![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
Goal of preventative medicine
|
To promote health, minimize disease, injury and sequelae
|
|
|
Describe the relevance of CPM to the clinician (4 points)
|
• What happens in the community affects the health of the patient
• Patients prefer to remain healthy/prevent disease than to get sick and be treated • HEDIS provide preventative services • Payers are experimenting w/ bonuses for keeping people healthy |
|
|
Examples of CPM in the practice of clinical medicine (5)
|
In the US, there are over 24 specialty boards and 100 subspecialties that use preventative measures -
• Internal MD/GP: Counseling obese w/ high sugar levels • Surgery: the decision to use a prophylactic Ab • OBGyn: Recommendation of Folic acid • Pediatrician: usage of vaccines for school • Ophamology: measuring introcular pressure |
|
|
Three core approaches to CPM
|
• Screening
• Counseling • Immunization |
|
|
Examples of interaction btwn PH agencies and clinicians (5)
|
• Lab testing
• PH surveillence results • Health alerts (i.e. anthrax, influenza) • Selected vaccines, anti-toxins • Prevention materials |
|
|
The responsibility clinicians have to PH agencies (3)
|
• PH surveillance reporting
• Completing death certificates • Reporting suspected child/elder abuse |
|
|
The 3 levels of prevention, their disease stage and the appropriate response
|
• Primary, pre-disease, Health promotion, specific prevention
• Secondary, latent, Screening & Tx • Tertiary, Sx disease, Tx-disability limitation-rehab |
|
|
Key word for physician-produced disease or injury
|
Iatrogenic
|
|
|
Key word for hospital-acquired infections and its #1 cause
|
Nosocomial; Hand washing is #1 cause
|
|
|
Ways to prevent surgical and medical errors
|
more training, system changes, surveillance/reporting
|
|
|
5 interventions to reduce risk of heart disease and its complications:
• (2) Primary • (2) Secondary • (1) Tertiary |
• primary - making exercise grounds/sports available, outlawing cig sales to minors
• secondary - Screening for hypertension and hypercholesterolemia, EKG for a diabetic w/ 3 risk factors • Tertiary - daily aspirin following acute MI |
|
|
4 interventions to reduce risk of diabetes and its complications:
• (1) Primary • (1) Secondary • (2) Tertiary |
5 interventions to reduce risk of diabetes and its complications:
• Primary - Counseling obese non-diabetics • Secondary - Screening using fasting plasma glucose • Tertiary - Measuring HbA1c ever 3-4 months, eye exams for retinopathy |
|
|
The goal of screening (2)
|
To ID disease or susceptibility when it is more easily/successfully treated
To minimize mortality and morbidity |
|
|
The Objective of screening
|
To classify individuals as likely/unlikely to have a disease, then refer the likely for diag testing
|
|
|
Difference between Screening and Diagnosis
|
In screening, asymptomatic people are tested to determine if further testing is needed whereas in diagnosis, those who are suspected to have the disease are tested for presence/absence of it ---> No sx group screened vs sx group being screened
|
|
|
Most important WHO requisite for a successful screening program
|
Early tx influences the course and prognosis of the disease
|
|
|
According to WHO, a screening test/exam is suitable if it follows these points (5)
|
• Relatively sensitive and specific
• Detects disease at a latent or early sx stage • Simple & inexpensive • Safe • It is acceptable to the population and providers |
|
|
Consequences of a True-positive result (5)
|
• early dx
• early or less radical tx • reduced morbidity, mortality and disability • "labeling effect" • reduced cost |
|
|
Consequence of a true-negative result
|
reassurance
|
|
|
Consequences of a false-positive (4)
|
• Unnecessary follow-up tests
• labeling, anxiety • Over-treatment of questionable abnormalities • inciting fear of future tests |
|
|
Consequences of a false negative (4)
|
• Delayed dx, leading to the disease advancing/premature diability or death
• Disregarding of early signs/sx • False reassurance • Exposure of others to infection |
|
|
Sources of screening recommendations (6)
|
Government agencies and the panels convened by them
Medical specialty associations Special interest organizations Individual experts National Guideline Clearing House |
|
|
The USPSTF base their recommendations on this
|
Evidence of the effectiveness of clinical preventative services
|
|
|
Def of passive immunity
|
A susceptible host receives protection through transfer of immunity products from another organism.
The protection os temporary and wanes with time. |
|
|
Examples of passive immunity (5)
|
• Maternal Abs
• Igs and Hyper Igs • Anti- (toxins and venoms) |
|
|
Def of Active immunity
|
In response to a foreign/non-self antigen, protection is produced by the person's own immune system.
