![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
What are relatively common outcomes of arrhythmias?
|
- Syncope
- Sudden cardiac death (SCD) - Sudden infant death syndrome (SIDS) |
|
|
How common is Long QT Syndrome?
|

1:2000 - 5000
|
|
|
What genetic abnormality can lead to Long QT Syndrome?
|

Mutations in ion channel genes that either cause:
- Influx of Na+/Ca2+ - Decrease K+ in cardiac cells --> shift of electrical AP and repolarization effects |
|
|
What are the criteria for diagnosis of Long QT Syndrome by gender?
|

Identified by prolonged QT interval on EKG:
- >450 ms in males - >470 ms in females Borderline QT interval: - 431-450 in males - 451-470 in females * Approx. 30-40% of LQTS carriers have a QT interval equal to that of normal individuals * |
|
|
What is the normal QT interval by gender?
|
- <430 ms in males
- <450 ms in females |
|
|
What are the symptoms of Long QT Syndrome?
|
- Syncope (esp. during exercise or high emotions)
- Sudden Cardiac Death - Due to ventricular tachyarrhythmias, typically Torsades de Pointes (TdP) - TdP may cause seizures |
|
|
What are people with Long QT Syndrome most likely to pass out? Least likely?
|
- Most likely: exercise and high emotions
- Least likely: rest or sleep (although can be a trigger in certain mutations for Romano-Ward Syndrome) |
|
|
What are acquired factors that can cause QT prolongation?
|
- Primary myocardial problems: MI, myocarditis, cardiomyopathy
- Electrolyte abnormalities: hypokalemia, hypomagnesemia, hypocalcemia - Autonomic influences - Drug effects - Hypothermia |
|
|
What are some inherited syndromes that cause Long QT Syndrome?
|
- Romano-Ward Syndrome (RWS)
- Jervell and Lange-Nielson Syndrome (JLNS) |
|
|
What happens in Romano-Ward Syndrome (RWS)? Cause?
|
- Elecrophysiologic disorder that causes QT prolongation and T-wave abnormalities
- Autosomal dominant inheritance - 10 genes associated with it including: KCNQ1, KCNH2, SCN5A |
|
|
Which genetic syndrome is associated with QT prolongation and T-wave abnormalities?
|
Romano-Ward Syndrome (RWS)
|
|
|
What are the most common genes that are mutated in Romano-Ward Syndrome (RWS)? How common is each one? What ions do they affect?
|
- KCNQ1 (LQTS Type 1) = >60% - K+
- KCNH2 (Type 2) = 35% - K+ - SCN5A (Type 3) = <5% - Na+ |
|
|
What happens in Jervell and Lange-Nielson Syndrome (JLNS)? Cause?
|
- Causes QT prolongation and profound, bilateral sensorineural deafness
- Presentation: deaf child w/ syncopal episodes during periods of stress, exercise, or fright - Increased risk of SIDS in children - Autosomal recessive - 2 genes associated with it: KCNQ1 and KCNE1 |
|
|
Which genetic syndrome is associated with a deaf child that experiences QT prolongation causing syncopal episodes during periods of stress, exercise, or fright?
|
Jervell and Lange-Nielson Syndrome (JLNS)
|
|
|
What are the most common genes that are mutated in Jervell and Lange-Nielson Syndrome (JLNS)? How common is each one? What ions do they affect?
|
- KCNQ1 (LQTS Type 1) = 90% - K+
- KCNE1 (LQTS Type 5) = 10% - K+ |
|
|
How are the inherited forms of Long QT Syndrome inherited?
|
- Romano-Ward Syndrome: Autosomal Dominant (KCNQ1 or KCNH2 or SCN5A mutations)
- Jervell and Lange-Nielson Syndrome: Autosomal Recessive (KCNQ1 or KCNE1 mutations) |
|
|
If your patient is diagnosed with Romano-Ward Syndrome (RWS), what is the chance that a 1st degree relative also has RWS?
|
50% (autosomal dominant inheritance)
|
|
|
What is the most common mutation (cause of >60%) that causes Romano-Ward Syndrome (RWS)?
- Incidence of cardiac event? - Cardiac event triggers? - Sudden cardiac death risk? |
KCNQ1 (LQTS Type 1)
- 63% incidence of cardiac events - Triggers: exercise, sudden emotion, swimming - 4% risk of SCD |
|
|
What is the second most common mutation (cause of 35%) that causes Romano-Ward Syndrome (RWS)?
- Incidence of cardiac event? - Cardiac event triggers? - Sudden cardiac death risk? |
