![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
142 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
eczema
|
?
|
|
|
|
amitriptyline
|
?
|
|
|
|
What is the ddx for child presenting with fever?
|
flu
ear infection UTI |
|
|
|
carotidynia
|
?
|
|
|
|
patellar tendonitis
|
?
|
|
|
|
osgood-schlatter disease
|
Osgood-Schlatter Disease
Osgood-Schlatter disease is apophysitis of the tibial tubercle resulting from repeated normal stresses or overuse. These repetitive stresses imposed by the patellar tendon on its site of insertion results in a series of microavulsions of the ossification center and the underlying cartilage. Inflammation causes patellar tendonitis and the development of a remarkable prominence, induration, and tenderness of the tibial tuberosity. There is no avascular necrosis of the tibial tubercle. Children are usually between 10 and 15 years of age at time of onset; it more commonly occurs in running or jumping athletes. Boys are affected more often than girls, and most cases are bilateral, although symptoms are commonly asymmetric. Clinical Features Signs and symptoms of Osgood-Schlatter disease are chronic, intermittent pain and tenderness over the anterior aspect of the knee and the tibial tuberosity. Pain is aggravated by activates such as running, kneeling, squatting, and climbing stairs, and pain improves with rest. On examination, there is a prominence and soft tissue swelling over the tibial tubercle. The patellar tendon is tender and thick. The remainder of the knee examination usually is normal, and there is no knee effusion. Radiographs are not essential, but are usually obtained. Radiographic findings of soft tissue swelling and irregularities of the tibial tubercle are nonspecific (Figure 133-28). The irregularity of the ossification of the tibial tubercle is normal in this age group. A lateral knee radiograph may show prominence of the tibial tuberosity, calcification in the tibial tubercle region, or separate ossicles from the anterior border of the tubercle. Treatment The disease is self limited, and most patients' symptoms respond to rest and temporary avoidance of the offending activity. However, complete avoidance of activity or sports is not essential. Immobilization is actually contraindicated and can lead to rapid atrophy of the quadriceps muscle. Physical therapy and flexibility exercises to stretch and strengthen the quadriceps and hamstring muscles may help to alleviate stress on the tubercle and avoid recurrences. Applying ice after activity may decrease swelling, and pain can be controlled with NSAIDs. Corticosteroids should not be injected into the patellar tendon or para-apophyseal soft tissues. Parents should be provided reassurance that the condition is benign and self-limited and will resolve after closure of the proximal tibial growth plate. Rarely, an ossicle may persist after skeletal maturity that causes pain and may require excision. |
|
|
|
What is the pediatric dosing of amoxicillin for acute otitis media?
|
80-90mg/kg/day x 10 days
|
|
|

