![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
188 Cards in this Set
- Front
- Back
|
General functions of circulatory system |
1. Delivery of O2, nutrients, hormones, electrolytes, and water to cells
2. Removal of CO2 and metabolic wastes |
|
|
Common basic structure of whole circulatory system |
Concentric rings of tissue:
Tunica Intima Tunica Media Tunica Adventitia |
|
|
What is the Tunica Intima? |
Single layer of endothelial cells on a basement membrane (with a small amount of connective tissue) |
|
|
What is the Tunica Media? |
Concentric rings of smooth muscle with elongated blue nuclei |
|
|
What is the Tunica Adventitia? |
Connective tissue support/scaffolding for vessels, helping anchor them to rest of organ/tissue |
|
|
What constitutes the microcirculation? |
Arterioles, metarterioles, capillaries, post-capillary venules |
|
|
The microcirculation is the site for... |
Fluid, nutrient and waste exchange |
|
|
Capillary wall is a __________________ due to _________________, creating.... |
Semi-permeable membrane
Interendothelial pores
Osmotic pressure through plasma proteins |
|
|
What is the interstitium? |
Space between the cells and the microcirculation containing ECM |
|
|
ECM (extracellular matrix) is made up of? |
Collagen fibres embedded within a protein polysaccharide gel |
|
|
Interchange of water between the vascular and interstitial compartments is tightly regulated by? |
The Starling Equilibrium |
|
|
Starling equilibrium is achieved when there is a balance between? |
Net filtration and Net absorption |
|
|
2 types of Starling forces |
Hydrostatic pressure (forces fluid out)
Colloid Osmotic pressure (draws fluid in) |
|
|
Net filtration pressure equation |
(Plasma hydrostatic [arteriolar] + Tissue oncotic) - (Plasma oncotic + Tissue hydrostatic) |
|
|
Net absorption pressure equation |
(Plasma hydrostatic [venular] + Tissue oncotic) - (Plasma oncotic + Tissue hydrostatic) |
|
|
What happens when fluid balance is disturbed? |
EDEMA |
|
|
Define edema |
Accumulation of excess fluid in interstitial tissue spaces or body cavities |
|
|
Dependent edema |
Edema of ventral areas (limbs, under jaw) due to gravity |
|
|
Severe, generalized subcutaneous edema in a still born puppy due to congenital heart defect, is called? |
Anasarca |
|
|
Term for edema fluid accumulation in body cavities? |
Effusion
-Hydrothorax -Ascites (hydroperitoneum) -Hydopericardium |
|
|
4 Mechanisms of Edema |
1. Increased intravascular hydrostatic pressure 2. Decreased plasma oncotic pressure 3. Lymphatic obstruction 4. Increased vascular permeability |
|
|
Increased Intravascular Hydrostatic Pressure -Localized caused by? -Generalized caused by? |
Localized - Occlusions or obstructions to venous outflow (tumor, abscess, thrombus, intestinal accidents)
Generalized - Heart failure resulting in venous pressure
|
|
|
Left vs Right sided heart failure sequella? |
Left - Backflow into the lungs leading to pulmonary edema
Right - Backflow on the systemic and portal venous systems leading to bottle jaw/ventral subcutaneous edema |
|
|
Explain why decreased plasma oncotic pressure leads to edema? |
-Albumin exerts major portion of plasma oncotic pressure, therefore hypoalbuminemia decreases this pressure and fluid leaks out -Hypoalbuminemia results from reduced production or excessive loss |
|
|
Lymphatic obstruction aka ________________ is always ___________ -Caused by? |
Lymphedema
Localized
-Damage or obstruction by trauma, surgery, inflammation or neoplasia |
|
|
Clear to slightly yellow fluid with low protein and low cells is called ________________
Inflammatory edema fluid with high protein and high cells is called _______________ |
Transudate
Exudate |
|
|
How is Increased Vascular Permeability different from the other mechanisms? What is it caused by? |
It's an exudate rather than a transudate
Opening of interendothelial gaps due to (examples: inflammation, vasculitis, infections, toxins, insect bites) |
|
|
1. Enlarged mammary glands most common in ______________ cows 2. Evaluation of enlarged mammary glands should include __________ & ___________ histories 3. Most common causes of udder swelling are ___________________, ____________ & __________ 4. Congenital anomalies (such as....) won't show up until ____________ |
1. Periparturient
2. Medical & Reproductive histories
3. Onset of lactation, udder edema, and mastitis
4. (stenotic or absent teat canals) parturition/lactation |
|
|
What is the milk producing unit in the udder? |
Alveolus |
|
|
External pudendal vein returns to heart through the?
