![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
125 Cards in this Set
- Front
- Back
|
What is the general cause of Congenital Heart Defects? |
Abnormal morphological development of the heart and/or great vessels that results in altered hemodynamic function
|
|
|
How common are Congenital Heart Defects? How many of these are severe?
|
- 6-8/1000 live births
- 33% of those children have a "severe" defect - 20% will die within 1st year of life |
|
|
What re the types of Congenital Heart Defects?
|
- Left to Right Shunt
- Right To Left Shunt (Cyanotic) - Congenital Obstructions |
|
|
When are Congenital Heart Defects noticed?
|
- Stillbirth
- At birth - Undetected until later in life - In 21st century they are detected earlier (fetal ultrasound) and treated better (surgical advances), but cause more chronic disease (because patients live longer) |
|
|
When do most Congenital Heart Defects arise?
|
Weeks 3-8 of embryogenesis
|
|
|
What are the most common causes of Congenital Heart Defects?
|
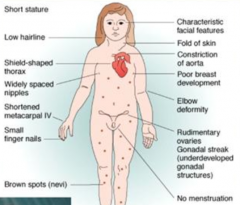
- Genetic: trisomies (13, 15, 18, 21), Turner syndrome (45,XO), monegenic disorders
- Environmental - Idiopathic (90%) |
|
|
What part of the fetus has the highest blood oxygen saturation? Adult?
|
- Fetus - umbilical vein (from placenta to fetus)
- Adult - pulmonary vein (from lungs to RA) |
|
|
What is a shunt?
|
- Abnormal communication between chambers or blood vessels
- Structural or functional |
|
|
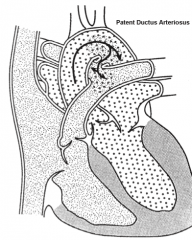
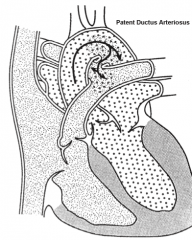
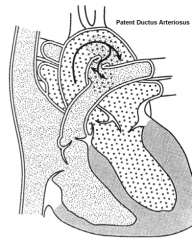
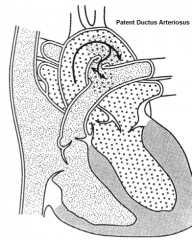
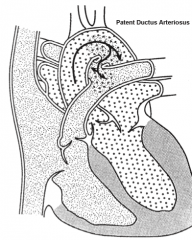
What are the types of Congenital Heart Defects that cause a Left-->Right shunt?
|
- Atrial Septal Defect (ASD)
- Ventricular Septal Defect (VSD) - Atrioventricular Septal Defect (AVSD) aka Endocardial Cushion Defect (ECD) - Patent Ductus Arteriosus (PDA) |
|
|
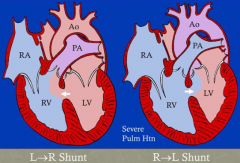
What makes a Left-->Right shunt clinically relevant?
|
- Physiologically left-to-right shunting of blood actually occurs
- Adding blood to R side of heart creates a volume overload on pulmonary circulation - If uncorrected, can progress to pulmonary vessel thickening, pulmonary hypertension, and right heart hypertrophy - This could cause shift to R-->L shunt which could cause cyanosis |
|
|
What are the types of Congenital Heart Defects that cause a Right-->Left shunt?
|
- Tetralogy of Fallot
- Transposition of Great Vessels - Truncus Arteriosus - Tricuspid Valve Atresia - TAPVR (Total Anomalous Pulmonary Venous Return) |
|
|
What makes a Right-->Left shunt clinically relevant?
|
- Causes bluing of mucous membranes and skin (cyanosis)
- Increase in amount of reduced (unoxygenated) hemoglobin in circulation (>1/3) - Deoxygenated blood gets into systemic circulation |
|
|
What are the types of Congenital Heart Defects that are caused by an Obstruction?
|
- Pulmonary Stenosis / Atresia
- Aortic Stenosis / Atresia / Hypoplastic Left Heart - Coarctation of the Aorta |
|
|
What makes an obstructive defect clinically relevant?
|
- Depends on whether it is from L or R side of heart
- L heart obstruction: increase in pulmonary circulation pressure (pressure overload) --> pulmonary venous hypertension --> left heart failure - R heart obstruction: insufficient blood flow to lungs --> hypoxia --> cyanosis (if R-to-L shunt present) --> eventually R heart failure |
|
|
What are the types of Congenital Heart Defects that are caused by valvular regurgitation?