|
Lateral radiograph illustrating Osgood-Schlatter disease with prominence of the tibial tuberosity in addition to ossicles separate from the anterior border of the tubercle (arrow).
|
|
|
|
What's the difference between virgin, extra virgin, and pure olive oil?
|
Whether an oil is considered to be extra virgin, virgin or pure olive oil is in the oil's acidity. The acidity has more influence on taste than on nutrition although the lower the acidity the higher the antioxidant content.
|
|
|
|
Amitriptyline is indicated for?
|
depression
tension HA peripheral neuropathy chronic pain |
|
|
|
What is a less greasy substitute for vaseline?
|
aquaphor (ointment)
|
|
|
|
List the following in most effective to least effective against dry skin: lotion, cream, ointment.
|
ointment > cream > lotion
|
|
|
|
What are the characteristics of acute eczema?
|
pruritus
erythema vesiculation |
|
|
|
What are the characteristics of chronic eczema?
|
pruritus
xerosis lichenification fissuring hyperkeratosis |
|
|
|
What are the risk factors and behaviors associated with contracting HIV/AIDs?
|
unprotected sex
shared needles blood transfusion perinatal transmission |
|
|
|
List the types of skin biopsy.
|
1. shave biopsy
2. punch biopsy 3. incisional biopsy 4. excisional biopsy |
|
|
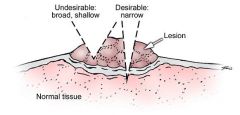
What type of skin biopsy is this?
|
incisional biopsy
|
|
|
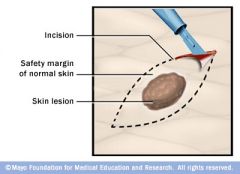
What type of skin biopsy is this?
|
excisional biopsy
|
|
|
|
Define exanthem?
|
generalized skin rash; caused by infectious disease, autoimmune disease, or drugs/toxins
|
|
|
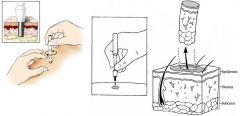
What kind of skin biopsy is this?
|
punch biopsy
|
|
|
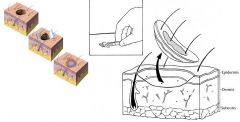
What kind of skin biopsy is this?
|
shave biopsy
|
|
|
|
Define enathem?
|
mucosal membrane rash; often accompanying an exanthem
|
|
|
|
Define cellulitis.
|
diffuse inflammation of connective tissue
|
|
|
|
How do you differentiate oral candidiasis from oral leukoplakia?
|
candidiasis will wipe off (and bleed when scraped) while leukoplakia will not
|
|
|
|
What is oral candidiasis?
|
yeast infection of the mouth
|
|
|
|
Name 9 dermatological disorders due to fungal infection.
|
tinea capitis
tinea barbae tinea corporis tinea manuum tinea cruris tinea pedis tinea unguium/onychomycosis tinea versicolor candidiasis |
|
|
|
Candida albicans is part of normal flora, true or false?
|
true
found in oropharynx, large intestine, and vagina |
|
|
|
VULVOVAGINAL CANDIDIASIS
|
ETIOLOGY:
infection caused by fungi candida albicans (90%) candida albicans is normal flora found in mouth, vagina, and feces but is also an opportunistic pathogen risk factors include pregnancy, obesity, DM, HIV, antibiotics, corticosteroids, oral contraceptives, chronic debilitation affects 75% of women in their lifetime CLINICAL PRESENTATION: severe vulvar pruritis vulvar erythema white cottage-cheesy vaginal discharge +/- burning following urination +/- dyspareunia +/- labia minora erythema, excoriation, edema if affecting skin adjacent to labia, think DM or other systemic illness DIAGNOSTIC WORKUP: pH normal (≤4.5) wet mount (KOH) → pseudohyphae fungal culture MANAGEMENT: 1. treat only if symptomatic 2. clotrimazole 100 mg vaginal tab x 7 days 3. miconazole 200 mg vaginal suppository x 3 days 4. fluconazole 150 mg PO single dose 5. d/c antibiotics if possible 6. control underlying disease COMPLICATIONS: recurrence common → fluconazole 150 mg PO weekly for maintenance therapy PATIENT EDUCATION: avoid nonabsorbent undergarments avoid douching |
|
|

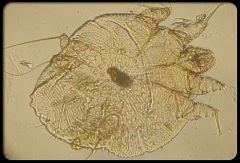
What does this wet mount slide indicate?
|
budding yeast (6) and pseudohyphae (7) of candida → vulvovaginal candidiasis
|
|
|
|
Describe scabies burrows.
|

irregular, 2-3mm long, width of hair
|
Current p137
|
|

|
scabies
|
|
|

|
scabies
|
|
|

|
scabies
|
|
|
|
scabies
|
|
|
|
What are the indications for prescribing permethrin 5% cream?
|
scabies
|
|
|

|
scabies burrow
|
|
|
|
What dermatomes are most commonly affected in herpes zoster?
|
thoracic and lumbar roots
|
Current p1241
|
|

|
herpes zoster
|
|
|
|
What are aggravating factors for herpes outbreaks?
|
trauma
infection sun exposure stress |
Current p113
|
|

