![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
176 Cards in this Set
- Front
- Back
|
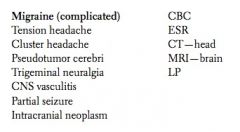
21 yo F presents with several episodes of throbbing left temporal pain that lasts for 2–3 hours. Prior to its onset, she sees flashes of light in her right visual field and feels weakness and numbness on the right side of her body for a few minutes. Headaches are often associated with nausea and vomiting. She has a family history of migraine. |
|
|
|
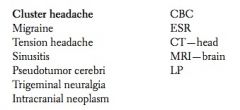
26 yo M presents with terrible right temporal headaches associated with ipsilateral rhinorrhea and eye tearing and redness. Episodes have occurred at the same time every night for the past week and last for 45 minutes.
|
|
|
|
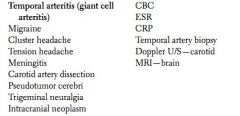
65 yo F presents with severe, intermittent right temporal headache, fever, blurred vision in her right eye, and pain in her jaw when chewing.
|
|
|
|
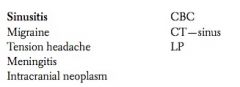
30 yo F presents with frontal headache, fever, and nasal discharge. There is pain on palpation of the frontal and maxillary sinuses. She has a history of sinusitis.
|
|
|
|
50 yo F presents with recurrent episodes of bilateral squeezing headaches that occur 3–4 times a week. She is experiencing significant stress in her life.
|
|
|
|
35 yo M presents with sudden severe headache, vomiting, confusion, left hemiplegia, and nuchal rigidity.
|
|
|
|
25 yo M presents with high fever, severe headache, confusion, photophobia, and nuchal rigidity. Kernig’s and Brudzinski’s signs are positive.
|

|
|
|
18 yo obese F presents with headache, vomiting, and blurred vision for the past 2–3 weeks. She is taking OCPs.
|
|
|
|
47 yo M c/o daily pain in the right cheek over the past month. The pain is electric in character and occurs while he is shaving. Each episode lasts 2–4 minutes.
|
|
|
|
Key elements Hx in HA?
Key elements in PE of HA? |
Hx: Location (especially unilateral vs. bilateral), quality, intensity, duration, timing (does it disturb sleep?); presence of associated neurologic symptoms, nausea, jaw claudication; recent trauma, dental surgery, si- nusitis symptoms; exacerbating (stress, fatigue, menses, exercise) and alleviating factors (rest, medicines); past history of headache; family history of migraines.
PE: Vital signs; inspection and palpation of entire head; ENT inspection; complete neurologic exam, includ- ing funduscopic exam. |
|
|
Confusion/Memory Loss:
Key in Hx? Key in PE? |
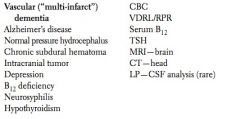
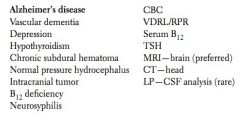
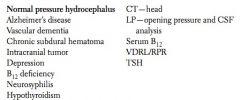
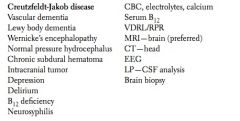
Hx: Must include history from family members/caregivers. Detailed time course of cognitive deficits, associ- ated symptoms (constitutional, incontinence, ataxia, hypothyroid symptoms, depression); screen for delirium (waxing/waning level of alertness); ADL/IADL status, falls, medications (and recent medication changes); history of stroke or other atherosclerotic vascular disease, syphilis, HIV risk factors, alcohol use, or vitamin B12 deficiency; family history of Alzheimer’s disease.