Superficial epigastric vein (milk) vein returns to heart through the? |
Caudal vena cava
Cranial vena cava |
|
|
Non-infectious cause of udder swelling:
Onset of Lactation (pathway) |
-Development of milk secretion tissue in the udder -Edema associated with the transition to lactation -Engorgement of tissues |
|
|
Mammogenesis during the DRY PERIOD? (Drying off process - what happens?)
Name Steps |
1. Milking is stopped 2. Intramammary luminal pressure in udder increases and becomes greater than the blood pressure 3. Milk biosynthesis ceases 4. Alveoli furthest from gland cistern degenerate first 5. Involution progresses to the alveoli closer to the gland cistern 6. Adipose cells occupy the empty intra-luminal space 7. With complete involution only the duct system remains |
|
|
Mammogenesis during LATE PREGNANCY |
-Estrogen alone stimulates mammary duct growth -Progesterone alone stimulates formation of alveoli -Synergistically, progesterone and estrogen induce lobule-alveolar development |
|
|
Non-infectious causes of udder swelling:
Udder Edema |
Dietary Congestive heart failure Poor conformation Reduced plasma proteins Lymphatic obstruction |
|
|
Most common cause of non-inflammatory mammary gland swelling |
Udder Edema |
|
|
Most common cause of INFECTIOUS mammary gland swelling? |
Mastitis |
|
|
Categories of mastitis |
Contagious
Environmental |
|
|
Contagious mastitis caused by? Source of infection? |
Cause: Gram +ve bacteria (Strep. agalactiae and Staph. aureus and Mycoplasma)
Source of infection: Udder |
|
|
Environmental mastitis results in the ?? Caused by?? Source of infection?? |
Most severe inflammatory reaction and swelling in the udder
Caused by: Gram -ve bacteria (E.coli & Klebsiella)
Source of Infection: Environment |
|
|
Where is the first detectable sign of udder swelling when caused by inflammation? |
Gland secretions with an elevated somatic cell count (number of WBCs) |
|
|
(Steps) Pathway of environmental mastitis infection? |
1. Coliform bacteria pass through streak canal and invade mammary gland 2. Bacteria rapidly proliferate & reach peak in 5-16 hours 3. Phagocytosis & killing of coliforms by neutrophils/macrophages releases LPS endotoxin from bacterial cell walls 4. Secondary endogenous release of inflammatory mediators such as prostaglandins & leukotrienes, and interleukins from macrophages are responsible for symptoms of acute coliform mastitis |
|
|
Staph. aureus mastitis details |
-Spreads rapidly from cow to cow -Primary source: infected udder -Transfer thru milking practices -Chronic subclinical mastitis -75-80% of dairies have some infection -Poor response to treatment -Damage to alveoli (can be gangrenous) |
|
|
Some teat malformations? |
-Web Teat -Blind Teat |
|
|
How can we evaluate teat obstructions? |
-Ultrasound -Theloscopy |
|
|
All causes of udder swellings?? |
-Onset of lactation -Udder edema -Mastitis -Injury -Obstruction of milk collection system -Tumors |
|
|
Define micturition |
Normal process of passive storage and active voiding or urine |
|
|
Disorders of micturition |
Incontinence - problem with urine storage
Urine Retention - problems with bladder emptying |
|
|
Define stranguria |
Straining to urinate |
|
|
Define pollakiuria |
Producing small amounts of urine, frequently |
|
|
Define dysuria |
Difficulty urinating |
|
|
Define polyuria |
Producing lots of urine |
|
|
Define anuria |
No urine production |
|
|
Define oliguria |
Small amounts of urine production |
|
|
3 layers of bladder wall? |
1. Mucosa with distensible Transitional Epithelium and lamina propria 2. Thick smooth muscle (Detrusor Muscle) 3. Fibrous adventitia |
|
|
Transitional epithelium is also called |
Urothelium |
|
|
Bladder Innervation: Para-sympathetic
1. Source 2. Neurotransmitter 3. Activity patterns 4. Effects/Receptor |
