![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
What are the layers of the pericardium?
|
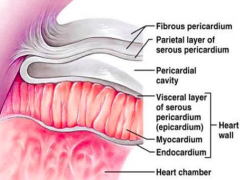
- Visceral
- Parietal |
|
|
What is the histological organization of the Visceral Pericardium? Function?
|
- Membrane composed of single layer of mesothelial cells
- Adheres to epicardial surface of heart |
|
|
What is the histological organization of the Parietal Pericardium? Function?
|
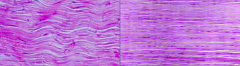
- Fibrous layer 2 mm in thickness, containing collagen and elastic fibers
- Collagen contains wavy bundles (low level of stretch) and Streight bundles (high levels of stretch) |
|
|
What is the relationship between the visceral and parietal pericardium?
|
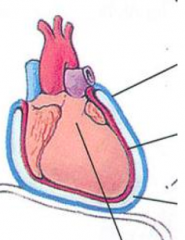
- Visceral pericardium reflects back near the origin of the great vessels and becomes the parietal pericardium
- Space contains 50 mL serous fluid |
|
|
What parts of the heart are extra-pericardial?
|
Part of posterior wall of LA
|
|
|
What structures stabilize the pericardium?
|
- Diaphragm
- Sternum - Spine |
|
|
What nerve is enveloped by the parietal pericardium?
|
Phrenic nerves
|
|
|
What can happen when the phrenic nerve is irritated?
|
Hiccups
|
|
|
What causes hiccups?
|
Irritation of phrenic nerve
|
|
|
What are the functions of the Pericardium?
|
- Maintains heart position
- Lubricates visceral and parietal layers - Barrier to infection - Prostaglandin secretion (modulates coronary vascular tone) - Restraining effect on cardiac volume (small reserve volume) |
|
|
What does the pericardium secrete? Function?
|
Prostaglandins - modulates coronary vascular tone
|
|
|
How does the pericardium affect the cardiac volume?
|
Restraining effect on cardiac volume:
- Mechanical properties of pericardial tissue - Small reserve volume - Tensile strength similar to rubber |
|
|
How does the stretchability of the pericardium depend on the cardiac volume? Implications?
|
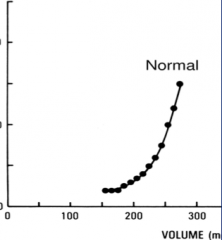
- Normal cardiac volume: more elastic - stretches easily
- Increased cardiac volume: pericardium becomes stiff - resistant to further stretch *In a pericardial effusion, once critical volume of effusion is reached, small additional amounts lead to a large increase in intra-pericardial pressure - Removal of a small amount of fluid leads to significant improvements of pressure |
|
|
How does the pericardium adapt to cardiac dilatation?
|
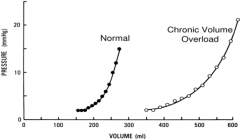
- Acutely, increasing volume can lead to significant increases in pressure
- Chronically, leads to adaptations to accommodate increased volume; pericardial growth occurs in response to chronic stretch - PV curve shifts to the R w/ decreased slope (less increased P d/t increase V) |
|
|
What are the implications of chronic cardiac dilation?
|
- Pericardium grows in response to the chronic stretch
- Slowly accumulating pericardial effusions can become very large before becoming symptomatic (as in hypothyroidism) |
|
|
What can cause a slowly accumulating pericardial effusion?
|
Hypothyroidism
|
|
|
What are the causes of acute pericardial inflammation?
|
* Majority (80-90%) are idiopathic
* Most assumed to be viral (routine testing of specific viral agents is not done because of cost and rarely alters management) - Other infections (bacterial, myobacterial) - Radiation - Blunt / penetrating trauma - CT disorder (SLE, RA, systemic sclerosis) - Post-MI or Dressler Syndrome |
|
|
What are the characteristic symptoms of Acute Pericarditis?
|
- Chest pain almost always present (moderate to severe intensity)
- Relieved when sitting down, worse when lying down - Sharp, pleuritic pain - Substernal, epigastric, L chest, trapezius muscle area (specific for pericarditis) |
|
|
What are the possible differential diagnoses for chest pain that is felt in Acute Pericarditis?
|
– Pneumonia with pleurisy (Pleuro-pericarditis) – PE with infarction
– Costochondritis – GERD – Intraabdominal processes – Aortic dissection – Pneumothorax – Herpes Zoster (before skin lesions) – Myocardial ischemia/infarction |
|
|
What physical exam findings indicate Acute Pericarditis?
|
- Fever, tachycardia, anxiety (not always present)
- Pericardial friction rub (best heard at L LSB w/ patient leaning forward) |
|
|
What is a "Pericardial Friction Rub" caused by? Physical exam findings?
|
- Cause: contact between parietal and visceral pericardia
- 3 components: ventricular systole, diastole, atrial contraction - Best heard at L LSB, w/ patient leaning forward - Dynamic (similar to EKG) - Disappearing / returning over short periods of time |
|
|
How sources of information do you use to diagnose Acute Pericarditis?
|
- Symptoms (history)
- Exam findings (physical) - ECG - Echo not necessary for diagnosis |
|
|
What are the ECG findings associated w/ Acute Pericarditis?
|

