![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
True or False:
The incidence of mortality due to COPD declined between the years of 1970 and 2002, but at a slower rate than other chronic diseases. |
FALSE
COPD has had a 120% increase in mortality rate between 1970 and 2002 |
|
|
Gold defination of COPD
|
COPD is a preventable and treatable disease state with some significant extrapulmonary effects that may contribute to the severity in individual patients. Its pulmonary component is characterized by airflow limitation that is not fully reversible. The airflow limitation is usually progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases.
|
|
|
What is the etiology of COPD?
|
1. Smoking - accounts for 80-90% of cases
2. Environmental exposures * occupational dusts * indoor and outdoor polution * environmental (2nd hand) tobacco smoke 3. Genetic predisposition * 1-3% of all COPD cases are due to inherited Alpha-1 Antitrypsin (antiprotease)Deficiency * results in COPD at a younger age than expected (<45) or COPD in a non-smoker |
|
|
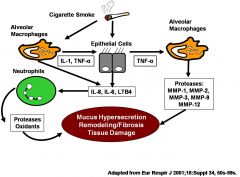
How does smoking cause inflammation and damage that lead to COPD?
|
|
|
|
Describe the pathogenesis of COPD.
|
1. Inflammation:
* mediators - LTB4, IL-8, TNF-alpha - neutrophils, macrophages, CD8* cells Leads to Protease Imbalance and Oxidative stress 2. Protease Imbalance * increased MMP's (matrix matalloproteinases) * increased cathepsins * increased proteinase-3 * increased neutrophil elastase 3. Oxidative stress: * nitric oxide * hydrogen peroxide 4. Inflammation, Protease imbalance and oxidative stress all lead to: * mucus gland hyperplasia - causes mucus hypersecretion * Airway narrowing/Fibrosis * Alveolar wall destruction |
|
|
How do proteases cause damage to the lungs?
|
* Proteases break down collagen which is a major component of lung tissue
* Proteases break down elastin which is responsible for aveolar recoil (without elastin the alveolar become floppy) |
|
|
What pathological changes in the proximal airways can result from COPD?
|
* inflammatory cell infiltration of the epithelium
* increased number and size of the epithelial goblet cells and mucus secreting glands leads to increased mucus secretion * impaired ciliary motility |
|
|
What pathological changes in the peripheral airways can result from COPD?
|
* chronic inflammation leads to
* airway remodeling leads to * scar tissue formation leads to * fibrosis leads to * diffuse airway narrowing/fixed airway obstruction (very difficult to open) |
|
|
What pathological changes in the lung parenchyma can result from COPD?
|
* Centrilobular emphysema
- most common form of emphysema - dilatation and destruction of the respiratory bronchioles * Panlobular emphysema - AAT deficiency - More severe - dilatation and destruction of respiratory bronchioles and alveolar ducts and sacs |
|
|
What pathological changes in the pulmonary vasculature can result from COPD?
|
* thickening of the pulmonary vessels
* endothelial cell dysfunction * infiltration of vessel wall by inflammatory cells - hypertrophy of the smooth muscle * leads to pulmonary HTN - high pressure in the lungs |
|
|
What pathological changes in the mucus and ciliary funtion can result from COPD?
|
Mucus hypersecretion and ciliary dysfunction:
* usually the first physiological abnormalities * results in an increased cough & sputum production |
|
|
What pathological changes in the expiratory airflow can result from COPD?
|
* Irreversible: remodeling leads to fibrosis & narrowing of airways, parenchymal destruction (loss of alveolar attachments and lung elastic recoil)
* Reversible: inflammatory cell infiltration & mucus accumulation |
|
|
What pathological changes in the pulmonary inflation can result from COPD?
|
Pulmonary hyperinflation (“barrel chest”)
* impaired elastic recoil leads to impaired emptying leads to air trapping leads to increased lung volumes |
|
|
What pathological changes in the gas exchange can result from COPD?
|
Gas exchange abnormalities
* peripheral airways obstruction, parenchymal damage & pulmonary vascular abnormalities lead to reduced gas exchange leads to hypoxia & hypercapnia * chronic hypoxemia leads to constriction of small pulmonary arteries leads to pulmonary hypertension leads to corpulmonale (right-sided heart failure) |
|
|
Systemic Features
|
Cachexia
Skeletal muscle wasting Osteoporosis Depression Anemia Increase in CAD |
|
|
How are COPD and Asthma differentiated?