1. Pelvic nerve 2. ACh, ATP, NO 3. Inputs from PMC during voiding phase; typically inhibited during storage phase 4. Detrusor contraction (M3); Presynaptic inhibition of NE (M2); Relaxation of bladder neck (NO)
*PMC: Pontine Micturition Center |
|
|
Bladder Innervation: Sympathetic
1. Source 2. Neurotransmitter 3. Activity patterns 4. Effects/Receptor |
1. Hypogastric nerve 2. Norepinephrine, Neuropeptide Y 3. Activated by inputs from urethra during storage phase; inhibited during voiding phase 4. Detrusor relaxation (B3); Contraction of bladder neck (a1); Presynaptic inhibition at parasympathetic ganglia (a2) |
|
|
Bladder Innervation: Somatic (skeleto-motor)
1. Source 2. Neurotransmitter 3. Activity patterns 4. Effects/Receptor |
1. Pudendal nerve 2. ACh 3. Activated by inputs from urethra, pons & cerebral cortex; inhibited via interneurons by inputs from PMC during voiding phase 4. Tonic contraction of external urethral sphincter (nicotinic) |
|
|
Bladder Innervation: A(delta) - afferent
1. Source 2. Neurotransmitter 3. Activity patterns 4. Effects/Receptor |
1. DRG 2. L-glutamate 3. Activated during normal bladder distension & contraction 4. Signal physiologic bladder fullness; trigger the normal micturition reflex |
|
|
Bladder Innervation: C-type-afferent
1. Source 2. Neurotransmitter 3. Activity patterns 4. Effects/Receptor |
1. DRG 2. L-glutamate, substance P, CGRP, ATP, NO 3. High threshold of activation; silent C-afferents activated by inflammation 4. Spinal micturition reflex in spinal cord injury; release of mediators from urothelium |
|
|
Unique features of Micturition |
-Highly dependent on CNS -Depends on voluntary control & learned behaviour -2 modes of operation (on/off switch) |
|
|
What happens during Storage reflex |
Relaxation of bladder Contraction of internal and external urethral sphincters |
|
|
What happens during Voiding reflex |
Contraction of bladder Relaxation of urethral sphincters |
|
|
2 major categories of micturition disorders |
1. Disorders associated with a large or distended urinary bladder (urine retention) 2. Disorders associated with a small or normal-sized urinary bladder (incontinence) |
|
|
Urine retention is usually secondary to... |
-Decreased detrusor contractility -Increased urethral outflow resistance |
|
|
Urinary incontinence is usually secondary to... |
-Decreased urethral outflow resistance -Increased detrusor muscle contractility (nerve damage) -Inability of bladder to expand in capacity -Bladder spasms |
|
|
Neurogenic causes of urine retention with a distended bladder |
-LMN disease (detrusor & sphincter areflexia) -UMN disease (detrusor areflexia & sphincter hypertonus) -Detrusor-urethral dyssynergia (functional urethral obstruction) |
|
|
LMN disease results in
(distended bladder disorder) |
Large, flaccid distended bladder; easily expressed |
|
|
UMN disease results in
(distended bladder disorder) |
Large, firm distended bladder: difficult to express |
|
|
Non-neurogenic causes of urine retention with a distended bladder |
Physical outflow tract obstruction |
|
|
Causes for physical outflow obstruction (urinary) |
Physical entity blocking outflow Neoplasia, calculi (dogs) Mucus plugs, calculi (cats) Calculi (horses & bulls) *Large distended bladder that is difficult to express and catheterize |
|
|
Clinical signs of physical outflow obstruction? |
-Stranguria (no actual urine production) -Urine dribbling -Restlessness/vocalization -Abdominal pain |
|
|
Urinary incontinence disorders with a small to normal urinary bladder |
Increased detrusor contractility -Bladder/urethral irritation & inflammation -UTI, FLUTD (feline lower urinary tract disease) -Pollakiuria, Dysuria, Stranguria, Hematuria
Decreased outflow resistance -aka: USMI - Urethral Sphincter Mechanism Incompetence -Seen in spayed, medium to large breed dogs -Decreased estrogen levels lead to decreased urethral muscle tone & urine leakage/incontinence |
|