The protection os usually long-lasting |
|
|
Criteria for a live attenuated vaccine
(4) |
• Must replicate in the host to be effective
• Produces an immune response similar to a natural infection but without causing clinical disease • Induces both humoral and cell-mediated immunity • With the exception of oral forms, it requires fewer doses |
|
|
Complications with live attenuated vaccines
|
• Fragile
• Severe rxns are possible, especially those who are immuno compromised • Can interfere with circulating Abs • Though rare, they can revert back to a being a virulent strain |
|
|
Two groups of Inactivated vaccines and the subtypes of each
|
• Whole
- viruses - bacteria • Fractional - Protein-based (toxoid and subunit) - Poly-saccharide based (pure and conjugate) |
|
|
Characteristics of Inactivated vaccines (7)
|
• Cannot replicate or revert
• Generally not as effective a live • Less interference from circulating ABs • Fewer side effects • More doses usually required (3-5) • Mostly a humoral response • Antibody titer may diminish w/ time requiring boosters |
|
|
Differences btwn WHO and US vaccine recommendations for children
|
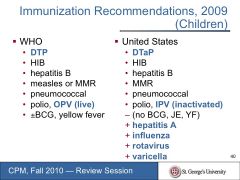
WHO includes the recommendations of DTP, OPV live polio, YF and +/-BCG
The US includes DTaP, Inactivated IPV polio, Hepatitis A, influenza, rotovirus and varicella |
|
|
Only vaccination given at birth
|
Hep B
|
|
|
The number of vaccine types recommended for children
|
9
|
|
|
The number of doses to complete the Hep B vaccine
|
3
|
|
|
The final vaccines given to children (age 4-6 yrs)
|
DTaP, IPV, MMR/VZ and Influenza (can be given much earlier)
|
|
|
Description of Part 1 (line a) of the cause of death section
|
Immediate cause of death
|
|
|
This should be listed last in Part 1 of the cause of death section
|
The underlying cause of death
|
|
|
These are never listed as an immediate cause of death
|
Mode of dying and terminal event (e.g. cardiac or respiratory arrest)
|
|
|
Define death/mortality rate and list 4 possible types
|
It is the frequency of death in a defined pop during a specified period
• Crude • Cause-specific • Age-specific • Infant mortality |
|
|
Best to worst infant mortality rates for US, UK, Grenada and Canada
|
Canada>UK>US>Grenada
|
|
|
In the equation for mortality rate:
(num/denom) x 10^n, What is the significance of 10^n? |
It represents a comparison population, usually of 1000.
|
|
|
3 actual causes of death in the US
|
Tobacco > Diet/inactivity > Alcohol
|
|
|
3 leading causes of death in US, UK and CAREC
|
HD, cancer and stroke
|
|
|
Purpose of ICD codes
|
To code for disease and causes of death worldwide
|
|
|
Physicians, Hospitals and Labs report suspected or confirmed communicable diseases here
|
Local Health Agencies
|
|
|
Physicians are also required to report these 4 situations
|
• Impaired driving
• Various types of abuse • Weapon/crime injuries • Burns > 5% of the body |
|
|
HIPAA protects the privacy of the person but specifically does not do this (3)
|
• Interfere w/ state PH reporting
• Interfere w/ investigations • Interfere w/ interventions |
|
|
The Key to analytic epidemiology and why it is needed
|
The key is a comparison group which is typically a control group; it is a population w/o the disease and needed to estimate the expected level of exposure
|
|
|
Role of the clinician in an outbreak investigation (4)
|
• see and dx patients
• report cases to the health department • provide medical records • incorporate health dept alerts/findings into their clinical practice |
|
|
Major modifiable risk factors for heart disease (7)
|
• High BP
• Abnormal blood lipids (dyslipidemia) • Tobacco use • Physical inactivity • Obesity • Unhealthy diet • Diabetes mellitus These are indirect causes on each other |
|
|
Topics to ask when taking an environmental exposure hx
|
Communit
Home Hobbies Occupation Personal habits Diet Drugs |
|
|
Common risk factors for diabetes (6)
|
• Family hx and genetics
• Ethnicity • Hx of gestational diabetes • Dyslipidemia • Over weight and Obesity • Poor diet and physical activity |
|
|
Two drugs shown to reduce the risk of diabetes
|
Metformin and Acarbose
|
|
|
In relation to diabetes prevention, medicine and lifestyle changes have shown to do this
|
increase the probability of reverting from IGT to normal glucose tolerance
|
|
|
Tertiary Prevention for screening diabetics (4)
|
Annual eye exams
Periodic foot exams HbA1c testing Psychosocial assessment |
|
|
Tertiary Prevention for vaccinating diabetics (2)
|
Influenza and Pneumococcal
|
|
|
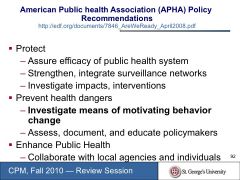
The APHA Policy recommendations for prevention (3 parts)
|
|
|
|
The two types of influenza and the type which is more virulent
|
Type A and Type B; Type A is most virulent and causes epidemics
|
|
|
Surface antigens on Type A
|
Hemagglutinin and Neuroamidase (both are glycoproteins)
|
|
|
Difference between antigen drift and shift and the type that produces new strains
|
Drift refers to minor mutations whereas shift refers to much larger immunological change, resulting in new subtypes or strains (reassortment)
|
|
|
This may cause seasonal epidemics
|
Antigenic drift
|
|
|
Components of seasonal influenza
|
Type A - H1N1, H3N2
Type B |
|
|
Difference btwn Intramscular injection and Intranasal spray influenza vaccines
|
Intramuscular - inactivated
Intranasal - Live, attenuated |
|
|
Two important facts about the 1918-1919 Pandemic
|
- Began in Spring as highly contagious, but not deadly
- Eventually had the highest death rate of those 15-35yrs of age |
|
|
The Avian Flu strain
|
H5N1
|
|
|
Criteria for an Influenza pandemic
|
• A new human influenza subtype (via antigenic shift)
• Must cause serious illness • Must spread easily from human to human |
|
|
Trend in history of the age group with the highest mortality rate for influenza
|
< 40 yrs
|