|
ONSET
* Asthma = Anytime, often childhood or early adulthood * COPD = Later in life, midlife or beyond Usual Etiology * Asthma = Immunologic stimuli, family history, allergies * COPD = Cigarette smoking (usually >20packyears) or exposure to other risk factors COURSE * Asthma = Usually intermittent * COPD = Chronic, progressive Airflow Limitation * Asthma = Largely reversible * COPD = Largely irreversible Clinical features * Asthma = Episodic wheeze, chest tightness, cough, dyspnea * COPD = Chronic dyspnea, cough, sputum, wheeze Inflammatory cells * Asthma = Eosinophils, mast cells, CD4+ cells * COPD = Neutrophils, macrophages, CD8+ cells Response to steroids *Asthma = inhibits inflammation * COPD = Little to no effect on inflammation |
|
|
What are classic symptoms of COPD?
|
Chronic cough = first symptom
chronic sputum production dyspnea leads to progressive, persistent and usually worse on exertion |
|
|
List risk factors for COPD
|
Smoking history (usually >20 packyears
occupational dusts and chemicals family history of Alpha-1 Antitrypsin deficiency |
|
|
What parameters are evaluated with spirometry?
|
FVC (force vital capacity)
FEV1 (force expired volume in 1 sec) |
|
|
How are FVC and FEV1 used for COPD diagnosis and staging?
|
Fev1/FVC ratio (post bronchodilator) <0.7 indicates the presence of obstruction that is not fully reversible
% predicted FEV1 (post bronchdilator - comparison of patient's FEV1 after bronchodilation to what would be expected based on height, age, sex, and race. This indicates the severity of obstruction |
|
|
What additional data is available with Full Pulmonary Function Testing?
|
Total lung capacity
Residual volume Diffusion capacity (DLCO) *gas-transfer function of the lungs * carbon monoxide used as a surrogate for oxygen * reduced value consistent with emphysematous changes |
|
|
What is the GOLD staging of COPD?
|
Stage 1 (mild)
* FEV1/FVC <0.7 * FEV1 % predicted > or = 80% * Lung function is abnormal but patient may or may not have symptoms Stage 2 (moderate) * FEV1/FVC <0.7 * FEV1 % predicted 50-79% * Worsening lung function; start experiencing symptoms Stage 3 (Severe) * FEV1/FVC <0.7 * FEV1 % predicted 30-49% * Worsening symptoms; repeated disease exacerbations Stage 4 (very Severe) * FEV1/FVC <0.7 * FEV1 % predicted < 30% or * < 50% + evidence of chronic or respiratory failure |
|
|
Goals of COPD Management
|
|
|
|
How is Stage 1 COPD managed?
|
1. Smoking Cessation & vaccinations (influenza and pneumococcal)
2. Short-acting beta-agonist as needed for acute relief of symptoms (dyspnea and wheezing) |
|
|
How is Stage 2 COPD managed?
|
1. Smoking Cessation & vaccinations (influenza and pneumococcal)
2. Short-acting beta-agonist as needed for acute relief of symptoms (dyspnea and wheezing) 3.Add scheduled long-acting bronchodilator or Ipratropium; Possibly combination bronchodilators; Pulmonary rehabilitation |
|
|
How is Stage 3 COPD managed?
|
1. Smoking Cessation & vaccinations (influenza and pneumococcal)
2. Short-acting beta-agonist as needed for acute relief of symptoms (dyspnea and wheezing) 3.Add scheduled long-acting bronchodilator or Ipratropium; Possibly combination bronchodilators; Pulmonary rehabilitation 4. Combination bronchodilators Add inhaled steroid if the patient has repeated exacerbations |
|
|
How is stage 4 COPD managed?
|
1. Smoking Cessation & vaccinations (influenza and pneumococcal)
2. Short-acting beta-agonist as needed for acute relief of symptoms (dyspnea and wheezing) 3.Add scheduled long-acting bronchodilator or Ipratropium; Possibly combination bronchodilators; Pulmonary rehabilitation 4. Combination bronchodilators Add inhaled steroid if the patient has repeated exacerbations 5. Long-term O2/Surgery |
|
|
What is the effect of Smoking Cessation on COPD?
|
|
|
|
Vaccination recommendations for COPD patients
|
|
|
|
What is the mainstay therapy for stable COPD?
|
Bronchodilators
|
|
|
Which drug therapy can alter the progression of COPD
(i.e. the long-term rate of decline in FEV1) |
No drug therapy alters the progression of the disease (i.e, long-term rate of decline in FEV1)
|
|
|
Bronchodilator Therapy Pearls for COPD
|
|
|
|
Short-acting β2-Agonists
|
|
|
|
What are common side effects of the Short-acting β2-Agonists?
|
|
|
|
How are Short-acting β2-Agonists dosed?