PE: Vital signs; complete neurologic exam, including mini-mental status exam and gait; general physical exam, including ENT, heart, lungs, abdomen, and extremities. |
|
|
81 yo M presents with progressive confusion over the past several years together with forgetfulness and clumsiness. He has a history of hypertension, diabetes mellitus, and two strokes with residual left hemiparesis. Mental status has clearly worsened after each stroke.
|
|
|
|
84 yo F brought by her son c/o forgetfulness (e.g., forgets phone numbers, loses her way back home) along with difficulty performing some of her daily activities (e.g., bathing, dressing, managing money, using the phone). The problem has gradually progressed over the past few years.
|
|
|
|
72 yo M presents with memory loss, gait disturbance, and urinary incontinence for the past six months.
|
|
|
|
55 yo M presents with a rapidly progressive change in mental status, inability to concentrate, and memory impairment for the past two months. His symptoms are associated with myoclonus and ataxia.
|
|
|
|
70 yo insulin-dependent diabetic M presents with episodes of confusion, dizziness, palpitation, diaphoresis, and weakness.
|
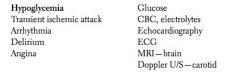
|
|
|
55 yo F presents with gradual altered mental status and headache. Two weeks ago she slipped, hit her head on the ground, and lost consciousness for two minutes.
|
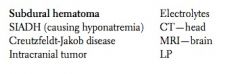
|
|
|
Dizzyness:
Key in HX: Key in PE: |
Hx: Lightheadedness vs. vertigo, ± auditory symptoms (hearing loss, tinnitus), duration of episodes, context (occurs with positioning, following head trauma), other associated symptoms (visual disturbance, URI, nausea); neck pain or injury; medications; history of atherosclerotic vascular disease.
PE: Vital signs; complete neurologic exam, including Romberg test, nystagmus, tilt test (e.g., Dix-Hallpike maneuver), gait, hearing, and Weber and Rinne tests; head and neck exam; cardiovascular exam. |
|
|
35 yo F presents with intermittent episodes of vertigo, tinnitus, nausea, and hearing loss over the past week.
|
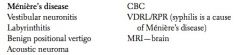
|
|
|
55 yo F c/o dizziness for the past day. She feels faint and has severe diarrhea that started two days ago. She takes furosemide for her hypertension.
|
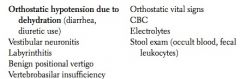
|
|
|
65 yo M presents with postural dizziness and unsteadiness. He has hypertension and was started on hydrochlorothiazide two days ago.
|
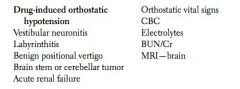
|
|
|
44 yo F c/o dizziness on moving her head to the left. She feels that the room is spinning around her head. Tilt test results in nystagmus and nausea.
|
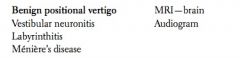
|
|
|
55 yo F c/o dizziness that started this morning. She is nauseated and has vomited once in the past day. She had a URI two days ago and has experienced no hearing loss.
|
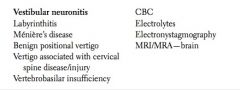
|
|
|
55 yo F c/o dizziness that started this morning and of “not hearing well.” She feels nauseated and has vomited once in the past day. She had a URI two days ago.
|
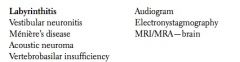
|
|
|
LOC: Key elems in ...
Hx? PE? |
HX: Presence or absence of preceding symptoms (nausea, diaphoresis, palpitation, pallor, lightheadedness), context (exertional, postural, traumatic; stressful, painful, or claustrophobic experience; dehydration); as- sociated tongue biting, incontinence, tonic-clonic movements, prolonged confusion; dyspnea or pul- monary embolism risk factors; history of heart disease or arrhythmia; alcohol and drug use.
Key Physical Exam Vital signs, including orthostatics; complete neurologic exam; carotid and cardiac exam; lung exam. |
|
|
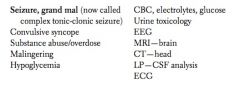
26 yo M presents after falling and losing consciousness at work. He had rhythmic movements of the limbs, bit his tongue, and lost control of his bladder. He was subsequently confused (as witnessed by his colleagues).
|
|
|
|
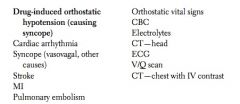
55 yo M c/o falling after feeling dizzy and unsteady. He experienced transient LOC. He has hypertension and is on numerous antihypertensive drugs.
|
|
|
|
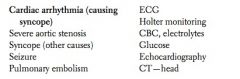
65 yo M presents after falling and losing consciousness for a few seconds. He had no warning prior to passing out but recently had palpitations. His past history includes coronary artery bypass grafting (CABG).
|
|
|
|
Numbness/weakness - Key elems of ...