|
genital herpes
|
|
|

|
genital herpes
|
|
|

|
oral herpes
|
|
|

|
oral herpes
|
|
|
|
SEBORRHEIC KERATOSES:
|

ETIOLOGY:
cause unknown, suspected genetic and UV light associations originates from keratocytes common, especially in elderly and on sun-exposed areas benign CLINICAL PRESENTATION: plaque, 3-20 mm, beige to black velvety or warty surface appear stuck or pasted to skin DIAGNOSTIC WORKUP: +/- biopsy to r/o melanoma or other cutaneous neoplasm MANAGEMENT: no treatment necessary if pruritic or inflamed → currettage or cryotherapy COMPLICATIONS: none PATIENT EDUCATION: common and benign |
|
|
|
What are seborrheic keratoses?
|

benign plaques with velvety or warty appearance that appear stuck or pasted to skin
|
|
|

|
seborrheic keratosis
|
|
|

|
seborrheic keratosis
|
|
|
|
What is another name for atypical nevus?
|
atypical mole
dysplastic nevus |
|
|
|
ATYPICAL NEVI:
|

ETIOLOGY:
benign mole with atypical features originates from melanocytes 5-10% of white Americans have ≥1 atypical nevi increased risk of melanoma if: 1. ≥50 typical nevi + ≥1 atypical nevi + 1 ≥8mm nevi 2. many atypical nevi CLINICAL PRESENTATION: ≥6 mm color non-uniform border irregular DIAGNOSTIC WORKUP: none → diagnosis of atypical nevi made clinically not histologically +/- biopsy if suspect melanoma MANAGEMENT: f/u every 6-12 months with dermatologist using dermatoscopy f/u more frequently if many atypical nevi + positive FH for melanoma since 50% develop melanoma by 50y/o COMPLICATIONS: melanoma PATIENT EDUCATION: monitor for changes in moles over time and consult provider if change noticed use mnemonic ABCDE to detect significant changes: A = shape asymmetric B = border irregular C = color non-uniform D = diameter ≥6 mm E = lesion evolving or changing over time |
|
|
|
What is an atypical nevus?
|
benign mole that may resemble melanoma d/t large size, multi-coloration, and irregular border
|
|
|
|
What are the criteria for detecting atypical nevi/melanoma?
|
use mnemonic ABCDE to detect significant changes:
A = shape asymmetric B = border irregular C = color non-uniform D = diameter ≥6 mm E = lesion evolving or changing over time |
|
|
|
What does the mnemonic ABCDE stand for?
|
mnemonic for detecting atypical nevi or melanoma where:
A = shape asymmetric B = border irregular C = color non-uniform D = diameter ≥6 mm E = lesion evolving or changing over time |
|
|

|
malignant melanoma
|
|
|

|
malignant melanoma
|
|
|
|
What is melanoma?
|
malignant neoplasm of melanocytes
|
|
|
|
What is the most deadly skin disease?
|
malignant melanoma
|
|
|
|
MALIGNANT MELANOMA:
|

ETIOLOGY:
malignant neoplasm originating from melanocytes most deadly skin disease, particularly of whites 1 in 4 melanomas occur before 40y/o CLINICAL PRESENTATION: irregular topography → partly flat and partly raised irregular notched border with pigment leaking into normal surrounding skin non-uniform color → may include white, pink, red, blue, gray, black recent change in appearance of pigmented skin lesion "ugly duckling sign" → mole stands out from other moles on individual bleeding or ulceration DIAGNOSTIC WORKUP: dematoscopy → to help determine if biospy needed (95% sensitive, 85% specific) excisional biopsy histological types include: 1. lentigo maligna melanoma → arising from chronically sun-exposed skin of older individuals 2. superficial spreading malignant melanoma → arising from intermittently sun-exposed individuals 3. nodular malilgnant melanoma 4. acral lentiginous melanoma → arising on palms and soles as dark irregular shaped lesions; arising on nail beds as solitary dark broad longitudinal streaks; particularly affects dark-skinned individuals 5. mucous membrane malignant melanoma MANAGEMENT: excision → histological diagnosis → re-excision with margins dicated by tumor thickness → sentinel lymph node biopsy if >1 mm thick lesion or high-risk histologic features or intermediate-risk without adenopathy refer if white, pink, blue, gray, or black colored refer if intermediate or high-risk COMPLICATIONS: prognosis determined by tumor thickness, lymph node involvement, distant metastases 10-year survival rate is 95% if <1mm, 80% if 1-2 mm, 55% if 2-4 mm, and 30% if >4 mm 5-year survial rate is 30% if lymph node involvement and <10% if distant metastases PATIENT EDUCATION: monitor for changes in moles over time and consult provider if change noticed use mnemonic ABCDE to detect significant changes: A = shape asymmetric B = border irregular C = color non-uniform D = diameter ≥6 mm E = lesion evolving or changing over time |
|
|
|
What is dermatoscopy?
|
use of a special magnifying device to evaluate pigmented lesions
|
|
|

