![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Draw the anatomy underlying horizontal gaze.
|
|
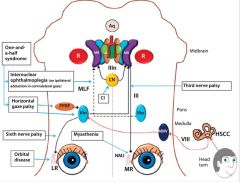
-Voluntary lateral gaze is governed by the parapontine reticular formation (PPRF), under cortical control by the contralateral frontal eye field.
-The PPRF excites the adjacent abducens nucleus (which stimulates the ipsilateral lateral rectus) and the contralateral medial rectus subnucleus of the oculomotor nucleus via the MLF (which stimulates the contralateral MR via a branch of CNIII). |
|
|
Draw the anatomy underlying vertical eye movement.
|
|
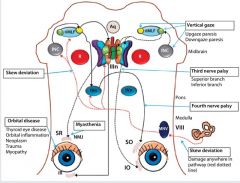
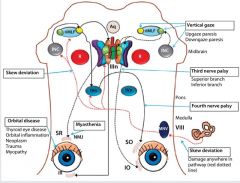
-Vertical saccades are governed by the rostral interstitial nucleus of the MLF (riMLF) in the midbrain, while the interstitial nucleus of Cajal (INC) is involved in smooth pursuit and maintenance of the eyes in eccentric vertical gaze.
-Downgaze: medial riMLF stimulates the ipsilateral IR subnucleus of IIIn (causing ipsilateral IR activation and this depression) and IVn (whose fibres decussate and cause contralateral SO activation and thus depression). -Upgaze: lateral riMLF stimulates IO subnucleus (activating ipsilateral IO) and SR subnucleus (whose fibres decussate and activate the contralateral SR) thus causing elevation. |
|
|
Describe the anatomical basis for skew deviation.
|
-The relative height of the two eyes is governed by afferents from the utricle that sense body or head tilt.
-Ipsilateral head tilt results in utricular activation, carried by the vestibular branch of CNVIII to the medial vestibular nucleus (medulla), which in turn activates compensatory contralateral depression and ipsilateral elevation. -Injury to this pathway mimics activation of the contralateral pathway, resulting in a pathologic vertical strabismus known as skew deviation. |
|
|
|
What is the differential localization of pure horizontal diplopia?
|
1. Pure medial or lateral rectus dysfunction, which can result from:
-Cranial neuropathies -Orbital pathology -Myasthenia gravis 2. INO |
|
|
|
What is the differential localization for a pure vertical diplopia?
|
1. Trochlear nerve palsy
2. Skew deviation (an imbalance in the vestibular-ocular signal governing ocular torsion and vertical alignment in response to body or head tilt). |
|
|
|
What syndrome is suggested by retinal pigmentary deposition in association with diffuse ophthalmoplegia suggests which syndrome?
|
The mitochondrial disease Kearns-Sayre syndrome.
|
|
|
|
List signs of orbital eye disease.
|
|
|
|
|
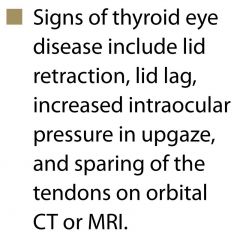
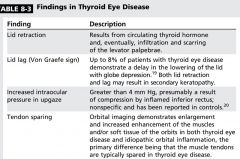
List signs of thyroid eye disease.
|
|
|
|
|
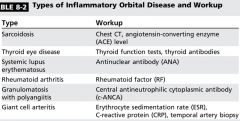
What etiologies can lead to orbital inflammation? What is the workup for each?
|
-Sarcoidosis
-Thyroid eye disease -SLE -Rheumatoid arthritis -Some vasculitides (including granulomatosis and rarely GCA) -IgG4 (a subclass of IgG that is linked with multiple forms of systemic inflammatory disease) has been linked with some cases of idiopathic orbital inflammation, particularly with inflammation of the eyelids, lashes, extraocular muscles, and lacrimal system. |
|
|
|
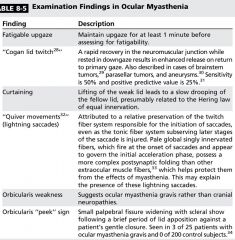
List 6 exam findings in ocular myasthenia.