Dynamic (like rub)
ST segment elevation - Diffuse (not in leads aVR, V1) - Occasionally focal (trauma and post-op) - ST segment concave - No reciprocal changes Upright T waves *PR depression (elevation in aVR) - may be the only ECG finding |
|
|
What are the differences between ST elevation in STEMI vs Acute Pericarditis?
|
- STEMI: localized ST elevation (not in all leads)
- AP: diffuse presentation (except not present in aVR and V1), ST segment is concave *AP may have focal ST elevation in post-op or traumatic presentation |
|
|
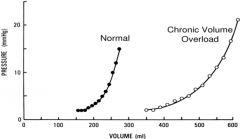
What are the stages of Pericarditis on EKG?
|
Stages I, II, III, IV
|
|
|
What are the features of Stage I?
|
- Diffuse, concave ST-segment elevation
- Early on ST elevation may be focal and mimic AMI |
|
|
What are the features of Stage II?
|
- ST segments normalize, w/ J point returning to baseline
- T-wave amplitude begins to decrease - PR depression (which may make it appear as though there is continued ST elevation) |
|
|
What are the features of Stage III?
|
- T wave inversions develop diffusely (may be quite deep)
- No PR depression or ST elevation |
|
|
What are the features of Stage IV?
|
- EKG abnormalities again normalize
- T-wave inversions may become permanent |
|
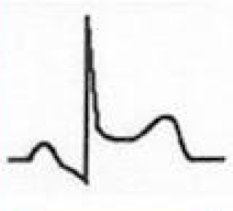
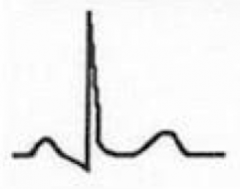
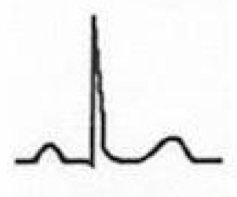
What does this EKG represent? Features?
|
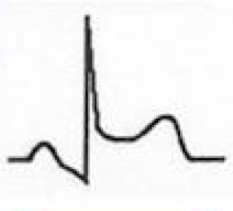
Stage I of Pericarditis
- Diffuse, concave ST-segment elevation - Early on ST elevation may be focal and mimic AMI |
|
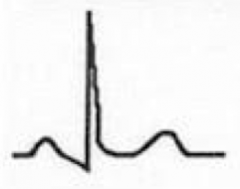
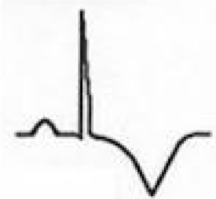
What does this EKG represent? Features?
|
Stage II of Pericarditis
- ST segments normalize, w/ J point returning to baseline - T-wave amplitude begins to decrease - PR depression (which may make it appear as though there is continued ST elevation) |
|

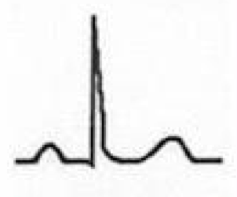
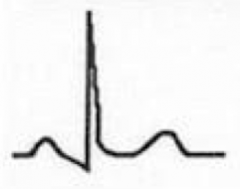
What does this EKG represent? Features?
|

Stage III of Pericarditis
- T wave inversions develop diffusely (may be quite deep) - No PR depression or ST elevation |
|
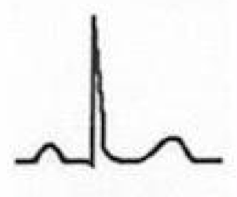
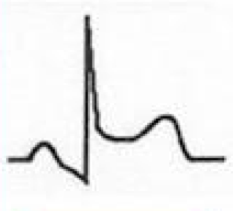
What does this EKG represent? Features?
|
Stage IV of Pericarditis
- EKG abnormalities again normalize - T-wave inversions may become permanent |
|
|
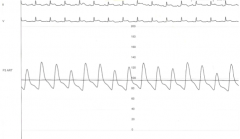
What are "electrical alternans"? Cause?
|