|
solar lentigo d/t chronic sun damage
|
|
|

|
solar lentigo d/t acute sun burn
|
|
|

|
tinea capitis
|
|
|
|
What are lentigines?
|
solar lentigo
|
|
|
|
SOLAR LENTIGO:
|
ETIOLOGY:
localized proliferation of melanocytes d/t acute or chronic sun exposure may arise after sunburns or PUVA overdose usually occurs if >40y/o, white/asian, skin phototype I-III similar to freckles but acquired and does not fade with lack of sunlight CLINICAL PRESENTATION: macule round or oval 3-5 mm (according to Current), 1-5 cm (according to Fitzpatrick) light yellow, light brown, or dark brown; non-uniform in color circumscribed or irregular ill-defined border (especially on back) located in sun-exposed areas → forehead, nose, cheeks, upper chest, upper back, dorsum of forearms/hands, shins do not fade with lack of sun exposure scattered discrete stellate and sharply defined after acute sunburn DIAGNOSTIC WORKUP: ddx includes freckles, seborrheic keratosis, spreading pigmented actinic keratosis, lentigo maligna r/o neoplasm MANAGEMENT: 1. topical tretinoin 0.1% 2. topical tazaroten 0.1% 3. topical 4-hydroxyanisole 2% with tretinoin 0.01% (Solage) 4. cryotherapy → no more than 10s should be administered, otherwise depigmentation of normal skin can occur 5. laser surgery COMPLICATIONS: none PATIENT EDUCATION: benign reduce sun exposure or wear sun screen |
|
|

|
tinea corporis
|
|
|

|
solar lentigo
|
|
|

|
dermatofibroma
|
|
|
|
TINEA CAPITIS:
|

ETIOLOGY:
fungal infection of hair and/or scalp caused by Trichophyton tonsurans (90%) or Microsporum canis (10%) CLINICAL PRESENTATION: thickened, broken-off hairs 2-3 mm from follicle leaving “black dot” appearance erythema and scaling of underlying scalp +/- diffuse pustules on scalp +/- boggy fluctuant mass (kerion) on scalp suggesting exaggerated host response MANAGEMENT: 1. wood lamp → Trichophyton tonsurans doesn’t fluoresce, Microsporum canis fluoresces yellow-green 2. KOH 3. fungal culture 4. oral griseofulvin (take with fatty meal to increase absorption) 5. continue fungal cultures every 4 weeks 6. continue medication 4 weeks following negative fungal culture |
|
|

|
dermatofibroma
|
|
|
|
What is the treatment for tinea unguium/onychomycosis?
|
1. terbinafine 250mg tablets PO daily x 6 weeks (fingernails) or 12 weeks (toenails)
2. order HFP mid-way through treatment to screen for hepatotoxicity |
|
|
|
What is a skin lesion "dimple sign"?
|

depression of skin lesion with lateral pressure
ddx includes: dermatofibroma blue nevus papulonodular lesions containing mucin pilar cyst scar Kaposi sarcoma dermatofibrosarcoma protuberans metastatic carcinoma |
|
|