|
Ebstein Anomaly
|
|
|
Which type of Congenital Heart Defect has cyanosis?
|
R-->L shunts
|
|
|
Which type of Congenital Heart Defect has late cyanosis?
|
L-->R shunts
|
|
|
What are the most common types of Congenital Heart Defects?
|
1) Ventricular Septal Defect
2) Patent Ductus Arteriosus (these two make up 75% of CHD) 3) Atrial Septal Defect 4) Transposition of Great Vessels 5) Tetraology of Fallot (these five make up 95% of CHD) |
|
|
What kind of tissue is estimated to be involved in formation 3/4 of Congenital Heart Defects?
|
Cardiac Mesenchyme (Cushion Tissue)
|
|
|
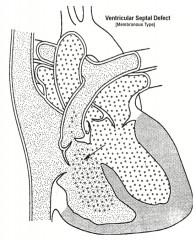
What is the most common major Congenital Heart Defect?
|
Ventricular Septal Defect (VSD) = 25% of all Congenital Heart Defects
|
|
|
Where do Ventricular Septal Defects occur?
|
- Opening between LV and RV
- 90% at septum (membranous portion) - Also can be in muscular portion (50% close spontaneously) |
|
|
What is the clinical picture of Ventricular Septal Defects?
|
- More common in males
- Murmur can be heard if there is shunting of blood across the defect - Usually associated with other anomalies (only 30% in isolation) |
|
|
What are the characteristics of a Membranous Ventricular Septal Defect (VSD)? Treatment?
|
- Most common type of VSD (90%)
- Defect is usually large - Spontaneous closure by septal TV leaflet only occurs <10% of cases - Requires surgical closure, usually ~1 year of age |
|
|
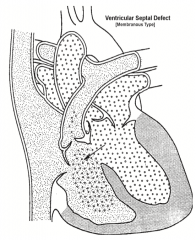
What are the characteristics of a Muscular Ventricular Septal Defect (VSD)? Treatment?
|
- Less common type of VSD (10%)
- Defect is usually small - Spontaneous closure by fibrous adhesions occurs in 60% by age 1 - Most do not require surgery - If there are multiple muscular VSDs = "swiss cheese septum" |
|
|
In what direction does blood flow through a Ventricular Septal Defect?
|
- L-->R shunt (oxygenated blood flows from LV to RV) because of high systemic pressure relative to pulmonic pressure
- This can cause severe pulmonary hypertension - This may convert the shunt to R-->L causing cyanosis |
|
|
What determines the magnitude of the Ventricular Septal Defect shunt?
|
- VSD size
- Pulmonary vascular resistance |
|
|
What are the four major complications of Ventricular Septal Defects (VSDs) that have significant shunts?
|
- CHF secondary to large volume L-->R shunt
- Pulmonary Hypertension w/ eventual reversal of shunt to R-->L shunt (Eisenmenger's syndrome) - LV dysfunction as a late consequence of chronic volume overload - Bacterial endocarditis |
|
|
What are potential late post-op complications of Ventricular Septal Defects?
|
- Endocarditis
- Aortic regurgitation - Tricuspid regurgitation - Heart block - LV obstruction |
|
|
What are the types/locations of Atrial Septal Defects (ASD)?
|
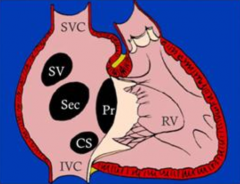
- Secundum type (most common, 90%) = at fossa ovale
- Primum type = at original ostium primum, adjacent to AV valves (5%) - Sinus Venosus type = near SVC entrance (5%) |
|
|
What are the clinical features of Atrial Septal Defects?
|
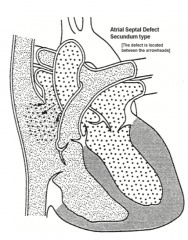
- Often asymptomatic until adulthood
- Can allow paradoxical embolism - <10% lead to pulmonary HTN - Murmur present if shunting occurs - More common in females |
|
|
What is the difference between a secundum type Atrial Septal Defect and a Patent Foramen Ovale?