Hx PE |
Hx: Distribution (unilateral, bilateral, proximal, distal), duration, ± progressive, pain (especially headache, neck or back pain); constitutional symptoms, other neurologic symptoms; history of diabetes, alcoholism, atherosclerotic vascular disease.
Key Physical Exam Vital signs; neurologic and musculoskeletal exams; relevant vascular exam. |
|
|
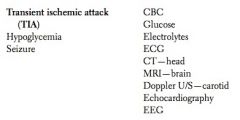
68 yo M presents following a 20-minute episode of slurred speech, right facial drooping and numbness, and right hand weakness. His symptoms had totally resolved by the time he got to the ER. He has a history of hypertension, diabetes mellitus, and heavy smoking.
|
|
|
|
68 yo M presents with slurred speech, right facial drooping and numbness, and right hand weakness. Babinski’s sign is present on the right. He has a history of hypertension, diabetes mellitus, and heavy smoking.
|
|
|
|
33 yo F presents with ascending loss of strength in her lower legs over the past two weeks. She had a recent URI.
|
|
|
|
30 yo F presents with weakness, loss of sensation, and tingling in her left leg that started this morning. She is also experiencing right eye pain, decreased vision, and double vision. She reports feeling “electric shocks” down her spine upon flexing her head.
|
|
|
|
55 yo M presents with tingling and numbness in the hands and feet (glove and stocking distribution) over the past two months. He has a history of diabetes mellitus, hypertension, and alcoholism. There is decreased soft touch, vibratory, and position sense in the feet.
|
|
|
|
40 yo F presents with occasional double vision and droopy eyelids at night with normalization by morning.
|
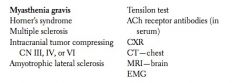
|
|
|
25 yo M presents with hemiparesis (after a tonic-clonic seizure) that resolves over a few hours.
|
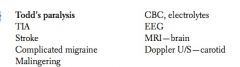
|
|
|
Fatigue and sleepiness - Key elems of ...
Hx PE |
Hx:
Duration; sleep hygiene, snoring, waking up choking/gasping, witnessed apnea; overexertion; stress, de- pression, or other emotional problems; diet; weight changes; other constitutional symptoms; symptoms of thyroid disease; history of bleeding or anemia; medications; alcohol and drug use. Key Physical Exam Vital signs; head and neck exam (conjunctival pallor, oropharynx/palate, lymphadenopathy, thyroid exam); heart, lung, abdominal, and neurologic exams; consider rectal exam and occult blood testing. |
|
|
40 yo F c/o feeling tired, hopeless, and worthless and of having suicidal thoughts. She recently discovered that her husband is gay.
|
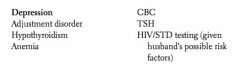
|
|
|
44 yo M presents with fatigue, insomnia, and nightmares about a murder that he witnessed in a mall one year ago. Since then, he has avoided that mall and has not gone out at night.
|
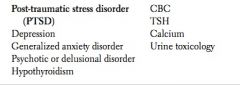
|
|
|
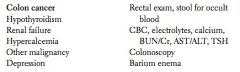
55 yo M presents with fatigue, weight loss, and constipation. He has a family history of colon cancer.
|
|
|
|
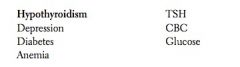
40 yo F presents with fatigue, weight gain, sleepiness, cold intolerance, constipation, and dry skin.
|
|
|
|
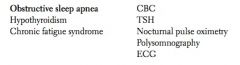
50 yo obese F presents with fatigue and daytime sleepiness. She snores heavily and naps 3–4 times per day but never feels refreshed. She also has hypertension.
|
|
|
|
20 yo M presents with fatigue, thirst, increased appetite, and polyuria.
|

|
|
|
35 yo M policeman c/o feeling tired and sleepy during the day. He changed to the night shift last week.
|

|
|
|
Sore throat - key elems of....