|
|
|
|
Long-acting β2-Agonists
|
|
|
|
How are Salmeterol and Formoterol dosed?
|
|
|
|
How is Arformoterol dosed?
|
|
|
|
Anticholinergics
|
|
|
|
Tiotropium Bromide
|
Tiotropium Bromide SPIRIVA® HandiHaler
|
|
|
How is Tiotropium Bromide dosed?
|
Dosing: inhale contents of
one capsule every 24hrs (once daily) (dry powder inhaler) |
|
|
What are common side effects of Tiotropium Bromide?
|
Most common side effect = dry mouth (> ipratropium), rarely other anticholinergic side effects (worsening symptoms of BPH or arrowangle glaucoma)
|
|
|
Ipratropium bromide
|
Ipratropium bromide (Atrovent HFA®)
|
|
|
How is Ipratropium bromide dosed?
|
Dosing: 2-3 puffs MDI (with spacer) or 500 mcg solution every 6hr
|
|
|
What are common side effects of Ipratropium bromide?
|
Well tolerated: most common side effect = dry mouth, bitter taste
|
|
|
What agent is a last line option for COPD due to it's narrow therapeutic index and significant side effects?
|
Theophylline
|
|
|
Combination Brochodilator Options
|
|
|
|
Ipratropium + Albuterol MDI
|
Ipratropium + Albuterol MDI
(Combivent®) |
|
|
What role do Inhaled Corticosteroids (ICS) have in the treatment of COPD?
|
|
|
|
What are the GOLD guideline recommendations for ICS?
|
Use in symptomatic patients with an FEV1 < 50% predicted (stages 3 & 4) and repeated exacerbations (> 1 exacerbation per year)
|
|
|
ICS used in COPD
|
Fluticasone (Flovent HFA®)
•Best evidence for efficacy; reduces symptoms & exacerbation rate; improved health status •1-2 puffs (220-440 mcg) q12hrs (MDI) Budesonide (Pulmicort Flexihaler®) •Short-term improvement in FEV1; Effect on QOL & exacerbations not reported •2 puffs (360 mcg) q12hrs (DPI) |
|
|
Combination Inhaled Therapies
(LA B2-agonist + Steroid) |
|
|
|
Inhaled Steroid + LA B2-agonist agents used in COPD
|
Fluticasone/salmeterol (Advair HFA®)
•Comes in three different strengths. •FDA-approved for Asthma •Dosing: 2 puffs q12hrs (MDI) Budesonide/Formoterol (Symbicort®) •Recently FDA-approved for COPD •Dosing: 2 puffs q12hrs (Inhalation Aerosol) Fluticasone 250 or 500 mcg/salmeterol 50 mcg (Advair Diskus) •250/50 dose FDA-approved for patients with COPD •500/50 dose used in the large trials •Dosing: 1 puff q12hrs (DPI) |
|
|
Long-term oxygen therapy
|
|
|
|
Pulmonary Rehabilitation
|
|
|
|
Surgery
|
|
|
|
Patient Education in COPD
|
|
|
|
Suggested Management Plan for a patient with the following:
• 65 years old •chronic cough •progressive shortness of breath that has been getting worse •decreased exercise tolerance •hx of HTN and bronchitis •Smoker 1-2 ppd x 48 years •FEV1/FVC (post-broncho) = 0.60 •% predicted FEV1 (post-broncho) = 57% |
Our patient is stage 2 COPD
1. Smoking cessation and vaccination (flu and pneumococal) 2. Long-acting beta agonist or long-acting anticholinergic for chronic maintenance 3. Short acting beta agonist q4-6h prn (rescue inhaler) |
|
|
Suggested Management Plan for a patient with the following:
• 65 years old •chronic cough •progressive shortness of breath that has been getting worse •decreased exercise tolerance •hx of HTN and bronchitis •Smoker 1-2 ppd x 48 years •FEV1/FVC (post-broncho) = 0.60 •% predicted FEV1 (post-broncho) = 45% • Patient's current therapy includes Tiotropium and prn Albuterol |
Our patient is stage 3 COPD
Add on a LABA or an ICS Last line consider theophylline |
|
|
Suggested Management Plan for a patient with the following:
• 65 years old •chronic cough •progressive shortness of breath that has been getting worse •decreased exercise tolerance •hx of HTN and bronchitis •Smoker 1-2 ppd x 48 years •FEV1/FVC (post-broncho) = 0.60 •% predicted FEV1 (post-broncho) = 45% • Patient's current therapy includes a LABA and prn Albuterol |
Our patient is stage 3 COPD
Add on Ipratropium or Tiotropium or an ICS Last line consider theophylline |