- Alternation between large and small QRS complexes
- Sign of pericardial effusion |
|
|
What are the lab findings for Acute Pericarditis?
|
Idiopathic "Viral" Pericarditis (rather non-specific)
- Mildly elevated WBC count w/ lymphocytes - Mildly elevated ESR |
|
|
What are some secondary causes of the lab findings of acute pericarditis?
- Mildly elevated WBC count w/ lymphocytes - Mildly elevated ESR |
- Significant WBC elevation w/ left shift
- Anemia, elevated ESR (CT disorder) - Elevated ESR (CT disorder, TB) |
|
|
How do chest x-ray findings affect your diagnosis of Acute Pericarditis?
|
- Usually normal in uncomplicated pericarditis
- Abnormal CXR finding considered secondary disorders (pleural effusions, infiltrates, mass lesions, CHF) |
|
|
How do Echo results affect your diagnosis of Acute Pericarditis?
|
- Not required for diagnosis and management of idiopathic pericarditis
- Small, otherwise clinically silent, effusion not uncommon - Large effusion considered secondary disorder |
|
|
Is a large effusion expected for Acute Pericarditis?
|
- No - this is probably a secondary disorder (secondary pericarditis)
- However, a small, clinically silent effusion, is not uncommon for primary pericarditis |
|
|
How should you treat Acute Pericarditis?
|
Acute idiopathic "viral" pericarditis:
- Uneventful recovery in 70-90% - Treat w/ NSAIDs (post MI, use Aspirin) ** Best: Treat w/ Colchine (w/ NSAIDs or as alternative to NSAIDs) - Treat w/ Steroids Secondary Pericarditis - Identify and treat secondary disorder |
|
|
What are the pros and cons of using Colchicine for Acute Idiopathic ("Viral") Pericarditis?
|
Pros:
- Decreased incidence of recurrent pericarditis - Anti-inflammatory - Preferential concentration in leukocytes (16x higher peak conc. than in plasma) Cons: - Discontinuation rate 10-15% (d/t GI side effects) |
|
|
What are the pros and cons of using Steroids for Acute Idiopathic ("Viral") Pericarditis?
|
- Rapid response to treatment
- May encourage relapses (avoid if possible) |
|
|
Which tx for acute pericarditis decreases relapses? Increases relapses?
|
- Decreased relapses: colchicine
- Increased relapses: steroids |
|
|
What is the mechanism of Colchicine?
|
- Disrupts microtubules / inhibits microtubule self-assembly
- Takes place in mitotic spindle or in interphase stage * Inhibits movements of intercellular granules and secretion of various substances in leukocytes |
|
|
What were the conclusions of the COPE (Colchicine for acute Pericarditis) trial?
|
- Colchicine + conventional therapy led to a clinically important and statistically significant benefit over conventional therapy alone
- Decreased the recurrence rate by 50% (Conventional therapy: aspirin, ibuprofen, or glucocorticoids) |
|
|
What criteria are necessary to diagnose Acute Pericarditis?
|
Two of the following:
– Typical chest pain (sharp and pleuritic, improved by sittng up and leaning forward) – A pericardial friction rub – Suggestive changes of on ECG (widespread ST-segment elevation or PR depression) – New or worsening pericardial effusion |
|
|
What criteria are necessary to diagnose Incessant Pericarditis?
|
Persistent pericarditis w/ symptom-free intervals of less than 6 weeks duration
|
|
|
What were the conclusions of the ICAP (Investigation on Colchicine for Acute Pericarditis) trial?
|
When colchicine is added to conventional therapy, it significantly reduced the rate of incessant or recurrent pericarditis
|
|
|
What are some non-inflammatory causes of pericardial disease ?
|
- Hydropericardium: accumulation of serous transudate in pericardial space (assoc. w/ CHF, hyponatremia, or chronic kidney or liver disease)
- Hemopericardium: accumulation of blood in pericardial sac (assoc. w/ trauma of heart or aorta; or myocardial rupture after acute MI) |
|
|
What happens in Hydropericardium? What is it associated with?
|
- Accumulation of serous transudate in pericardial space
- Assoc. w/ CHF, hyponatremia, or chronic kidney or liver disease |
|
|
What happens in Hemopericardium? What is it associated with?
|
- Accumulation of blood in pericardial sac
- Assoc. w/ trauma of heart or aorta; or myocardial rupture after acute MI |
|
|
What is the most common cardiac manifestation of HIV infection?
|
Pericardial Effusion - most are small, asymptomatic, and idiopathic
|
|
|
What is the relationship between HIV and Pericardial disease?
|
- 20% of HV patients develop pericardial involvement
- More common pre-HAART - Pericardial effusion is the most common cardiac manifestation of HIV infection - Seen in more advanced stages of disease (greater mortality risk) - Most effusions are small, asymptomatic, and idiopathic |
|
|
What can cause large effusions in HIV patients?
|
- Infection (MT, MAI, CMV, Cryptococcus)
- Neoplasm (Kaposi Sarcoma, Lymphomas) |
|
|
How do you treat pericardial effusions in HIV patients?
|
Treat underlying cause
|
|

If you have a patient presenting w/ ST elevation on EKG, what should you do?
|
Send them to the cath lab - it might just be acute pericarditis, but it could be ACS
|
|
|
What is Pulsus Paradoxicus?
|
Variation of systolic pressure by >10 mmHg (consistent w/ pericardial effusion)
|