|
tinea pedis
|
|
|
|
TINEA CORPORIS, CRURIS, MANUUM, PEDIS & UNGUIUM
|

ETIOLOGY:
fungal infection usually caused by Trichophyton mentagrophytes, Trichophyton rubrum, Microsporum canis, Epidermophyton floccosum CLINICAL PRESENTATION: tinea corporis → annular marginated plaques with a thin scale and clear center or annular confluent dermatitis tinea cruris → symmetrical, sharply marginated lesions in inquinal areas tinea pedis → red scaly lesions on soles of feet or fissuring between toes tinea unguium (onychomycosis) → yellowed, thickened, crumbling nails MANAGEMENT: 1. KOH → scrape thin scales from border of lesion, positive for hyphae 2. fungal culture 3. treat tinea corporis, tinea cruris, and tinea pedis with topical → imidazoles, allylamines, benzylamines, or ciclopirox applied twice daily x 3-4 weeks 4. treat tinea unguium with griseofulvin (if refractory, try itraconazole or terbinafine) |
|
|
|
What is a dermatofibroma?
|

benign button-like nodule usually located on extremities
|
|
|

|
tinea cruris
|
|
|
|
DERMATOFIBROMA:
|

ETIOLOGY:
benign composed of disordered collagen cause unknown, possibly late reaction to arthropod bite common in adults, females>males CLINICAL PRESENTATION: dermal papule or nodule button-like, domed; dull, shiny, or scaling texture 3-10 mm color variable; skin-colored, pink, tan, brown, dark brown; darker at center, fading to normal skin at margin ill-defined border d/t fading at margin firm, +/- tenderness usually solitary usually located on extremities, legs>arms>trunk appear gradually over several months DIAGNOSTIC WORKUP: if pigmented r/o malignant melanoma MANAGEMENT: cryosurgery with a cotton-tip applicator COMPLICATIONS: none PATIENT EDUCATION: benign may persist without enlargement for years or decades may regress spontaneously |
|
|
|
What is another name for tinea versicolor?
|
pityriasis versicolor
|
|
|
|
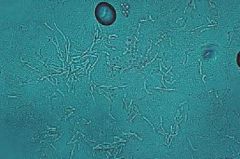
KOH revealing short hyphae and spores d/t tinea versicolor
|
|
|

|
tinea versicolor
|
|
|

|
tinea unguium
|
|
|

|
tinea versicolor
|
|
|
|
What genus of fungus causes tinea versicolor?
|
Malassezia
|
|
|
|
"Spaghetti and meatballs" KOH indicates?
|

hyphae and spores indicatives of tinea versicolor
|
|
|
|
A fungal culture is useful in diagnosing tinea versicolor, true or false?
|
false
|
|
|
|
TINEA VERSICOLOR:
|

ETIOLOGY:
superficial skin infection caused by the fungi genus Malassezia normal skin flora CLINICAL PRESENTATION: asymptomatic, rarely pruritus macules 4-5mm to large confluent areas white, pink or tan hypo or hyperpigmentation velvety fine scales only seen when scraping lesion usually located on upper trunk, sometimes neck, upper arms and groin DIAGNOSTIC WORKUP: skin scraping → KOH → large blunt hyphae and thick-walled budding spores AKA "spaghetti and meatballs" fungal culture not useful MANAGEMENT: 1. selenium sulfide lotion → apply from neck to waist for 5-15 min daily x 7 days → repeat weekly x 1 month, then monthly for maintenance 2. ketoconazole shampoo 1% or 2% → apply to chest and back for 5 min 3. ketoconazole 200mg PO daily x 1 week (risk of drug-induced hepatitis) 4. ketoconazole 400mg PO single dose (may not work in hot/humid areas) 5. fluconazole 300mg PO two doses 14 days apart 6. imidazole creams, solutions or lotion (effective but expensive) COMPLICATIONS: 80% recurrence over 2 years without maintenance therapy PATIENT EDUCATION: Selsun Blue Dandruff Shampoo can be bought OTC and contains selenium sulfide hypo or hyperpigmentation may take months to return to normal apply lotion/shampoo weekly or monthly for maintenance therapy exercise before and do not shower for 8-12 hours after oral ketoconazole ingestion because it is delivered via sweat to skin |
|
|
|
What is the ddx for annular skin lesions?
|
tinea corporis
→ positive KOH pityriasis rosea → lesions more numerous than tinea corporis syphilis → lesions on palms, soles, mucous membranes psoriasis → lesions on scalp, elbows, knees, nails lupus erythematosus granuloma annulare → lesions lack scales |
|
|