|
Congenital causes for decreased urethral outflow resistance |
-Ectopic ureters -Patent urachus
*Seen an constant urine dribbling |
|
|
Diestrus
1. Structures on ovaries 2. Dominating hormone 3. Cervix |
1. Corpus luteum 2. Progesterone 3. Closed |
|
|
Estrus
1. Structures on ovaries 2. Dominating hormone 3. Cervix |
1. Follicles (and a corpus albicans) 2. Estrogen 3. Open |
|
|
Describe the mare's general estrous cycle |
Seasonally Polyestrous Long day breeders 21-22 days Diestrus is 14 days Estrous period shorter during peak of season |
|
|
Seasonality is influenced by |
Melatonin levels (pineal gland/darkness)
Nutrition, Temperature, Opioids |
|
|
Fall transition for mare's seasonality - what happens? |
-FSH and LH levels start to decline -LH declines first -Follicular growth without ovulation -Mares have an autumn follicle |
|
|
What is an autumn follicle? |
-Follicle with large diameter -Follicle persists -No concurrent uterine edema or signs of estrus *Can not be manipulated |
|
|
Methods to manipulate seasonality? |
-GnRH -recombinant FSH |
|
|
General canine estrous cycle |
-Monestrous, non-seasonal -2 estrous periods a year -Dormitory effect |
|
|
Canine Estrous Cycle:
Length of... -Diestrus -Anestrus -Proestrus -Estrus |
Diestrus - 2 months Anestrus - 4 months Proestrus - 9 days (0-27dys) Estrus - 9 days (4-24dys) |
|
|
Signs of anestrus in a bitch |
-Not receptive to mating -Small vulva -Deep anestrus (FSH and LH low) -Parabasal cells with occasional small intermediate cells |
|
|
Signs of proestrus in a bitch |
-Male interested in female, but female is NOT interested in male -Follicles grow due to increase in estrogen -Vaginal mucosa is smooth (edematous) and vulva swells -Testosterone peaks at end of proestrus -Progesterone low until late proestrus |
|
|
Signs of estrus in a bitch |
-Female is receptive to mating -Estrogen peaked in proestrus, levels decline in estrus -Progesterone increases -LH surge and ovulation occurs |
|
|
Vaginal cytology during estrus in a bitch |
-Increase in cornified cells -RBCs decrease -Ovulate primary oocyte |
|
|
Signs of disestrus in a bitch |
-Female is not receptive to mating; no longer attracts males -Estrogen is low -Progesterone increases rapidly to peak 3-4 weeks after diestrus onset |
|
|
Vaginal cytology for first day of diestrus in a bitch |
Abrupt decline in cornified cells >50% intermediate cells WBCs present Metestrum cells |
|
|
Define feedlot |
An area or building where cattle (or other livestock) are fattened rapidly for market |
|
|
Factors that may influence feedlot profitability |
-Economic factors (purchase, sale, feed, interest) -Management factors (ADG, FE, carcass quality) |
|
|
Role as veterinary consultant at a feedlot |
Optimize production & Maximize profits by developing, implementing and evaluating herd health management programs adapted to each individual feedlot
|
|
|
What does a good herd health management program do? |
-Provides for healthier, better performing cattle -Avoid unnecessary use of vaccines, anthelmintic and antibiotics -Helps insure you are producing a safe, wholesome product |
|
|
Heard health management programs include |
-Preventative medicine programs (vaccination, on-arrival antibiotics, metaphylaxis)
-Therapeutic management programs (treatment protocols for disease syndromes) |
|
|
Implementation of herd health programs includes |
-Training and education of feedlot employees -Ongoing disease diagnostics (necropsies) -Record keeping system (computer software) |
|
|
Evaluation/Revision of herd health programs includes |
Data analysis on: -Morbidity/mortality -Treatment response -Performance |
|
|
Given a feedlot problem case, what are the steps required to respond to case? |
1. Data analysis -calculate feedlot performance
2. Investigate cause -differential diagnosis, additional tests, final diagnosis |
|
|