|
|

|
|
|
What percentage of ocular myasthenia patients progress to generalized myasthenia?
|
-50-80%
-Almost all ocular myasthenia with the MuSK antibody generalizes. |
|
|
|
Which oculomotor subnucleus innervates the contralateral eye?
|
superior rectus subnucleus
|
|
|
|
Which cranial nerve has the longest course and is the only that exits the brainstem does ally? Does it decussate?
|
CNIV
Yes |
|
|
|
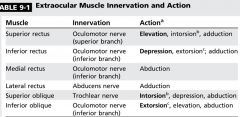
List the innervation and primary and secondary actions of the 6 extraocular muscles.
|
|
|
|
|
What are the findings of cavernous sinus lesions?
|

|
|
|
|
How can a CNIII nuclear lesion produce either bilateral ptosis or no ptosis?
|
Involvement or lack of involvement of the single subnucleus controlling the levator
|
|
|
|
What signs may be associated with fascicular CNIII lesions?
|
Hemiparesis
Ataxia Tremor (From involvement of adjacent corticospinal tracts, red nucleus, brachium conjunct, and cerebellar peduncles) |
|
|
|
What deficit results from a CNVI nuclear lesion?
|
-A nuclear lesion of the sixth nerve produces a gaze palsy due to the neurons innervating the contralateral medial rectus.
-A fascicular lesion produces an isolated abduction deficit. |
|
|
|
What findings may be associated with nuclear and fascicular CNVI lesions?
|
-Sixth nerve nuclear lesions can damage the adjacent medial longitudinal fasciculus and produce a one-and-a-half a syndrome.
-Fascicular lesions can be accompanied by hemiparesis, sensory change, or facial nerve palsy from involvement of the corticospinal tract, medial lemniscus, or seventh nerve fascicle. |
|
|
|
What are the 5 main differential localizations for multiple cranial neuropathies?
|
1. Cavernous sinus
2. Orbital Apex 3. CSF-based process affecting the nerves in the subarachnoid space 4. Neuromuscular junction process 5. Inflammatory cranial neuropathy |
|
|
|
What are the 4 main factors that need to be determined when evaluating an isolated CNIII palsy?
|
1. Is the pupil involved? (Larger than the other pupil and less reactive)
-Pupillary involvement is considered to be the hallmark of compressive third nerve palsies because the fibers serving the pupil are on the outside of the nerve. 2. Is the oculomotor involvement partial or complete? -The rule of the pupil only applies in the presence of complete motor involvement. Incomplete motor involvement with a normal pupil can be seen with aneurysmal or other compressive third nerve palsies early on. With progression motor involvement can become complete in the pupil becomes involved. |
3. Does the third nerve palsy effect only the superior division or inferior division?
-This divisional pattern would indicate an orbital process. 4. Are any signs of aberrant regeneration present? -Aberrant regeneration consists of an expected gaze movement producing an unexpected or aberrant response. -Aberrant regeneration can be seen after traumatic third nerve palsy or with a long-standing palsy from a compressive etiology (primary aberrant regeneration; usually caused by meningiomas but sometimes by aneurysms). |
|
|
What features on history and exam help distinguish a decompensated congenital CNIV palsy?
|
-Patients will frequently recall brief episodes of vertical diplopia in the past, usually associated with excessive fatigue or alcohol use.
-Patients frequently have long-standing head tilt to the side opposite the palsy as a method to reduce symptoms. -Some patients have facial asymmetry with the side of the face opposite the head tilt being slightly smaller. -The hallmark is increased vertical fusional amplitudes or greater than average ability to fuse to vertically misaligned images into a single image. The normal range is 1-4 prism diopters; patients with a decompensated congenital fourth near palsy typically have six or more prism diopters of vertical fusional amplitude. |
|
|
|
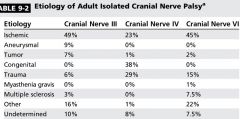
List the most common etiologies of CNIII, CNIV, and CNVI palsies by incidence.
|
|
|
|
|
What two initial questions should be asked in cases of multiple cranial neuropathies?
|
1. Are the involved nerves in a single anatomic localization (eg left third, fourth,and sixth nerve palsies from cabernous sinus process)?