|
tinea cruris
|
|
|

|
tinea corporis
|
|
|

|
tinea corporis
|
|
|

|
tinea corporis and pedis
|
|
|
|
What is the common name for tinea cruris?
|
jock itch
|
|
|
|
What is the ddx for rashes in the intertriginous groin area?
|
tinea cruris → KOH reveals hyphae
erythrasma → wood's lamp reveals coral-red fluorescence candidiasis → bright red with satellite papules/pustules outside main border of lesion; involves scrotum seborrheic dermatitis → also involves face, sternum, axillae intertrigo → more red, less scaly, extension onto thigh; often in obese individuals psoriasis → distinct plaques |
|
|

|
candidal diaper dermatitis
|
|
|

|
erythrasma in axillary fold
|
|
|
|
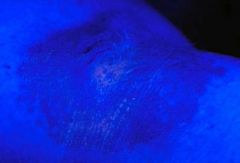
wood's lamp reveals coral-red fluorescence indicative of erythrasma
|
|
|
|
TINEA PEDIS, CRURIS:
|
ETIOLOGY:
fungal infection usually caused by Trichophyton rubrum (most common), Trichophyton mentagrophytes, Microsporum canis, Epidermophyton floccosum CLINICAL PRESENTATION: tinea corporis → +/- pruritus, erythematous ring-shaped lesions with central clearing and advancing scaly border or scaly patches with distinct border; found on trunk or exposed areas such as face and arms tinea cruris → asymptomatic or marked pruritus, sharply marginated lesions with central clearing and spreading scaly peripheries, located in groin and gluteal cleft, usually sparing scrotum tinea pedis → red scaly lesions on soles of feet or fissuring between toes tinea unguium (onychomycosis) → yellowed, thickened, crumbling nails DIAGNOSTIC WORKUP: skin scraping from scales at border of lesion → KOH → hyphae fungal culture MANAGEMENT: 1. tinea corporis → topical clotrimazole, miconazole, butenafine or terbinafine (all OTC) twice daily until 1-2 weeks after clearing; griseofulvin 250-500 mg PO twice daily x 4-6 weeks; itraconazole 200 mg PO daily x 7 days; terbinafine 250 mg PO daily x 1 month 2. tinea cruris → topical clotrimazole, miconazole, ketoconazole etc (all OTC) twice daily until 1-2 weeks after clearing; terbinafine cream daily x 7 days; griseofulvin 250-500 mg PO twice daily x 1-2 weeks; itraconazole 200 mg PO daily x 7 days; terbinafine 250 mg PO daily x 7 days 2. tinea unguium → griseofulvin (if refractory, try itraconazole or terbinafine) COMPLICATIONS: tinea corporis → extention of disease down hair follicles making it more difficult to cure; pyoderma tinea cruris → reoccurence common; can apply drying powder miconazole nitrate if excessive perspiration or obesity PATIENT EDUCATION: treat infected household pets (Microsporum infections) tinea corporis → usually responds to tx within 4 weeks tinea cruris → possible hyperpigmentation upon resolution |
|
|
|
ERYTHRASMA:
|
ETIOLOGY:
superficial skin infection caused by gram-pos bacteria Corynebacterium minutissiumum part of normal skin flora (bacillus, aerobic or facultatively anaerobic, non-spore forming) affects adults risk factors include obesity, hyperhydrosis, occlusive clothing/shoes, warm/humid climate CLINICAL PRESENTATION: asymptomatic red or tan patches scaling at sites not continuously occluded excoriation or lichenification if pruritic symmetric, sharply marginated located in intertriginous areas; toe webspaces >> inguinal folds > axillae > submammary, subpanniculus, intergluteal toe webspaces may be macerated, eroded or fissured; may have dematophytosis, candidiasis, or pseudomonal coconmitant infection DIAGNOSTIC WORKUP: Wood's lamp → coral-red fluorescence d/t presence of coproporphyrin III (may not be present if patient bathed recently) bacterial culture → positive for corynebacterium, helps r/o staph, strep KOH → negative for hyphae, helps r/o candida MANAGEMENT: 1. topical benzoyl peroxide 2.5% gel daily after showering x 7 days 2. topical erythromycin or clindamycin twice daily x 7 days 3. topical sodium fusidate ointment 4. topical mupirocin ointment or cream 5. topical clotrimazole, miconazole or econazole 6. oral macrolide or tetracycline x 7 days COMPLICATIONS: reoccurence if risk factors not corrected PATIENT EDUCATION: post-inflammatory hyperpigmentation may occur in heavily melanized individuals reoccurence if risk factors not corrected prophylaxis tx include applying medicated powders, washing with benzoyl peroxide, applying isopropyl or ethanol topical antiseptic alcohol gels |
|
|
|
What is aphthous stomatitis?
|