Feed efficiency calculation |
Units of feed DM consumed / Units of animal weight gain
OR
Units of animal weight gain / Units of feed DM consumed |
|
|
Define Residual Feed Intake (RFI) |
Difference between actual feed intake and the feed an animal is expected to consume based on its body weight and ADG
|
|
|
What does a negative RFI mean? |
Higher efficiency as cattle are consuming less than expected |
|
|
List some factors that impact DMI |
-Animal factors (genetics, BW, body fat, gender, age, breed) -Feeding management (energy density of diet, feedbunk management) -Implants & feed additives (ionophores) -Environmental factors (ambient temperature, mud) -Health status of animal |
|
|
2 types of feedbunk management |
1. Slick bunk management
2. Ad-libitum management |
|
|
Slick bunk management: goal and risk |
Goal: to have a clean bunk in slightly less than a 24 hour period
Risk: Reduction in intake if too much restriction; potential for grain overload
*More widely adopted |
|
|
Ad-libitum management: goal and risk |
Goal: To always have feed in the bunk
Risk: wasted-feed, increased labour, potential for digestive disorders |
|
|
How do ionophores impact ADG and F:G |
Act in rumen to increase energy availability by changing the proportion of VFAs *More propionic acid, less acetic and butyric acid |
|
|
How does monensin work? |
Works on gram +ve bacteria and causes loss of K+ out of the cell, with Na+ and H+ moving into the cell. Energy is required to export H+ out of cell and thus the bacterial cells expend so much energy doing this, that they die due to less energy availability for growth & metabolism. |
|
|
What do B-agonists do? |
Repartitioning agent that basically changes fat deposition to protein/muscle deposition |
|
|
Which implant strategy is best when optimum efficiency is the only goal, regardless of carcass quality? |
High-dosage implants with re-implantation frequently |
|
|
3 ways to alter growth? |
1. Genetics 2. Nutrition 3. Growth Promoting Agents |
|
|
Type of muscle/fat growth: 1. Embryonic stage 2. Fetal stage 3. End of fetal stage (7-9.5 months)
Bonus: when are total # of muscle fibres fixed? |
1. Primary (type 1) myogenesis
2. Secondary (type 2) myogensis)
3. Adipogenesis & Muscle fibre hypertrophy
*6 months |
|
|
How does growth of skeletal muscle occur post-natally? |
Satellite cells below sarcolemma are stimulated, start dividing and fuse with skeletal muscle and incorporate their nuclei into nuclei of skeletal muscle cells |
|
|
Beef: British breeds vs Continental breeds |
Continental: Charolais, Limousin, Simmental -Large frame -Late fattening (internal fat > subcutaneous) -Higher DMI, BW and ADG British: Angus, Hereford, Shorthorn -Small frame -Early fattening (^ fat on high energy diets) -Fat (internal fat < subcutaneous fat) |
|
|
Types of implants for beef |
1. Estrogens 2. Androgens 3. Combination |
|
|
Mechanisms of Endocrine Disease
|
Insufficient (hypo function)
Excessive hormone production (hyper function) |
|
|
Mechanisms of Endocrine Disease: Hypofunction types
|
Primary
Secondary |
|
|
Primary Hypofunction causes
|
-Biochemical defect in synthetic pathway (uncommon!)
-Failed to develop -Destruction (immune-mediated OR neoplasia) |
|
|
Secondary Hypofunction causes
|
-Destructive lesion in one organ leads to hypo function of another
-Failure of trophic hormone production -Usually pituitary lesion (nonfunctional tumour) *RARE |
|
|
Mechanism of Endocrine Disease: Hyperfunction types
|
Primary
Secondary |
|
|
Primary Hyperfunction causes
|
-Neoplasm of endocrine gland (common)
-Autonomously secrete a hormone in excess of body's ability to use/degrade |
|
|
Secondary Hyperfunction causes
|
-Lesion in one organ results in stimulation and hyper secretion of hormone in target organ
-Excess production of trophic hormone -Pituitary neoplasm (functional) |
|
|
Adrenal gland medulla secretes?