2. Is any sensory involvement present? Myasthenia Gravis or Miller-Fisher syndrome can affect multiple cranial nerves but will have no sensory findings. |
|
|

What are the findings? What is the diagnosis?
|
A. Right gaze shows narrowed palebral fissure in the left eye.
B. Normal alignment in primary position. C . Left gaze shows limited abduction of the left eye. All of these findings are consistent with a congenital Duane syndrome. |
|
|
|
List 4 features that help distinguish Duane syndrome from cranial nerve palsy.
|
1. Duane syndrome is congenital, and most patients have suppression and do not report diplopia despite obvious misalignment.
2. In primary gaze, most patients are aligned despite marked limitations in abduction or adduction. This contrasts with CN palsies, in which you would expect misalignment in virtually all gaze positions, including primary gaze. 3. Duane syndrome frequently shows narrowing of the palpebral fissure with the adduction. 4. Retraction of the globe (best viewed from the side) occurs with adduction. |
|
|
|
What 3 features distinguish INO from a partial CNIII palsy?
|
1. Patients with an INO are aligned in primary position despite large adduction deficits. The exception to this rule is patients with bilateral INO who are exophoric, termed wall-eyed INO, or WEBINO.
2. Patients with INOs have no other signs of third nerve dysfunction, and a complete adduction deficit without other third nerve findings is extremely rare. 3. Patients with an INO can have an associated skew deviation, with the higher eye being on the side of the INO, that would not be seen with a third nerve palsy. |
|
|
|
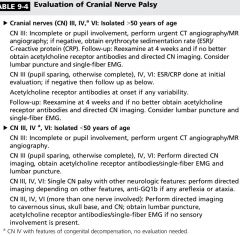
Describe the investigations for isolated CNIII, CNIV, and CNVI palsies in patients >50 years old and <50 years old.
|
|
|
|
|
What are saccades?
|
Saccades are the primary eye movement used in the visual exploration of the environment, rapidly moving the eyes in a conjugate fashion to foveate targets of interest. Saccades may be volitional or triggered involuntarily by head or environmental movement.
|
|
|
|
Do saccades occur in response to environmental stimuli in coma?
|
No. The machinery to generate saccades requires alertness; while slow phases may appear in coma, normal saccades are absent under these circumstances.
|
|
|
|
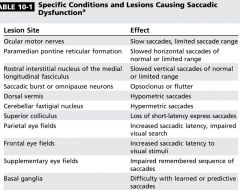
List 11 specific conditions and lesions causing saccadic dysfunction and their effect on saccades.
|
|
|
|
|
What is the function of optokinetic nystagmus? What is the localizing value of optokinetic nystagmus asymmetries?
|
1. Optokinetic nystagmus serves to maintain foveation on a portion of the moving object or scene as it travels across the retina, and consists of smooth pursuits and fast phases (saccades).
2. Although any postchiasmal lesion may produce a complete homonymous hemianopsia, an occipital lesion leaves OKN intact, while a parietal lesion affecting the optic radiations produces an OKN defect with stimuli rotated in an ipsilesional direction. |
|
|
|
When shifting gaze to a peripheral target of interest, one must generate an accurate saccade to the target, then supply appropriate innervation to maintain foveation on that target. How is this achieved?
|
-Saccadic movements achieve this through a pulse and step: the pulse of innervation rapidly moves the eyes to the target of interest; then a lower level of innervation, the step, is involved in maintaining gaze on the target.
-The nucleus prepositus hypoglossi, medial vestibular nucleus, and flocculus are the neural integrators. -Any mismatch in this calculation results in faulty gaze holding, with a pathologic slow phase back toward primary position driven by the elastic forces of the extraocular muscles within the orbit (gaze-evoked nystagmus). |
|
|
|
What features distinguish a skew deviation from a cranial nerve palsy?
|
-Ocular ductions are full in skew.