HX PE |
HX
Duration, fever, other ENT symptoms (ear pain, URI), odynophagia, swollen glands, ± cough, rash; sick contacts, HIV risk factors. Key Physical Exam Vital signs; ENT exam, including oral thrush, tonsillar exudate, and lymphadenopathy; lung, abdominal, and skin exams. |
|
|
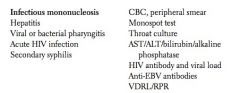
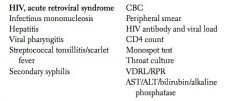
26 yo F presents with sore throat, fever, severe fatigue, and loss of appetite for the past week. She also reports epigastric and LUQ discomfort. She has cervical lymphadenopathy and a rash. Her boyfriend recently experienced similar symptoms.
|
|
|
|
26 yo M presents with sore throat, fever, rash, and weight loss. He has a history of IV drug abuse and sharing needles.
|
|
|
|
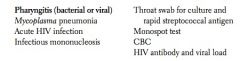
26 yo F presents with fever and sore throat.
|
|
|
|
Cough / SOB - key elems of ....
HX PE |
HX
Acute vs. chronic; presence/description of sputum, associated symptoms (constitutional, URI, postnasal drip, dyspnea, wheezing, chest pain, heartburn, other), exacerbating and alleviating factors; exposures; smoking history; history of lung disease; allergies; medicines (especially ACE inhibitors). Key Physical Exam Vital signs ± pulse oximetry; exam of nasal mucosa, oropharynx, heart, lungs, lymph nodes, and extremi- ties (clubbing, cyanosis, edema). |
|
|
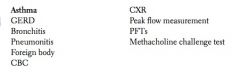
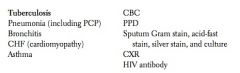
30 yo M presents with shortness of breath, cough, and wheezing that worsen in cold air. He has had several such episodes over the past four months.
|
|
|
|
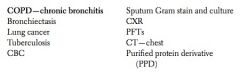
56 yo F presents with shortness of breath, as well as productive cough that has occurred over the past two years for at least three months each year. She is a heavy smoker.
|
|
|
|
58 yo M presents with pleuritic chest pain, fever, chills, and cough with purulent yellow sputum. He is a heavy smoker with COPD.
|
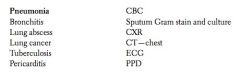
|
|
|
25 yo F presents with two weeks of a nonproductive cough. Three weeks ago she had a sore throat and a runny nose.
|
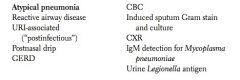
|
|
|
65 yo M presents with worsening cough over the past six months together with hemoptysis, dyspnea, weakness, and weight loss. He is a heavy smoker.
|
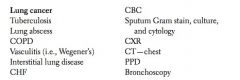
|
|
|
55 yo M presents with increased dyspnea and sputum production over the past three days. He has COPD and stopped using his inhalers last week. He also stopped smoking two days ago.
|
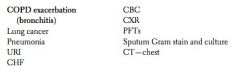
|
|
|
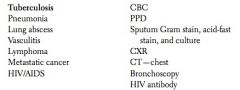
34 yo F nurse presents with worsening cough of six weeks’ duration together with weight loss, fatigue, night sweats, and fever. She has a history of contact with tuberculosis patients at work.
|
|
|
|
35 yo M presents with shortness of breath and cough. He has had unprotected sex with multiple sexual partners and was recently exposed to a patient with active tuberculosis.
|
|
|
|
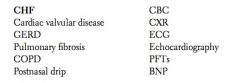
50 yo M presents with cough that is exacerbated by lying down at night and improved by propping up on three pillows. He also reports exertional dyspnea.
|
|
|
|
Chest Pain - Key elems of ...
