![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
prevalence of congenital heart disease
|
8/100 live births
most prevalent chromosomal abnormalities- most common in down's syndrome |
|
|
congenital heart disease and complications
|
respiratory infections
congestive heart failure hypoxemia growth restriction developmental delays pulmonary vascular disease failure to thrive death |
|
|
assessment of cardiac function and obstetrical history
|
genetic predisposition
maternal disease (rubella, IDDM) maternal age>40 maternal alcoholism environmental triggers- radiation, medication Down Syndrome Cytomegalo Virus |
|
|
assessment of cardiac function
|
feeding problems
FTT respiratory distress frequent respiratory infection exercise intolerance |
|
|
FTT
|
Failure To thrive
|
|
|
Assessment of cardiac function
|
PE:
cyanosis clubbing edema weak, absent or irregular pulses murmur |
|
|
Diagnosis of congenital heart disease
|
CXR- to assess size of heart
ECG- assess disruptions of rhythm echocardiogram- show flow of blood cardiac catheterization exercise stress test MRI-cellular level |
|
|
acyanotic defects
|
left to right shunt
-atrial Septal Defect -ventricular septal defect Patent Ductus Arteriosis |
|
|
Left to right shunt
|
through asd or vsd
increased work load of right side increased pulmonary blood flow -tachypnea -dyspnea -pulmonary edema -pulmonary hypertension heart failure right ventricular hypertrophy reverse right to left shunt |
|
|
pulmonary hypertension overtime causes...
|
pulmonary artery thickens and dilates from increase bp
|
|
|
signs and symptoms of left and right shunt
|
cardiac- tachycardia, right ventricular hypertrophy
Pulmonary- tachypnea, dyspnea, pulmonary edema, pulmonary artery hypertension |
|
|
Right ventricular hypertrophy
|
affected by strength of muscle
resistance |
|
|
atrial septal defect (ASD)
|
abnormal opening between right and left atria
altered hemodynamics -L atrial Pressure-->R atrial pressure so oxygenated blood flows into R atrium -extra volume is well tolerated by R ventricle |
|
|
ASD manifestations
|
systolic ejection murmur at 2nd-3rd interspace along LSB- Herbs point
|
|
|
Management of ASD
|
if defect is small, it may close spontaneously
if moderate to large, surgical closure by 2-4 yo |
|
|
Ventricular septal defects (VSD)
|
abnormal opening between left and right ventricles
blood flows from L ventricle to R ventricle |
|
|
VSD clinical manifestations
|
Loud harsh pansystolic murmur
FTT- due to poor eaters child older than 2 years may have: -frequent respiratory infection fatigue R-sided hypertrophy and CHF |
|
|
VSD management
|
if defect is small and child is asymptomatic or symptoms can be controlled- wait and hope for spontaneous closure
if large or uncontrolled by digoxin and diuretics-open heart surgery by year 1 |
|
|
Patent Ductus arteriosus (PDA)
|
occurs when ductus arteriosus doesn't close after birth
Pulmonary Artery has lower pressure than aorta, so blood will shunt from aorta into PA oxygenated blood is shunted into PA and recirculated thru lungs common in premies |
|
|
PDA manifestations
|
murmur at mid-upper LSB
enlargement of L atrium and L ventricle and possibly R ventricle Leads to CHF, child may have frequent resp infections and FTT |
|
|
PDA management
|
some may close spontaneously
surgical ligation of patent ductus may attempt to close ductus with indomethacin |
|
|
acyanotic obstruction defects
|
coarctation of the aorta
aortic stenosis pulmonary stenosis |
|
|
coarctation of aorta
|
narrowing of the aorta after the branches for the head and arms
location and degree of stricture vary increased pressure proximal to the defect decreased pressure distal to the defect |
|
|
coarctation of aorta manifestations
|
marked difference in BP of upper and lower extremities
weak or absent femoral pulses infants usually show some signs of ftt and chf hypertension, dizziness, fainting, HA, epistaxis Murmur may or may not be present can cause aortic anuerism |
|
|
management of coarctation of aorta
|
surgical repair recommended within first 2 years
resection with end-to-end anastomosis or enlargement using graft |
|
|
aortic stenosis
|
narrowing or stricture of aortic outflow tract
|
|
|
types of aortic stenosis
|
valvular- on valve
subvalvular- after valve supravalvular- before valve |
|
|
altered hemodynamics of aortic stenosis
|
resistance to ejection of blood from LV
LV hypertrophy increased LA pressure increased pressure in pulmonary veins pulmonary congestion/edema |
|
|
aortic stenosis manifestations
|
fainting
epigastric or anginal pain exercise intolerance dizziness after prolonged standing Murmer heard at 2nd intercostal space- aortic area |
|
|
aortic stenosis management
|
commissurotomy- open up valve further
incise fibrous ring in subvalvular type valve replacement |
|
|
Pulmonic stenosis
|
narrowing at entrance to pulmonary artery
cuspus of valve fused or malformed |
|
|
altered hemodynamics
|
blood cannot flow readily from RV to PA
|
|
|
pulmonic stenosis manifestations
|
systolic ejection murmur heard at 2nd intercostal space of LSB- pulmonic
Dyspnea on exertion fatigue majority of children with PS are asymptomatic growth and development normal edema from venous backup |
|
|
Pulmonic stenosis management
|
mild stenosis- watch
balloon angioplasty pulmonary valvulotomy |
|
|
Cyanotic Defects
|
Right-to-left shunt
tetralogy of fallot |
|
|
Right to Left shunt
|