|
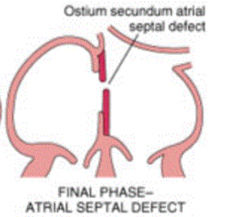
- ASD: rare, fenestrated or deficient fossa ovale, L-->R shunting, potential pulmonary hypertension and R-sided failure
- PFO: present in 1/3 of people, small remnant opening, no shunting (back pressure closes) except in rare cases, paradoxical emboli, decompression sickness, and migraines possible |
|
|
What is the direction of the shunt through an Atrial Septal Defect?
|
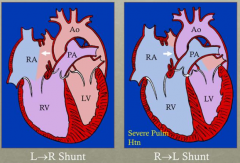
- Initial: L-->R shunt
- If progresses to severe pulmonary hypertension: R-->L shunt |
|
|
What are the long term effects of Atrial Septal Defects?
|
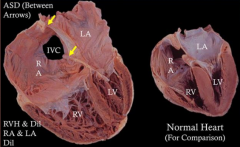
- Right Ventricular Hypertrophy and dilation
- Right Atrial and Left Atrial dilation |
|
|
What defect occurs in an Endocardial Cushion Defect (ECD)?
|
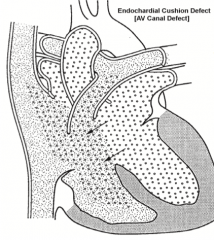
Atrioventricular Septal Defect / AV Canal Defect:
- Deficient AV septum - May also include Mitral valve and Tricuspid valve anomalies |
|
|
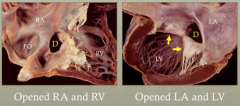
What are the types of Atrioventricular Septal Defect / Endocardial Cushion Defect?
|
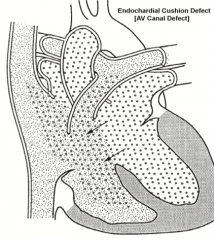
- Partial: primum atrial septal defect + cleft mitral valve w/ mitral regurgitation
- Complete: Atrioventricular Septal Defect + common AV valve defect |
|
|
What is Atrioventricular Septal Defect / Endocardial Cushion Defect associated with?
|
Down Syndrome, Trisomy 21 (40%) w/ complete AVSD
|
|
|
Which Congenital Heart Defect is associated with Down Syndrome?
|
Atrioventricular Septal Defect / Endocardial Cushion Defect
|
|
|
What are the clinical characteristics of Atrioventricular Septal Defect / Endocardial Cushion Defect?
|
- Mildest (bifid mitral valve) to severe (common AV canal)
- Associated with Down Syndrome - L-->R shunting - Murmur can be heard during systole and diastole |
|
|
What kind of Congenital Heart Defect causes a primum atrial septal defect, a cleft mitral valve, and mitral regurgitation?
|
Partial Atrioventricular Septal Defect
|
|
|
What kind of Congenital Heart Defect causes a common AV valve w/ 5 leaflets?
|
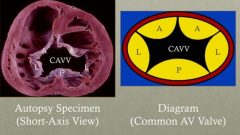
Complete Atrioventricular Septal Defect
|
|
|
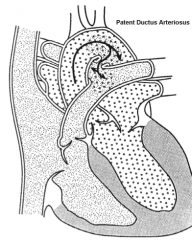
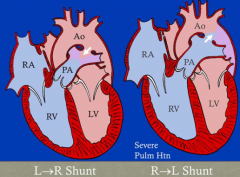
What does the Ductus Arteriosus form from?
|
Distal portion of L 6th pharyngeal arch artery
|
|
|
What does the Ductus Arteriosus connect?
|
Pulmonary trunk and Aorta
|
|
|
When does the Ductus Arteriosus close? What does it form?
|
- Normal functional closure: ~12 hours after birth
- Normal structural closure: ~3 months - Forms Ligamentum Arteriosum |
|
|
How can you delay the closure of the Ductus Arteriosus? When is it important to maintain the patency of the Ductus Arteriosus?
|
- Prostaglandin E1 (continuously infused)
- Necessary for survival in AV or PV atresia, others |
|
|
What determines the amount of shunting through the Patent Ductus Arteriosus (PDA)?
|
- Diameter of opening
- Difference in blood pressure between aorta and pulmonary trunk - Vascular resistance in systemic and pulmonary circulations |
|
|
What are the characteristic clinical findings associated with a Patent Ductus Arteriosus?
|
** Harsh, continuous "machinery-like" murmur
- Usually seen in isolation (90%) - Necessary for survival in AV or PV atresia, others |
|
|
What is the direction of blood through a Patent Ductus Arteriosus?