Hx PE |
HX
Location, quality, severity, radiation, duration, context (exertional, postprandial, positional, cocaine use, trauma), associated symptoms (sweating, nausea, dyspnea, palpitation, sense of doom), exacerbating and alleviating factors (especially medicines); prior history of similar symptoms; known heart or lung disease or history of diagnostic testing; cardiac risk factors (hypertension, hyperlipidemia, smoking, family history of early MI); pulmonary embolism risk factors (history of DVT, coagulopathy, malignancy, recent immo- bilization). Key Physical Exam Vital signs ± BP in both arms; complete cardiovascular exam (JVD, PMI, chest wall tenderness, heart sounds, pulses, edema); lung and abdominal exams. |
|
|
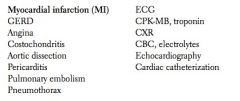
60 yo M presents with sudden onset of substernal heavy chest pain that has lasted for 30 minutes and radiates to the left arm. The pain is accompanied by dyspnea, diaphoresis, and nausea. He has a history of hypertension, hyperlipidemia, and smoking.
|
|
|
|
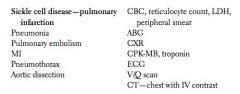
20 yo African-American F presents with acute onset of severe chest pain. She has a history of sickle cell disease and multiple previous hospitalizations for pain and anemia management.
|
|
|
|
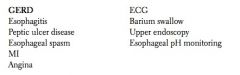
45 yo F presents with a retrosternal burning sensation that occurs after heavy meals and when lying down. Her symptoms are relieved by antacids.
|
|
|
|
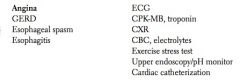
55 yo M presents with retrosternal squeezing pain that lasts for two minutes and occurs with exercise. It is relieved by rest and is not related to food intake.
|
|
|
|
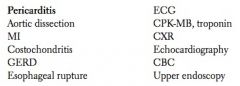
34 yo F presents with retrosternal stabbing chest pain that improves when she leans forward and worsens with deep inspiration. She had a URI one week ago.
|
|
|
|
34 yo F presents with stabbing chest pain that worsens with deep inspiration and is relieved by aspirin. She had a URI one week ago. Chest wall tenderness is noted.
|
|
|
|
70 yo F presents with acute onset of shortness of breath at rest and pleuritic chest pain. She also presents with tachycardia, hypotension, tachypnea, and mild fever. She is recovering from hip replacement surgery.
|
|
|
|
55 yo M presents with sudden onset of severe chest pain that radiates to the back. He has a history of uncontrolled hypertension.
|
|
|
|
Palpitations - key elems of ....
HX PE |
Hx
Gradual vs. acute onset/offset, context (exertion, caffeine, anxiety), associated symptoms (lightheaded- ness, chest pain, dyspnea); hyperthyroid symptoms; history of bleeding or anemia; history of heart disease. Key Physical Exam Vital signs; endocrine/thyroid exam, including exophthalmos, lid retraction, lid lag, gland size, bruit, and tremor; complete cardiovascular exam. |
|
|
70 yo diabetic M presents with episodes of palpitations and diaphoresis. He is on insulin.
|
|
|
|
Wt Loss - key elem of ....\
HX PE |
HX
Amount, duration, ± intentional; diet history, body image, anxiety or depression; other constitutional symptoms; palpitation, tremor, diarrhea, family history of thyroid disease; HIV risk factors; alcohol and drug use; medications; history of cancer. Key Physical Exam Vital signs; complete physical. |
|
|
42 yo F presents with a 7-kg weight loss over the past two months. She has a fine tremor, and her pulse is 112.
|
|
|
|
Wt gain - key elems of ....
HX PE |
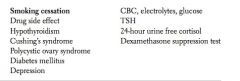
HX
Amount, duration, timing (relation to medication changes, smoking cessation, depression); diet history; hypothyroid symptoms (fatigue, constipation, skin/hair/nail changes); menstrual irregularity; past med- ical history; alcohol and drug use. Key Physical Exam Vital signs; complete exam, including signs of Cushing’s syndrome (hypertension, central obesity, moon face, buffalo hump, supraclavicular fat pads, purple abdominal striae). |
|
|
44 yo F presents with a weight gain of
> 11 kg over the past two months. She quit smoking three months ago and is on amitriptyline for depression. She also reports cold intolerance and constipation. |
|
|
|
Dysphagia - key elems of ....