|
Catecholamines
-Epinephrine -Norepinephrine |
|
|
Outer to inner zone of adrenal gland cortex
|
Zona glomerulosa
Zona fasiculata Zona reticularis |
|
|
Zona glomerulosa secretes
|
Mineralcorticoids (aldosterone!!)
|
|
|
What controls the zona glomerulosa?
|
RAAS (renin angiotensin aldosterone system)
|
|
|
Functions of Aldosterone
|
Acts on distal convoluted tubules
-Excretion of potassium -Retention of sodium *Decreases blood pressure |
|
|
Zona fasiculata
-What does it secrete? -Release regulated by? |
Glucocorticoids (cortisol)
ACTH |
|
|
What does cortisol do?
|
-Spares glucose (gluconeogenesis, lipolysis, protein catabolism)
-Suppress inflammation/immunity -Negative effect on wound healing (reduces fibroplasia) |
|
|
Zona reticularis
-What does it secrete? -Secretion regulated by? |
Sex hormones (progesterone, estrogen, androgens)
Regulated by ACTH |
|
|
Types of Canine Hyperadrenocorticism (and what causes them)
|
Pituitary Dependant (85% of cases)
-Excess ACTH secretion -Pars distalis adenoma Adrenal Dependent (15% of cases) -Excess cortisol secretion -50:50 benign vs malignant Iatrogenic |
|
|
Is hyperadrenocorticism common in cats?
|
NO
|
|
|
Most common clinical manifestations of canine hyperadrenocorticism (or Cushing's disease)
|
PU/PD
Alopecia Pendulous abdomen Hepatomegaly Polyphagia Panting Muscle weakness *NOTE: complaints of illness are ABSENT!! |
|
|
Adrenal hypo function: when do we see clinical signs?
|
When 85-90% of adrenal tissue is lost
|
|
|
Hypoadrenocorticism most commonly results in?
|
Cortisol & Aldosterone deficiency
|
|
|
Suspected cause of hypoadrenocorticism
|
Immune mediated mechanism
|
|
|
Functions of cortisol
|
Stress hormone
Glucose metabolism (hepatic gluconeogenesis, glycogenesis) Vascular tone |
|
|
Absence of cortisol results in?
|
Anorexia, lethargy, GI signs, possibly hypoglycemia
|
|
|
Aldosterone is the principal cell of??
-Functions of aldosterone |
*Principal cell of distal tubule & collecting duct
-Tubular reabsorption of sodium -Promotion of potassium secretion |
|
|
Absence of aldosterone results in?
|
Hyperkalemia
Hyponatremia |
|
|
Clinical signs of 'acute crisis' adrenohypocorticism
|
Weak pulses, bradycardia, prolonged CRT, mental depression, maybe GI signs
|
|
|
Clinical signs of 'chronic' hypoadrenocorticism
|
Ain't doing right*, weight loss, intermittent or chronic GI signs, intermittent or chronic lethargy
|
|
|
Diagnostic tests for hypoadrenocorticism
|
Serum Biochemistry (electrolytes)
-check for hyponatremia, hyperkalemia -hypoglycemic Complete Blood Count -absence of stress leukogram in clinical ill patient -cortisol (important role in movement of WBCs) |
|
|
Definitive diagnosis for hypoadrenocorticism
(include steps for test) |
ACTH Stimulation Test
1) Assess basal cortisol concentrations 2) Administer synthetic ACTH 3) Measure cortisol post-stimulation |
|
|
ACTH Stimulation Test results and what they mean
|
Resting: <27 nmol/L
Post stimulation: <27 nmol/L *NO CHANGE *Addison's Disease |
|
|
Hyperadrenocorticism aka
|
Cushing's Disease
|
|
|
Hypoadrenocorticism aka
|
Addison's Disease
|
|
|
Hypothalamic-Pituitary-Thyroid Axis:
What does the hypothalamus secrete? Negative feedback on hypothalamus by? |
TRH - Thyrotropin Releasing Hormone
fT4 & fT3 negative feedback on hypothalamus |
|
|
Hypothalamic-Pituitary-Thyroid Axis:
What does the anterior pituitary secrete? Negative feedback on anterior pituitary by? |
TSH - Thyroid Stimulating Hormone
fT4 & fT3 negative feedback on anterior pituitary |
|
|
Hypothalamic-Pituitary-Thyroid Axis:
What does the thyroid gland secrete? What happens to secretions? |
Thyroglobulin --> monoiodotyrosine (MIT) & diiodotyrosine (DIT) --> T3 (triiodothyronine) & T4 (thyroxine)
T4 is converted to T3 in peripheral tissues T3 is more potent than T4 |
|
|
Functions of Thyroid Hormone
|
-Increased metabolic rate
-Increased number & affinity to beta adrenergic receptors -Catabolism of muscle and fat -Stimulates normal growth -Influences normal respiratory centre responses -Stimulates normal bone turnover -Lipid metabolism (synthesis, mobilization, degradation) |
|
|
Common disorders of thyroid gland:
1) Canine 2) Feline |
1) Hypothyroidism
2)Hyperthyroidism |
|
|
Causes of thyroid follicular dysfunction
- Hypofunction/Hypothyroidism |
Primary
-Immune mediated, non-functional neoplasm -Destruction of gland/failure to develop Secondary (RARE) -Failure of TSH -Pituitary lesions Tertiary (RARE/NON-EXISTENT) -Destructive hypothalamus lesion |
|
|
Causes of thyroid follicular dysfunction
-Hyperfunction/Hyperthyroidism |
Primary
-Neoplasm/hyperplasia of thyroid follicular epithelium -Autonomously secretes hormone in excess to body's ability to use/degrade |
|
|
Canine Hypothyroidism
-Causes |
**PRIMARY**
Lymphocytic thyroiditis (50%) -progressive destruction (slow) Idiopathic atrophy (45%) -functional tissue replaced by adipose/fibrous tissue |
|
|
Common clinical manifestations of canine hypothyroidism
|
Obesity (due to decreased metabolic rate)
Dermatological signs Lethargy, mental dullness |
|
|
Why do we get dermatological signs in canine hypothyroidism?
|
Hair is in resting phase (telogen) due to lack of thyroid hormone
[Thyroid hormone stimulates growth phase of hair cycle (anagen)] |
|
|
Diagnostics for canine hypothyroidism
|
Total T4 (below reference interval; don't use on its own)
Run concurrent TSH (this will be increased) |
|
|
Most common endocrinopathy in cats?
|
Feline hyperthyroidism
|
|
|
Aetiologies of feline hyperthyroidism?
|
Adenoma (90-95%)
-70% bilateral, 30% unilateral Adenocarcinoma (2-5%) Functional ectopic tissue (rare) |
|
|
Clinical manifestations of feline hyperthyroidism
|
Weight loss
Palpable thyroid Polyphagia Hyperactivity Tachycardia PU/PD Vomiting Cardiac murmur Diarrhea |
|
|
Why do we see PU/PD in feline hyperthyroidism?
|
Increased renal blood flow
Thyroid has direct effect on thirst centre |
|
|
Why do we see tachycardia in feline hyperthyroidism?
|
Increased adrenergic receptors and sensitivity in heart
|
|
|
Diagnosis of feline hyperthyroidism
|
Consistent clinical signs
Thyroid hormone analysis (elevated!) |
|
|
Low dose dexamethasone suppression test:
-What does it screen for? -Theory of results? |
Presence of hyperadrenocorticism
Normally, glucocorticoids have negative feedback to pituitary-adrenal axis and ACTH release. Exogenous steroids will thus reduce cortisol levels in a normal patient. If cortisol not suppressed in 8 hours, then animal has hyperadrenocorticism |
|
|
What is a Stress Leukogram
|
Test that looks at cortisol by examining WBCs in circulation:
-Lymphopenia (decreased lymphocytes) -Neutrophilia (increased neutrophils) -Monocytosis (increased monocytes) |
|
|
Why do we have hyperkalemia and hyponatremia in Addison's disease?
|
Lack of aldosterone, which is important for Na reabsorption and Na/K ATPase function
Tubular lumen does not maintain negativity and thus, K is not excreted as much |
|
|
Diseases with weight loss AND polyphagia
|
1. Hyperthyroidism2. Exocrine Pancreatic Insufficiency (EPI)3. Diabetes
|
|
|
What is the cornea and what does it do?