|
- Normal: L-->R shunt
- Can switch to R-->L shunt if there is severe pulmonary hypertension |
|
|
In fetal circulation, where does blood enter Ductus Arteriosus? How much?
|
85% of RV output directed across ductus arteriosus
|
|
|
What are the outcomes of a patent ductus arteriosus?
|
- Pulmonary resistance drops
- Pressure in aorta becomes significantly higher than pressure in pulmonary artery - Blood flows from aorta to pulmonary artery (L-->R shunt) via PDA - L-->R shunt sends extra already oxygenated blood back to lungs instead of out to body - Can lead to heart failure and poor growth |
|
|
How should an infant with a patent ductus arteriosus that develops heart failure be treated?
|
- PDA should be closed
- Can be closed using medicine early after birth that promotes spontaneous involution (Indomethacin) - Surgically through incision in left chest, suture ligation of PDA - Also can use an obstructing coil or plug to close PDA |
|
|
What medication can be used to close a Patent Ductus Arteriosus?
|
Indomethacin
|
|
|
When is maintaining the patency oft he Ductus Arteriosus important?
|
Provides blood flow to lungs when there is severe obstruction to pulmonary blood flow:
- Severe pulmonary stenosis or atresia - Right heart hypoplasia - Tricuspid stenosis or atresia Provides blood flow to body when there is severe obstruction to aortic blood flow: - Severe aortic stenosis - Left heart hypoplasia - Coarctation of aorta |
|
|
What are the right-to-left shunts / cyanotic heart defects?
|
- Tetralogy of Fallot
- Transposition of great arteries - Truncus arteriosus - Tricuspid atresia - Total anomalous pulmonary venous connection (TAPVC) |
|
|
What is the most common right-to-left shunt / cyanotic heart defect?
|
Tetralogy of Fallot
|
|
|
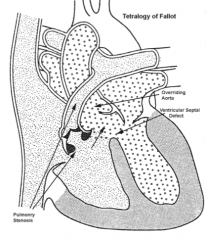
What are the features of the Tetralogy of Fallot?
|
1. Ventricular septal defect
2. Pulmonary trunk stenosis (d/t anterior displacement) 3. Aorta overrides opening to R and L ventricles 4. Right ventricular hypertrophy (called Pentology of Fallot if also has Atrial Septal Defect) |
|
|
What is the cause of Tetralogy of Fallot?
|
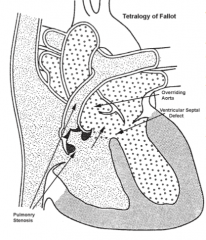
- Anterior-superior displacement of the infundibular septum
- DiGeorge Syndrome (22q11.2 deletion syndrome) is most common underlying genetic association - Next most common is Down Syndrome (trisomy 21) - Mutations in NKX2.5, JAG1, FOG27, trisomy 13, and CHARGE syndrome also associated w/ TOF |
|
|
What determines the clinical outcome of Tetralogy of Fallot?
|
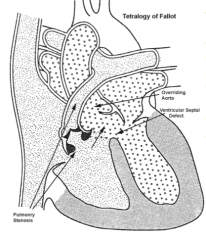
Severity of pulmonary trunk stenosis determines degree of cyanosis
|
|
|
What are the clinical features of Tetralogy of Fallot?
|
- Murmur present if significant pulmonary stenosis (systolic ejection murmur at left upper sternal border)
- Most common cyanotic heart defect - ± Tachypnea - More common in males - Heart appears boot-shaped due to RV hypertrophy - Gets worse with age d/t pulmonary outlet not growing with child |
|
|
How does the R-->L shunt of the Tetralogy of Fallot affect the lungs?
|
Does not damage the lungs because subpumonary stenosis restricts pulmonary blood flo
|
|
|
How do you treat the Tetralogy of Fallot?
|
- Initiation of IV PGE to maintain PDA to augment pulmonary blood flow
- Surgery required: shunt or complete repair |
|
|
What congenital heart defect is associated with DiGeorge Syndrome? What are the other symptoms?
|
Tetralogy of Fallot
- Phenotypic facies (microcephaly, small ears, hooded eyelids, cleft palate, etc) - Developmental delay / learning disability - Hypocalcemia (parathyroid under-development) - Immune deficiency (thymic hypoplasia) Truncus Arteriosus - Single vessel drains both ventricles- truncal artery - Large VSD |
|
|
What are the common side effects of PGE to monitor for?