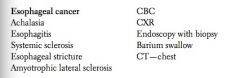
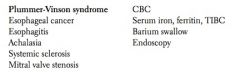
HX PE |
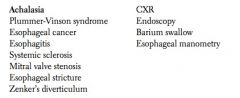
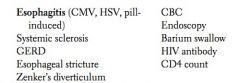
HX
Solids vs. both solids and liquids, ± progressive, constitutional symptoms (especially weight loss), drooling, re- gurgitation, odynophagia, GERD symptoms; medications; HIV risk factors, history of smoking, history of Raynaud’s phenomenon. Key Physical Exam Vital signs; head and neck exam; heart, lung, and abdominal exams; skin exam (for signs of sclero- derma/CREST). |
|
|
75 yo M presents with dysphagia that started with solids and progressed to liquids. He is an alcoholic and a heavy smoker. He has had an unintentional weight loss of 7 kg over the past four months.
|
|
|
|
45 yo F presents with dysphagia for two weeks together with fatigue and a craving for ice and clay.
|
|
|
|
48 yo F presents with dysphagia for both solid and liquid foods that has slowly progressed in severity over the past year. It is associated with regurgitation of undigested food, especially at night.
|
|
|
|
38 yo M presents with dysphagia and pain on swallowing solids more than liquids. Exam reveals oral thrush.
|
|
|
|
Nausea / vomiting - key elems of
HX PE |
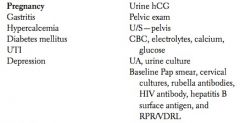
HX
Acuity of onset, ± abdominal pain, relation to meals, sick contacts, possible food poisoning, possible pregnancy; neurologic symptoms (headache, stiff neck, vertigo, focal numbness or weakness), other asso- ciated symptoms (GI, chest pain), exacerbating and alleviating factors; medications. Key Physical Exam Vital signs; ENT; consider funduscopic exam (increased intracranial pressure); complete abdominal exam; consider heart, lung, and rectal exams. |
|
|
20 yo F presents with nausea, vomiting (especially in the morning), fatigue, and polyuria. Her last menstrual period was six weeks ago, and her breasts are full and tender. She is sexually active with her boyfriend, and they use condoms for contraception.
|
|
|
|
ABD Pain - key elems of ....
HX PE |
HX
Location, quality, intensity, duration, radiation, timing (relation to meals), associated symptoms (constitu- tional, GI, cardiac, pulmonary, renal, pelvic, other), exacerbating and alleviating factors; prior history of similar symptoms; history of abdominal surgeries, gallstones, renal stones, atherosclerotic vascular dis- ease; medications; alcohol and drug use; domestic violence. Key Physical Exam Vital signs; heart and lung exams; abdominal exam, including guarding, rebound, Murphy’s sign, and CVA palpation; rectal exam; pelvic exam (women). |
|
|
45 yo M presents with sudden onset of colicky right-sided flank pain that radiates to the testicles, accompanied by nausea, vomiting, hematuria, and CVA tenderness.
|
|
|
|
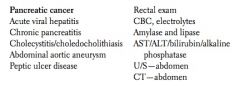
60 yo M presents with dull epigastric pain that radiates to the back, together with weight loss, dark urine, and clay- colored stool. He is a heavy drinker and smoker.
|
|
|
|
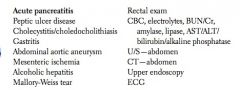
56 yo M presents with severe midepigastric abdominal pain that radiates to the back and improves when he leans forward. He also reports anorexia, nausea, and vomiting. He is an alcoholic and has spent the past three days binge drinking.