-The vertical misalignment may be comitant or incomitant in skew (a CN palsy is incomitant). -Uncrossed hypertropia is relatively common pattern in skew (right hypertropia in right gaze with left hypertropia in left gaze). -There is intorsion with the hypertropic eye in skew and extorsion with hypertropic CNIV palsy |
|
|
|
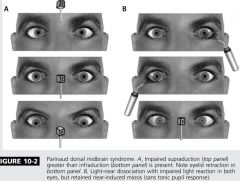
What are the 7 features of dorsal of midbrain syndrome?
|
1. Vertical gaze palsy
2. Vergence dysfunction (convergence spasm or paresis) 3. Light-near dissociation of the pupils 4. Eyelid retraction 5. Square-wave jerks 6. Convergence-retraction nystagmus 7. Skew deviation |
|
|
|
What is the differential diagnosis of light-near dissociation (poor pupillary response to light with retained brisk pupil response to a near target )?
|
-Parinaud dorsal midbrain syndrome
-Argyll Robertson pupils -Peripheral neuropathy with autonomic nerve involvement, severe afferent visual loss, or CNIII aberrancy |
|
|
|
Why is conjugate deviation of the eyes and head toward the side of the lesion (gaze preference) more common with right-sided, relatively smaller deficits involving the frontoparietal regions, but requires a larger lesion of the left hemisphere?
How do you confirm the lesion is supranuclear? |
-This right-left disparity is hypothesized to result from the predominant role of the right hemisphere in spatial orientation functions.
-The supranuclear nature of these lesions is confirmed by intact oculocephalic or caloric-induced VOR. |
|
|
|
How do you differentiate a gaze palsy from a gaze preference?
|
In contrast to a gaze preference, horizontal gaze palsy implies a lesion of the abducens nucleus within the pons that produces a ipsilesional gaze palsy that cannot be overcome by supranuclear activation by such as the oculocephalic maneuver.
|
|
|
|
What is the eight-and-one-half syndrome?
|
A lesion of the abducens nucleus, adjacent MLF, and the encircling facial nerve.
|
|
|
|
Dysfunction of the riMLF (eg due to infarction, demyelination, neoplasm, or neurodegenerative processes) produces slow or absent vertical saccades. What will the oculocephalic reflex or caloric testing show?
|
Given that the deficit is supranuclear, intact vertical eye movements may be possible when bypassing volitional pathways by activating the VOR.
|
|
|
|
1. What is the localization of selective loss of downgaze saccades?
2. What is the localization of loss of all downward eye movements? 3. What is the localization of loss of all upward eye movements? |
1. Bilateral riMLF lesions
2. Interstitial nucleus of Cajal or posterior commissure 3. Interstitial nucleus of Cajal or posterior commissure |
|
|
|
What are the oculomotor findings in PSP?
|
-Supranuclear paresis, initially for vertical but ultimately involving horizontal eye movements
-Slow saccades are often the initial ocular motor motor abnormality, and vertical saccades may take an oblique course (vertical saccades may trace an arc pattern including a horizontal trajectory, the round-the-house sign). -Horizontal saccades tend to be hypometric early -Frequent or continuous square-wave jerks (PSP has a lower blink rate and a higher rate of square-wave jerks than PD) -Impaired smooth pursuit -Eventually all volitional eye movements are lost (initially overcome with VOR) -Small fusional amplitudes producing persistent diplopia |
|
|
|
What is the hallmark oculomotor finding in idiopathic PD? What other oculomotor findings may be present.
|
-Hallmark: Vergence dysfunction producing convergence-insufficiency-related binocular horizontal diplopia at near distances.
-Additional ocular features may include square-wave jerks (lower rate than PSP), hypometric saccades, and impaired smooth pursuit. |
|
|
|
What is oculogyric crisis and what is the differential diagnosis?
|
-Oculogyric crisis is a dystonic reaction first described in relationship to the 1917 epidemic of encephalitis lethargica as part of the postencephalitis parkinsonism feature.