canker sore
|
Mosbys p339
|
|
|
What are other names for aphthous stomatitis?
|
aphthous ulcer
ulcerative stomatitis canker sore |
Current p203
|
|
|
What is the etiology of aphthous stomatitis?
|
unknown; possible association with HHV6
may be 2° to: drug allergies erythema multiforme herpes simplex pemphigus pemphigoid epidermolysis bullosa acquisita bullous lichen planus Behçet disease IBD |
Current p203
|
|
|
What is the clinical presentation of aphthous stomatitis?
|

painful small round ulceration with yellow-gray fibroid center
surrounded by red halo single or multiple found on labial or buccal mucosa recurrent |
Current p203
|
|
|
What is the management of aphthous stomatitis?
|
for symptomatic relief → prescribe topical corticosteroids → triamcinolone acetonide 0.1% (group IV potency) or fluocinonide 0.5% (group II potency)
|
Current p203
|
|
|
How long does healing take for aphthous stomatitis?
|
healing takes 10-14 days if <1cm
|
Current p203
|
|
|
Define photophobia.
|
abnormal sensitivity to light
|
|
|
|
Define diplopia.
|
double vision
|
|
|
|
What is the ddx for altered visual acuity?
|
refractive error
corneal opacities cataract uveitis vitreous hemorrhage retinal detachment involving the macula diabetic retinopathy central retinal vein occlusion central retinal artery occlusion macular degeneration optic nerve disorders |
|
|
|
What is the ddx for floaters?
|
benign vitreous opacities
posterior vitreous detachment vitreous hemorrhage posterior uveitis |
|
|

|
black arrow = external hordeolum
white arrow = chalazion |
|
|
|
HORDEOLUM (AKA STYE):
|
staphyloccocal abscess
characterized by a localized red, swollen, tender area on upper or lower lid external hordeolum is on lid margin and smaller internal hordeolum is a meibobian gland abscess and points onto conjunctival surface of lid tx: warm compresses abx ointment (bacitracin or erythromycin) applied to eyelid q3hr during acute stage incision if no resolution within 48hr internal hordeolum may lead to cellulitis |
|
|
|
CHALAZION:
|
granulomatous inflammation of meibomian gland
may follow internal hordeolum characterized by hard, non-tender swelling on upper or lower eyelid with redness and swelling of adjacent conjunctiva tx: I&D steroid injection may cause vision distortion if large enough to impress cornea |
|
|
|
What is the bulbar (AKA ocular) conjunctiva?
|
thin mucous membrane; cover and protects anterior surface of eye except cornea and surface of eyelid in contact with the globe
|
Mosbys p280
|
|
|
Describe the pathway of tears.
|
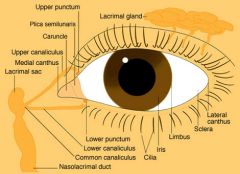
produced by lacrimal gland → flow over eye → drain via upper and lower punctum → upper and lower canaliculi → lacrimal sac → nasolacrimal duct → nasal meatus
|
Mosbys p280
|
|
|
Define ptosis.
|