|
Avascular, transparent layer that is found in anterior fifth of fibrous tunic
-Supports intraocular contents, refraction of light and transmission of light |
|
|
What is the sclera?
|
Opaque, vascular remainder of the fibrous tunic
|
|
|
Iris is composed of? What does it do?
|
Dilator muscle - radial smooth muscle (sympathetic)
Sphincter muscle - ring of smooth muscle at pupillary margin (parasympathetic) Affects pupil size, shape and reaction to light |
|
|
Term for pupils that are of unequal size or asymmetric??
More specific: Dilated? Constricted? Most common cause? other cause? |
Anisocoria
Mydrasis (dilated) Miosis (constricted) Ocular cause most common, also neurologic |
|
|
What is the lens and what does it do?
|
It is a refractive structure, suspended in the globe by zonular ligaments
Focuses images on the retina |
|
|
Which structure refracts light more: the cornea or the lens?
|
CORNEA!
|
|
|
What is a cataract?
|
Opacity to the lens
|
|
|
What is the vitreous of the eye? What does it do?
|
Largest structure in the eye that is transparent and made up of jelly-like material
Transmits light, maintains normal shape of the eye and supports the retina |
|
|
What is the choroid of the eye? What does it do?
|
Layer of vasculature under the retina
Main source of nutrition for the retina |
|
|
Tapedum lucidum is part of? What is it?
|
Choroid
Reflective layer that restimulates photoreceptors |
|
|
2 important layers of the retina?
|
Retinal pigmented epithelium
Neurosensory retina (all the other 9 layers) |
|
|
What does the retina do?
|
Phototransduction
Process by which the light is converted into a neuronal signal via rods and cones |
|
|
Types of Retinal Vascular Patterns
(where are blood vessels located in eye) |
Holangiotic - whole eye (ruminants, pigs, carnivores)
Paurangiotic - minute vessels around optic nerve head (horses, guinea pigs) Merangiotic - vessels eminate as broad horizontal bands from optic nerve head (rabbits) Anangiotic - avascular (birds, do have vascularized pecten though) |
|
|
What is the fundus? How can we examine it?
|
Internal structures of the eye including the retina, optic disc and choroid
Opthalmoscopy! |
|
|
Proportion of ipsilateral nerve fibres in:
1. Horses 2. Dogs 3. Cats |
1. 15% ipsilateral
2. 25% ipsilateral 3. 33% ipsilateral |
|
|
Visual pathway:
Why is partial crossover important? |
Allows for both hemispheres to continue receiving input if there is 100% destruction of one retina/optic nerve
|
|
|
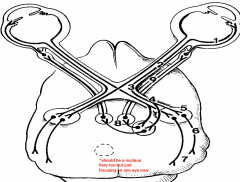
1. Retina
2. Optic Nerve 3. Optic Chiasm 4. Optic Tract 5. Lateral Geniculate Nucleus (LGN) 6. Optic Radiations 7. Occipital Cortex 8. Pretectal & Oculomotor Nerve Nuclei 9. Oculomotor Nerve |
|
|
Visual Pathway
|
Axons of ganglion cells converge at optic disc to form optic nerve - retinotopic arrangement of axons - optic nerve exits orbit - optic chiasm - optic tracts - 20% to brainstem nuclei, 80% go to LGN and then visual cortex in occipital lobe
|
|
|
The dazzle reflex is a _____________ reflex and requires?
|
Subcortical
Intact retina, optic nerve, optic tract and midbrain (does NOT require occipital cortex) |
|
|
Menace response is?
What does it involve? What does it require? |
NOT A REFLEX
Involves cerebral cortical integration & interpretation Requires intact retina, visual pathways, visual cortex and CN VII |
|
|
What is an electroretinogram?
What does it not assess? |
Test to assess retinal activity (specifically outer retina)
Doesn't assess ganglion cells or optic nerve |
|
|
Terms for
1. Right eye 2. Left eye 3. Both eyes |
1. OD - Oculus dexter2. OS - Oculus sinister3. OU - Oculus uterque
|