-Often preceded by a sense of fear -Associated features: eye pain, jaw spasm, retrocollis, and impaired communication -Currently seen in relationship to medications (most often dopamine antagonists such as antipsychotic agents or metoclopramide, but also phenytoin, carbamazepine, lamotrigine). -Can be aborted by anticholinergic medications |
|
|
|
If a patient has vertical diplopia at that worsens with downgaze, what is the differential for localization?
|
Inferior rectus or fourth nerve
|
|
|
|
The patient has horizontal diplopia that worsens with far vision, what is the differential for localization?
|
Lateral rectus or sixth nerve
|
|
|
|
Describe the exam technique to isolate the weak ocular muscle in horizontal diplopia.
|
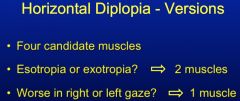
|
|
|
|
List six questions to ask in a patient presenting with double vision that may help you localize the anatomic site of dysfunction?
|
1. Does the double vision go away when closing either eye?
2. Are the two images separated vertically, horizontally, obliquely, or torsionally? 3. Is the diplopia worse at distance or at near? 4. In which direction is the double vision worse? 5. Is there a history of congenital strabismus or abnormal head position? 6. Is there associated pain, headache, or neurologic symptoms? |
|
|
|
Indicate which eye muscle you are testing in each position when performing versions and vergences.
|
1. Versions
-In lateral position: testing LR of the abducting eye and MR of the adducting eye -in lateral position, when the eye is moved superiorly: testing SR of abducting eye and IO of adducting eye -In lateral position, when the eye is moved inferiorly: testing IR of abducting eye and SO of adducting eye 2. Vergences -Convergence: both MR's -Divergence: both LR's |
|
|
|
What is the Hirschberg test?
|
Hirshberg test is used to detect a tropia by comparing the location of the reflection of a penlight on the cornea of both eyes.
|
|
|
|
What is the differential diagnosis for bilateral six nerve palsies?
|
1. Clivus lesion (metastatic, primary tumor, etc.)
2. Increased intracranial pressure 3. Idiopathic increased intracranial pressure |
|
|
|
Name three helpful localizing neighbourhood features of a nuclear fourth nerve palsy?
|
1. Contralateral fourth nerve palsy with ipsilateral INO (midline MLF)
2. Contralateral fourth nerve palsy with ipsilateral Horner's (descending sympathetics in the midbrain) 3. Contralateral fourth nerve palsy with contralateral RAPD (papillary axons in the brachium of the superior colliculus) |
|
|
|
Differentiate between the superior and inferior divisions of CNIII.
|
1. Superior division: levator palpebrae, superior rectus
2. Inferior division: papillary fibers via the ciliary ganglion, inferior rectus, medial rectus, and inferior oblique |
|
|
|
What disorder produces to Popeley of that is better in the morning and what disorder produces diplopia that is worse in the morning?
|
1. Better in the morning: myasthenia gravis
2. Worse in the morning: thyroid eye disease |
|
|
|
Give 2 differential diagnoses for aberrant regeneration of the third cranial nerve.
|
1. Cavernous sinus meningioma
2. Long-standing aneurysm |
|
|
|
Give a differential diagnosis for multiple cranial neuropathies from a cavernous sinus process.
|
-Vascular: cavernous sinus meningioma, aneurysm, cavernous sinus thrombosis
-Infectious: cavernous sinus infection -Tumour: cavernous sinus meningioma, pituitary adenoma, craniopharyngioma, sphenoid right wing meningioma -Autoimmune: sarcoidosis, Tolosa-hunt syndrome |
|
|
|
Give 7 differential diagnoses for multiple cranial neuropathies or subarachnoid/CSF space localization.
|
1. Carcinomatous meningitis
2. Chronic infections 3. Tuberculosis 4. Sarcoidosis 5. Miller Fischer syndrome (send anti-GQ1b) 6. Myasthenia Gravis (send anti-AchR Ab) 7. Lambert Eaton syndrome (arreflexia, proximal weakness, autonomic changes - send anti-VGCC) |
|
|
|
Describe the historical and examination features of a congenital strabismus causing ocular misalignment.
|
1. History of patching the eye, eye exercises, or special prism eyeglasses
2. No diplopia despite obvious ocular misalignment 3. Alignment is comitant (equal in all directions of gaze) |
|

