within 3 months of anti-psychotic therapy initiation?
|
4%
|
|
|
What problems do anti-psychotics possibly cause with glucose regulation?
|
- Diabetes Mellitus Type II: related to anti-psychotic induced weight gain and adiposity's effect on insulin secretion
- Diabetic Ketoacidosis (DKA): may be direct effect of some anti-psychotic medication on tissue insulin sensitivity or pancreatic beta-cell function |
|
|
How do anti-psychotics cause abnormal glucose regulation leading to Diabetes Mellitus type II?
|
- Adiposity levels are highly predictive of level of insulin sensitivity
- ↑ Adiposity → ↓ Insulin Resistance - Risk of diabetes during anti-psychotic tx generally follows rank order for wt gain |
|
|
How do anti-psychotics cause abnormal glucose regulation leading to Diabetic Ketoacidosis?
|
- Antagonize M3 cholinergic receptors
- Muscarinic M3 cholinergic receptors are located on pancreatic beta cells - Antagonism of M3 cholinergic receptors in pancreatic beta cells, releases insulin resistance |
|
|
How does a decrease in blood cholesterol affect CVD?
|
- Reduce blood cholesterol by 10% minimum with 30% decrease in risk of CHD
- Decreased diastolic BP of 6 mmHg in patients w/ BP >90 mmHg → ↓CHD and 42%↓ in stroke |
|
|
Which phase of the myocardial AP do anti-psychotics affect?
|
Phase 3: repolarization by opening of fast K+ rectifier channels (outward K+ flow)
|
|
|
How do you quickly and easily determine if the QT interval is normal?
|
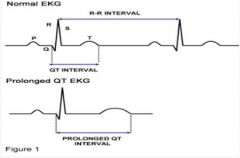
Use rule of thumb that normal QT is less than half the RR interval
|
|
|
How do you measure the QT interval? Which leads?
|
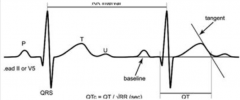
- Use lead II or V5 (these give you the best T waves)
- Draw a line tangent to steepest slope of T wave so that it crosses baseline (tangent) - Measure from first dip of Q wave to tangent = QT interval - Corrected QT interval: QTc = QT / √RR |
|
|
What are the risks of having a prolonged QTc interval?
|
- ↑ Risk of Torsades de Pointes
- Surrogate marker to predict drug-related cardiac morbidity and mortality |
|
|
What is a normal QT interval for men and women?
|
- Men: <440 msec
- Women: <450 msec |
|
|
What is a "highly abnormal" QT interval?
|
>500 msec for males or females
|
|
|
What are some non-modifiable risk factors for prolonged QT interval?
|
- Genetics (LQTS)
- Age >65 yo - Female Gender - Circadian Rhythm - CV Disease |
|
|
What are some modifiable risk factors for prolonged QT interval?
|
- Bradycardia (check if β-blockade is too high)
- Electrolyte Abnormalities (hypomagnesemia, hypokalemia) - Pharmacologic (check what drugs they are that may prolong QT) |
|
|
What causes Long QT Syndrome? Risks?
|
- Mutations in K+ channels (KCNQ1 and KCNH2) and others (Na+ channels too)
- Causes 3000-4000 deaths/year - Much more susceptible to drug-induced TdP (5-20% of cases) |
|
|
What channel is most often inhibited in acquired (or drug-induced) QT prolongation? Gene? Function?
|
HERG K+ channel
- KCNH2 encoded - Mediates the rapid component of the delayed-rectifier K+ current (Ikr) |
|
|
How do drugs that bind to the HERG K+ channel affect it? Outcomes?
|
- Inhibits outward K+ current (Ikr)
- Prolongs phase 3 of ventricular myocyte's AP duration - Lengthens QT interval |
|
|
What is Torsades de Pointes? How fast is rate?
|
- Polymorphic Ventricular Tachycardia
- Change in amplitude and morphology (ie, twisting) of QRS - Ventricular rate: 160-240 bpm |
|
|
What are the symptoms of a patient with Torsades de Pointes?
|
- Asymptomatic
- Self-limited dizziness, palpitations, or syncope - Sudden cardiac death - Usually short-lived and terminates spontaneously |
|
|
Which drugs have the greatest effect on prolonging the QT interval?
|
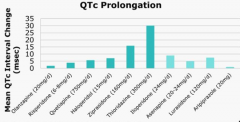
- Thioridazine
- Ziprasidone |