|
- Apnea
- Fever - Hypotension at higher doses - Increased secretions - Gastric outlet obstruction w/ chronic use |
|
|
How do you manage a newborn with "PINK" Tetralogy of Fallot?
|
- Discharge home w/ close follow up at clinic
- Optimize growth w/ good nutrition - Discuss TOF spells w/ parents as degree of RVOT obstruction may change w/ age - Plan for operative repair at 3-6 months of age |
|
|
What are "Tet spells"?
|
- Profound and progressive cyanosis
- Disappearance of typical ejection fracture systolic murmur - indicates RVOT obstruction is so severe that there is no forward blood flow into pulmonary arteries or significant R to L shunting across VSD - Hyperpneic, irritable |
|
|
What should be done for a baby experienceing a hypercyanotic "tet" spell?
|
- Calm infant and provide supplemental oxygen
- Place in knee-to-chest position to increase systemic venous return to heart and augment blood flow across RVOT, also increases systemic vascular resistance (SVR) - IM morphine sulfate to abort spell or IV fluid bolus of saline - Other meds: IV ketamine, IV phenylephrine, beta blockers |
|
|
A complete operative repair of a Tetralogy of Fallot includes what?
|
- Patch closure of ventricular septal defect, so that blood in LV will flow into aorta
- Relief of RV outflow tract obstruction (pulmonary trunk stenosis) w/ muscle resection, RVOT patch placement to increase diameter, or placement of RV to PA conduit |
|
|
What are the long-term effects of a repaired Tetralogy of Fallot?
|
- Many have residual pulmonary regurgitation
- Pulm. regurgitation may become more severe w/ age and may cause RV dilation - Transannular patch repair have more pulmonary regurgitation and larger indexed RV end-diastolic volume than those w/ RV-->PA conduits - RV-PA conduits do not grow and need to be replaced w/ age |
|
|
Why might someone with a repaired Tetralogy of Fallot need re-operation later in life?
|
- If pulmonary regurgitation becomes significant and leads to RV dilation / dysfunction
- RV-VA conduits do not grow and need to be replaced w/ age - Timing of pulmonary valve replacement is controversial |
|
|
What is the quality of life for patients with a repaired Tetralogy of Fallot?
|
- Children/adolescents have QOL not proportional to severity of their residual disease
- They self-reported QOL similar to healthy peers, while parents reported lower QOL - QOL positively correlated w/ child's exercise capacity |
|
|
What occurs in the transposition of the great arteries?
|
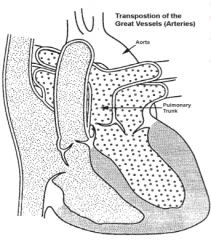
- Aorta arises from RV
- Pulmonary artery arises from LV |
|
|
What are the results of a complete transposition of the great vessels?
|
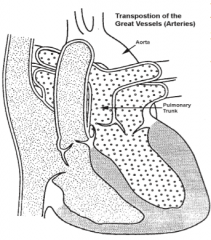
- Cyanosis if there is no shunt for mixing of blood
- RV hypertrophy develops - Pulmonary HTN develops unless pulmonary stenosis is present - No murmur |
|
|
What must happen to survive a transposition of the great vessels?
|
Shunt must be created or be occurring to allow oxygenated blood to get to the systemic circulation
|
|
|
Who is more likely to get a transposition of the great vessels? What is commonly seen with this defect?
|
- Males more likely
- 1/3 also have a VSD (good in this case because it allows mixing of blood) |
|
|
What are the two types of Transposition of the Great Vessels? How do they differ in outcomes?
|
- Intact Ventricular Septum (65%): unstable, needs prompt surgical intervention b/c relying on PDA to get oxygenated blood to systemic circulation (not sufficient)
- With Ventricular Septal Defect: stable (allows mixing of blood) |
|
|
When is a Transposition of the Great Vessels more likely?
|
Infants born to diabetic mothers, chromosomal and extra-cardiac abnormalities rare
|
|
|
What are mechanisms for an infant with transposed great vessels to get oxygenated blood to the systemic circulation?
|
Bidirectional shunting (mixing) via PFO/ASD, PDA, or VSD
|
|
|
What are the associated lesions with Transposition of the Great Vessels?
|
- Patent ductus arteriosus
- Ventricular septal defect - Pulmonary stenosis - Coronary artery abnormalities |
|
|
What outlet defects are associated with anterior deviation of the Conus Septum?