KCHN2 (LQTS Type 2)
- 46% incidence of cardiac events - Triggers: exercise, emotion, postpartum, sleep - 4% risk of SCD |
|
|
What is the third common mutation (causes <5%) that causes Romano-Ward Syndrome (RWS)?
- Incidence of cardiac event? - Cardiac event triggers? - Sudden cardiac death risk? |
SCN5A (LQTS Type 3)
- 18% incidence of cardiac events - Triggers: sleep - 4% risk of SCD |
|
|
Which mutations can predispose someone to have prolonged QT syndrome during their sleep? What syndrome does this correspond to?
|
- KCHN2 = RWS
- SCN5A = RWS |
|
|
If someone has a mutation for KCNQ1, what are they at risk for?
|
- Romano-Ward Syndrome (RWS)
- Jervell and Lange-Nielson Syndrome (JLNS) - Prolongs QT interval in both - RWS also has T-wave abnormalities - JLNS also causes sensorineural deafness |
|
|
What indications should cause you to evaluate for Long QT Syndrome?
|
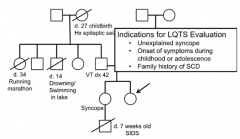
- Unexplained syncope
- Onset of symptoms during childhood or adolescence - Family history of SCD |
|
|
When should you do genetic testing for Long QT Syndrome?
|
- Molecular confirmation of clinical diagnosis in symptomatic individuals
- Risk assessment of asymptomatic family members of a proband w/ arrhythmia - Differentiation of hereditary arrhythmia from acquired arrhythmia - Recurrence risk calculation |
|
|
What is the current genetic testing detection rate for Long QT Syndrome?
|
- 75% will be positive for a mutation we know of
- 25% of families w/ a clinical diagnosis of LQTS will not have a detectable gene mutation |
|
|
If a family has a negative genetic test for LQTS, what should you tell them?
|
- This does not rule out Long QT Syndrome
- Large deletions and duplications may be present in LQTS genes - 25% of families will have a clinical diagnosis without a detectable mutation - 5-12% of patients w/ normal sequencing of most common LQTS genes had large genomic rearrangements |
|
|
What percent of people with hereditary Long QT Syndrome will have 2 mutations?
|
Up to 10%
|
|
|
What are the genetic test to assess for Long QT Syndrome? Main difference?
|
- Single gene analysis - assesses one gene at a time
- Arrhythmia gene panel - assesses multiple genes simultaneously |
|
|
What is done in a single gene analysis for Long QT syndrome?
|
- Exon sequencing evaluates mutations in one gene
- In the event of a negative result, CGH array can assess full exon deletions or duplications |
|
|
What is done in a arrhythmia gene panel for Long QT syndrome?
|
- Massive parallel sequencing (NextGeneration Sequencing) of coding exons within multiple genes simultaneously
- In the event of a negative result, CGH array can assess full exon deletions or duplications |
|
|
What is variable expressivity?
|
- Extent to which genotype is phenotypically expressed (physical signs and symptoms)
- Phenotype associated w/ same genotype may vary from MILD to SEVERE within families |
|
|
What is Reduced Penetrance?
|
Less than 100% of individuals with a certain genotype actually express the phenotype (ALL or NOTHING)
|
|
|
What are the mechanisms of Tachycardia?
|
- Re-entry
- Enhanced automaticity - Abnormal automaticity - Triggered activity |
|
|
What are the types of triggered activities that cause tachycardias?
|
- Abnormal cellular firings which can be triggered by pacing
- Early and Delayed After-Depolarizations (EAD and DAD) |
|
|
What are early after-depolarizations (EADs) associated with?
|
- Conditions that result in prolonged AP (long QT)
- Pause dependent, can be triggered by abruptly ceasing rapid pacing (resulting in a pause after) |
|
|
What are delayed after-depolarizations (DADs) associated with?
|
- Excessive cytoplasmic Ca2+ and associated Ca2+ induced Ca2+ release from SR
- Tachycardia dependent can be triggered by rapid pacing |
|
|
How dose rapid pacing affect after-depolarizations?
|
- EADs are triggered by ceasing rapid pacing
- DADs are triggered by rapid pacing |