drooping of the eyelid
|
|
|

|
ptosis of RT eye
|
|
|
|
Define entropion.
|

inversion of eyelid → may cause eyelashes to irritate cornea and conjunctiva → may lead to infection; patients often complain of foreign body sensation
|
Mosbys p289
|
|
|
Define extropion.
|

eversion of eyelid → may cause excessive tearing since inferior punctum is turned outward and unable to collect tears from lacrimal gland
|
Mosbys p289
|
|
|
What is blepharitis?
|

inflammation of the eyelid
|
|
|

|
hordeolum
|
|
|

|
blepharitis
|
|
|
|
What is palpebral AKA tarsal conjunctiva?
|
conjunctiva lining eyelids
|
|
|
|
sharply demarcated bright red area with healthy conjunctiva surrounding it indicates?
|

subconjunctival hemorrhage
|
|
|

|
subconjunctival hemorrhage
|
|
|

|
ectropion
|
|
|

|
entropion
|
|
|
|
Define pterygium.
|
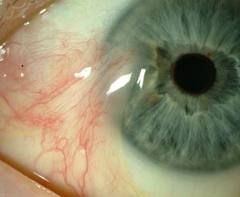
benign growth of the conjunctiva that extends over the cornea; commonly occurs on nasal side; can interfere with vision if advances over pupil
|
Mosbys p291
|
|

|
pterygium
|
|
|
|
What is bulbar conjunctiva?
|
membrane covering anterior eye except cornea
|
|
|
|
What is a corneal ulcer?
|
disruption of the corneal epithelium and stroma due to desiccation or infection
|
Mosbys p306
|
|

|
fungal-associated corneal ulcer
|
|
|
|
What is the diagnostic workup of apthous stomatitis?
|
incisional biopsy if diagnosis unclear to r/o SCC
|
|
|
|
What is the etiology of obstructive sleep apnea?
|
anatomically narrowed airway
nasal obstruction alcohol or sedatives before sleep hypothyroidism smoking most common in obese middle-aged men |
|
|
|
What is the diagnostic workup of obstructive sleep apnea?
|
sleep studies → apneic episodes with hypoxemia
pulse ox nocturnal pulse ox → normal rules out obstructive sleep apnea PFTs EKG → arrhythmias |
|
|
|
What is the clinical presentation of obstructive sleep apnea?
|
fatigue
daytime somnolence snoring obesity |
|
|
|
What is the management of obstructive sleep apnea?
|
weight loss
avoid alcohol and sedatives nasal continuous positive airway pressure (nasal CPAP) at night surgical options |
|
|
|
What polysomnography results indicate sleep apnea?
|
results reported using apnea-hypopnea index (AHI)
5-15 = mild sleep apnea 15-30 = moderate sleep apnea >30 = severe sleep apnea |
|
|
|
A "true" UTI is indicated by what 2 lab criteria?
|
1. only 1 significant organism detected on culture
2. >100,000 CFU/mL detected on culture |
|
|
|
What is the treatment for bacterial conjunctivitis for infants vs children?
|
infants = erythromycin ophthalmic ointment
(ointment interferes with vision but is preferred d/t prolonged contact with ocular surface + soothing effect) children = tobramycin ophthalmic drops (drops do not interfere with vision) |
|
|
|
What is the treatment for impetigo?
|
mupirocin topical 2%
|
|
|
|
What is vicodin made up of?
|
hydrocodone + acetaminophen
most commonly prescribed as 5mg hydrocodone + 500mg acetaminophen |
|
|
|
What is hydroxazine (brand vistaril)?
|
1st-generation antihistamine
effective for insomnia,anxiety, nausea, pruritus |
|
|
|
After performing a scoliosis screening, how would you document the RT shoulder is higher than the left?
|
RT thoracic concave curvature
|
|
|
|
What is the Pediarix vaccine composed of?
|
DTaP
HepB Polio |
|
|
|
What type of fracture is indicated by tenderness in the snuff box?
|
scaphoid fracture of the hand
|
|