deoxygenated blood shunted to left side
hypoxemia from deoxygenated blood being pumped to body Results: -polycythemia increased H&H Risk for thrombus acidosis |
|
|
polycythemia
|
increased RBC- cause of clots and strokes
|
|
|
tetralogy of Fallot
|
most common cyanotic defect
consists of 4 defects |
|
|
4 defects of tetralogy of fallot
|
1.pulmonary stenosis
2.VSD (usually large and high in septum) 3.overriding aorta- aorta right about vsd-makes it easy for deoxygenated blood to go into aorta 4.RV hypertrophy |
|
|
tetralogy of fallot altered hemodynamics
|
degree of pulmonary stenosis determines blood flow
will have R-to-L shunt of blood thru VSD if pulmonary stenosis is significant unoxygenated blood is forced thru VSD and out overriding aorta to systemic circulation |
|
|
manifestations of tetralogy of fallot
|
newborns may not be cyanotic initially
when PDA closes, pulmonic stenosis becomes more sever over time clubbing developmental delays pansystolic murmur at LLSB |
|
|
Tetralogy of fallot management
|
repair early
prior to surgery -supplemental iron to prevent iron-deficiency anemia -keep well-hydrated-prevents clots -avoid respiratory infection Lifelong -antibiotic prophylaxis and good dental hygiene to prevent bacterial endocarditis |
|
|
cyanotic mixed defects
|
transposition of great vessels
truncus arteriosis hypoplastic left heart syndrome congenital heart disease |
|
|
hypoplastic left heart
|
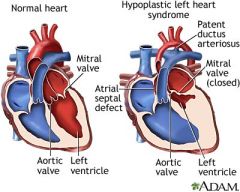
severely underdeveloped left side of heart
stenosis or closure of mitral and aortic valves may be asymptomatic until PDA closes Can cause sudden cyanosis and death |
|
|
transposition of the great vessels
|
pulmonary artery comes off the LV, aorta exits from RV
altered hemodynamics Not compatible with life unless there is also a VSD, ASD, or PDA to allow mixing of blood |
|
|
manifestations transposition of the great vessels
|
cyanosis always presents
CHF within first weeks of life hyperpnea murmur related to accompanying defect |
|
|
management of transposition of the great vessels
|
palliative measures until surgery can be done
prostaglandin to NB to keep PDA open Enlarge septal defect at time of cardiac catheterization with balloon to allow more mixing of blood corrective surgery |
|
|
truncus arteriosus
|
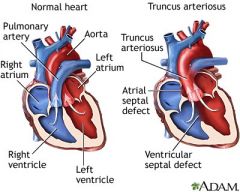
single vessel arises from both ventricles and overrides a VSD
single valve is often malformed, stenosed or incompetent |
|
|
truncus arteriosus and altered hemodynamics
|
blood from L and R ventricles mixes in truncus, flows to lungs and aorta
blood flow to lungs is greater |
|
|
truncus arteriosus manifestations
|
cyanosis
CHF systolic ejection murmur at LSB Bounding pulses in the upper extremity, and widened pulse pressure due to increased pulmonary blood flow |
|
|
truncus arteriosus management
|
first month- aggresive treatment of chf
surgical correction involves closing VSD |
|
|
Congestive heart failure
|
complication of congenital heart defects
inability of the heart to pump an adequate amount of blood to the systemic circulation to meet the body's metabolic demands |
|
|
Congestive heart failure due to the following...
|
volume overload
pressure overload decreased contractility high output demands |
|
|
congestive heart failure: Left-sided failure
|
LV end-diastolic pressure rises--> increases pressure in pulmonary veins-->lung congestion-->pulmonary edema
|
|
|
congestive heart failure: Right-sided failure
|
RV end-diastolic pressure rises-->increases central venous pressure-->systemic venous engorgement-->systemic venous hypertension-->hepatomegaly and edema
|
|
|
compensation of congestive heart failure
|
initially heart tries to compensate in two ways:
1. hypertrophy of cardiac muscle 2. tachycardia |
|
|
signs and symptoms of pulmonary congestion
|
Right-sided
tachypnea dyspnea orthopnea pleural effusion crackles, cough diaphoresis weakness, fatigue decreased urine output weak peripheral pulses decreased BP |
|
|
signs and symptoms of systemic congestion
|
sudden weight gain
edema ascites NVD Hepatomegaly Developmental delays |
|
|
Management of congestive heart failure
|
Reduce workload of heart
Digoxin- slows heart down and increase strength -monitor for signs of toxicity teach parents home care Nurtrition relieve respiratory distress prevent infection prevent skin breakdown |
|
|
signs of digoxin toxicity
|
low pulse, vomiting, see halos
|
|
|
ACE inhibitors
|
diuretics
monitor for signs of hypokalemia- heart dysrythmia, abdominal cramping, fluid restriction, Sodium restriction Decrease cardiac demands |
|
|
manifestations of rheumatic heart disease
|
strep infection 2-3 weeks prior
carditis, arthritis, chorea chronic progressive damage to heart and valves |
|
|
management of rheumatic heart disease
|
eradicating bacteria
10 days of PCN or erythromycin treat inflammation and fever corticosteroids NSAIDS Preventing permanent heart damage monthly injections of PVK Dental Prophylaxis |
|
|
assessment of rheumatic heart disease
|
History of sore throat
skin-maculopapular rash Neuro-chorea (jerky movements) Murmur painful joints |
|
|
Nursing management of rheumatic heart disease
|
teaching to assure compliance with antibiotics
allow verbalizations of frustrations of chorea Pain management steriods NSAIDS |
|
|
acyanotic
|
pulmonary blood flow
obstruction of blood flow from ventricles |
|
|
cyanotic
|
pulmonary blood flow
mixed blood flow |