|
Subaortic obstruction / coarctation
|
|
|
What outlet defects are associated with posterior deviation of the Conus Septum?
|
Subpulmonary obstruction
|
|
|
How should you manage a patient with transposition of the great arteries?
|
- Oxygen
- Volume - Correct metabolic abnormalities - PGE1 - open/maintain ductal patency |
|
|
What should you do if after providing oxygen, PGE1 and correcting metabolic abnormalities, a baby with transposition of the great arteries is still profoundly desaturated (<70%)?
|
Balloon Atrial Septoplasty
|
|
|
What are the surgical methods for treating a transposition of the great arteries?
|
- Atrial Septectomy (survive <6 months)
- Atrial Swtich (Senning Repair) - long-term problems: RV dysfunction, sudden death d/t arrhythmias - Arterial switch (long term survival much better now) |
|
|
What is a Senning Procedure used to treat? What happens?
|
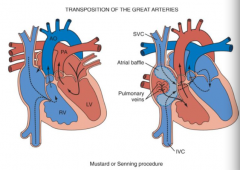
- Tx for transposition of great vessels
- Atrial switch |
|
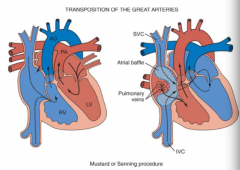
What are the complications of a Senning procedure for tx of transposition of the great vessels?
|
- Venous obstruction (systemic or pulmonary veins)
- Arrhythmias (atrial or sinus node dysfunction) - Systemic ventricle (RV) dysfunction |
|
|
What is a Jatene Procedure used to treat? What happens?
|
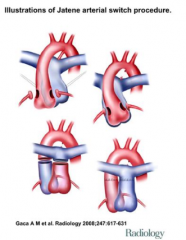
- Tx for transposition of great vessels
- Arterial switch |
|
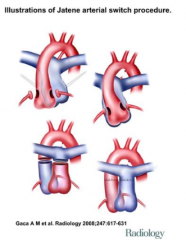
What are the complications of a Senning procedure for tx of transposition of the great vessels?
|
- Coronary issues (rare episodes of sudden death)
- Aortic root dilatation - Aortic insufficiency - Branch pulmonary artery stenosis - Generally, long-term outcomes are good |
|
|
What is the defect in Truncus Arteriosus?
|
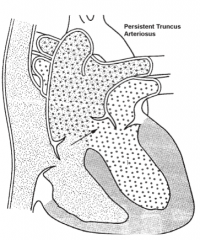
- Origin of aorta and pulmonary artery from truncal artery (single vessel empties both ventricles)
- Must have large VSD - Associated w/ DiGeorge Syndrome |
|
|
What causes Truncus Arteriosus?
|
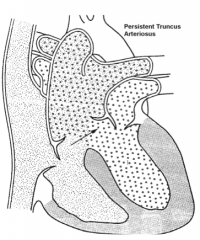
Developmental failure of separation of the embryologic truncus into the aorta and pulmonary artery
|
|
|
What are the outcomes of Truncus Arteriosus?
|
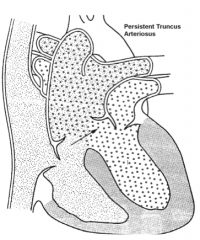
- Mixing of blood via VSD
- Increased pulmonary blood flow - Pulmonary hypertension |
|
|
What occurs in Tricuspid Atresia? Cause?
|

- Complete occlusion of the tricuspid valve orifice
- D/t unequal division of the AV canal - Cause: unequal division of the AV canal - mitral valve is enlarged |
|
|
What is necessary for Tricuspid Atresia survival? Outcomes?
|

- Need: Coexisting ASD/PFO and VSD
- Outcome: RV hypoplasia, symptomatic, high mortality |
|
|
What is the defect in Total Anomalous Pulmonary Vein Return (TAPVR)?
|
- Pulmonary veins do not directly drain into L atrium
- Causes L atrial hypoplasia - Instead, pulmonary veins connect via L innominate vein or coronary sinus - Occurs when pulmonary veins fail to develop or regress |
|
|
What is necessary for survival of Total Anomalous Pulmonary Venous Return?
|
ASD/PFO allows oxygenated blood to enter systemic circulation
|
|
|
What are the obstructive congenital heart defects associated w/ the L side of the heart?
|
- Coarctation of aorta
- Aortic Stenosis / Atresia - Hypoplastic Left Heart Syndrome |
|
|
What are the obstructive congenital heart defects associated w/ the R side of the heart?
|
Pulmonary stenosis / atresia
|
|
|
What is the defect that occurs in the Coarctation of the Aorta? What is the difference in the two types?
|
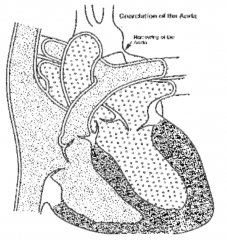
Narrowing of the aorta near the ductus arteriosus
- Preductal - tubular hypoplasia of the aorta by PDA (congenital) - Postductal - ridgelike infolding of aorta after ligamentum arteriosum, without PDA (adult) |
|
|
What is the clinical presentation of a child with Coarctation of the Aorta?
|
- Preductal narrowing of aorta accompanied by PDA --> lower body cyanosis
- Differential pulses in extremities - Heaving LV impulse at apex if LV volume overload - Systolic thrill possible in suprasternal notch - Murmur may occur d/t constriction of blood flow - Often associated w/ females w/ Turner Syndrome (45,XO) and is more common in males - 50% associated w/ bicuspid aortic valve |
|
|
What is the treatment for Coarctation of the Aorta?
|
- Requires surgery in neonatal period for preductal (e.g., end to end anastomosis)
- Also surgically treatable if postductal - Also catheterization techniques (percutaneous balloon angiplasty, percutaneous stenting) |
|
|
What is the clinical presentation of an adult with Coarctation of the Aorta?
|
- Postductal narrowing of aorta not accompanied by PDA
- Symptoms depend on degree of narrowing - Rib notching (chest x-ray) - HTN, upper>lower |
|
|
How does the Coarctation of the Aorta affect a fetus?
|
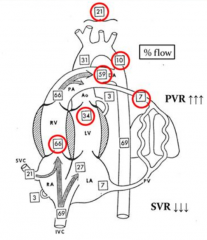
- Blood flow through aortic isthmus only constitutes about 10% of total aortic output
- 59% of blood flows through ductus arteriosus so it doesn't matter of the aorta is narrowed |
|
|
How does the Coarctation of the Aorta affect a newborn?
|
- Normall the ductus arteriosus constricts and pulmonary blood flow increases
- Flow through descending aorta increases - Pulmonary resistance drops and ductus reverses directions - Now there is a problem getting blood to the systemic circulation |
|
|
What is the defect in Aortic Stenosis? Aortic Atresia?
|
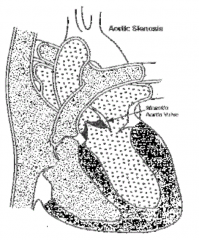
- Stenosis: Aortic valve obstruction d/t hypoplasia, dysplasia or abnormal number of cusps, causing narrowing of the opening/outlet
- Atresia: absence of aortic valve |
|
|
What are the outcomes of having Aortic Stenosis?
|
- LV must work harder --> hypertrophy
- LA dilatation - May lead to LV failure - Systolic murmur |
|
|
What are the outcomes of aortic valve atresia with an intact ventricular septum?
|
- Hypoplastic mitral valve and LV
- Dependent on PDA for survival - Requires staged surgical correction |
|
|
Why does the Ductus Arteriosus/Aorta close?
|
- Ductal tissue theory: result of migration of ductal smooth muscle cells into periductal aorta, with subsequent constriction and narrowing of the aortic lumen
- Hemodynamic theory: reduced volume through fetal aortic arch (10%) |
|
|
Which Congenital Heart Defect is associated with Turner (45,XO) syndrome?
|
Coarctation of the Aorta
|
|
|
What are the advantages and disadvantages of a transcatheter stent placement for Coarctation of the Aorta?
|
Advantages:
- Decreased stenosis related to vessel recoil (eliminates need for over-dilation) - Decreased incidence of late aneurysm formation Disadvantages: - Physiologic impact of a rigid aortic segment - Large sheath - Size of available stents/balloons may be limiting in little babies |
|
|
What is the normal aortic valve structure?
|
- Tri-leaflet valve
- 3 equal sized pocketlike cusps - Thin and mobile valve cusps - Valve tissue attached to a fibrous ring within aorta for support |
|
|
What does the aortic valve develop from?
|
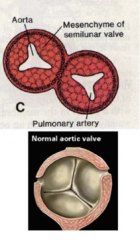
- 3 swellings of subendocardial mesenchyme
- Cavitation of these swellings forms the thin valve leaflets and sinuses |
|
|
What causes leaflet fusion and aortic stenosis?
|
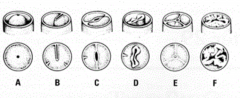
- Abnormal cavitation of the 3 subendocardial mesenchyme swellings
- Leads to decreased orifice size, increased thickening and rigidity of valve leaflets, and fusion of valve leaflets |
|
|
What happens to an aortic stenosis with time?
|
- Progressive - worsens over time d/t calcification and fibrosis of valve leaflets
- Aortic insufficiency may develop d/t annular dilation and valve degeneration - May cause LV failure from chronic ischemia |
|
|
How does Aortic Stenosis affect the fetus?
|
- Mild-moderate AS has no effect on fetal circulation
- Severe AS results in increased LV end-diastolic pressure which reduces flow of highly oxygenated blood from umbilical vein into LV and into aorta - Umbilical venous blood high in O2 is instead directed through RV where it mixes with SVC blood (low in O2) and then directed through DA into descending aorta and retrograde to ascending aorta *Blood lower in O2 content supplying brain and coronary arteries* |
|
|
How does Aortic Stenosis affect the neonate?
|
- Mild-severe AS have normal post natal circulation
- Critical AS dependent on DA for systemic blood flow |
|
|
What effect can aortic stenosis have on the left side of the heart?
|
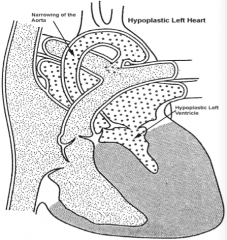
Hypoplastic Left Heart Syndrome
- Stenosis of Aortic Valve --> hypoplastic mitral valve and LV - Hypoplasia results because LV is not filled during development - Absence of filling is probably d/t mitral stenosis or oval foramen that closes too soon or is too small |
|
|
What other congenital defects are associated with Hypoplastic Left Heart Syndrome
|
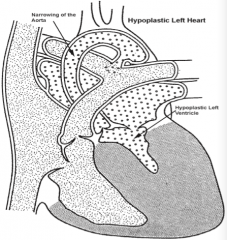
* Aortic Stenosis/Atresia & Mitral Stenosis or Oval Foramen that is too small
- Coarctation of Aorta |
|
|
What is necessary for survival in an infant with Hypoplastic Left Heart Syndrome?
|
Shunt between L and R heart needed for extrauterine survival
|
|
|
What is necessary for the chambers of the heart to develop normally?
|
They must be filled during formation
|
|
|
What defect is noticed in Pulmonary Stenosis / Atresia?
|
- Stenosis = narrowing of the pulmonary valve or outflow region of RV d/t hypoplasia, dysplasia, or abnormal number of cups
- Atresia = absence of pulmonary valve (very rare) |
|
|
What are the outcomes of Pulmonary Stenosis / Atresia?
|
- Right ventricle must work harder and results is RV hypertrophy
- Murmur is present - Cyanosis occurs only if a R-to-L shunt is present - Post stenotic injury to PA |
|
|
What are the characteristics of the Ebstein Anomaly?
|
* Affects Tricuspid Valve *
- Inferiorly displaced and adherent septal and posterior leaflets - Redundant anterior leaflet - Dilated annulus with tricuspid regurgitation - RV and RA dilatation - Arrhythmias, including WPW syndrome - May be asymptomatic until adulthood |
|
|
What defect causes a dilatation of the RA and the RV?
|
Ebstein Anomaly of the Tricuspid Valve
|
|
|
What occurs in Dextrocardia?
|
Right-sided heart - usually associated with situs inversus (5-10% have other cardiac anomalies, usually TGA)
|
|
|
What happens in Ectopia Cordis?
|
- Anterior thoracic wall fails to close properly
|
|
|
What are the symptoms of the Pentalogy of Cantrell?
|
1) Ectopia cordis - anterior thoracic wall fails to close
2) Ventricular septal defect 3) Sternal defect 4) Diaphragmatic hernia 5) Omphalocele (abdominal wall didn't close correctly leading to abdominal organs outside of body) |
|
|
What is the most common congenital heart defect? Which is the least worrisome?
|
- Most common: VSD
- Least worrisome: ASD |