|
|
|
|
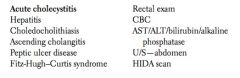
41 yo obese F presents with RUQ abdominal pain that radiates to the right scapula and is associated with nausea, vomiting, and a fever of 101.5°F. The pain started after she had eaten fatty food. She has had similar but less intense episodes that lasted a few hours. Exam reveals positive Murphy’s sign.
|
|
|
|
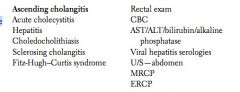
43 yo obese F presents with RUQ abdominal pain, fever, and jaundice. She was diagnosed with asymptomatic gallstones one year ago.
|
|
|
|
25 yo M presents with RUQ pain, fever, anorexia, nausea, and vomiting. He has dark urine and clay-colored stool.
|
|
|
|
35 yo M presents with burning epigastric pain that starts 2–3 hours after meals. The pain is relieved by food and antacids.
|
|
|
|
37 yo M presents with severe epigastric pain, nausea, vomiting, and mild fever. He appears toxic. He has a history of intermittent epigastric pain that is relieved by food and antacids. He also smokes heavily and takes aspirin on a regular basis.
|
|
|
|
18 yo M boxer presents with severe LUQ abdominal pain that radiates to the left scapula. He had infectious mononucleosis three weeks ago.
|
|
|
|
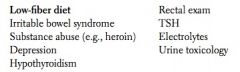
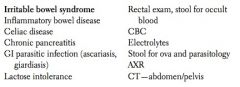
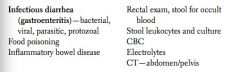
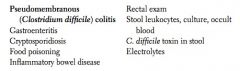
Constipation/Dhea - key elems of ....]
HX PE |
HX
Frequency and volume of stools, duration of change in bowel habits, associated symptoms (constitu- tional, abdominal pain, bloating, sense of incomplete evacuation, melena or hematochezia); thyroid dis- ease symptoms; diet (especially fiber and fluid intake); medications (including recent antibiotics); sick contacts, travel, camping, HIV risk factors; history of abdominal surgeries, diabetes, pancreatitis; alcohol and drug use; family history of colon cancer. Key Physical Exam Vital signs; relevant thyroid/endocrine exam; abdominal and rectal exams; ± female pelvic exam. |
|
|
40 yo M presents with crampy abdominal pain, vomiting, abdominal distention, and inability to pass flatus or stool. He has a history of multiple abdominal surgeries.
|
|
|
|
70 yo F presents with acute onset of severe, crampy abdominal pain. She recently vomited and had a massive dark bowel movement. She has a history of CHF and atrial fibrillation, for which she has received digitalis. Her pain is out of proportion to the exam.
|
|
|
|
21 yo F presents with acute onset of severe RLQ pain, nausea, and vomiting. She has no fever, urinary symptoms, or vaginal bleeding and has never taken OCPs. Her last menstrual period was regular, and she has no history of STDs.`
|
|
|
|
68 yo M presents with lower LLQ abdominal pain, fever, and chills for the past three days. He also reports recent onset of alternating diarrhea and constipation. He consumes a low-fiber, high-fat diet.
|
|
|
|
20 yo M presents with severe RLQ abdominal pain, nausea, and vomiting. His discomfort started yesterday as a vague pain around the umbilicus. As the pain worsened, it became sharp and migrated to the RLQ. McBurney’s and psoas signs are positive.
|
|
|
|
30 yo F presents with periumbilical pain for six months. The pain never awakens her from sleep. It is relieved by defecation and worsens when she is upset. She has alternating constipation and diarrhea but no nausea, vomiting, weight loss, or anorexia.
|
|
|
|
24 yo F presents with bilateral lower abdominal pain that started with the first day of her menstrual period. The pain is associated with fever and a thick, greenish-yellow vaginal discharge. She has had unprotected sex with multiple sexual partners.
|
|
|
|
67 yo M presents with alternating diarrhea and constipation, decreased stool caliber, and blood in the stool for the past eight months. He also reports unintentional weight loss. He is on a low- fiber diet and has a family history of colon cancer.
|
|
|
|
28 yo M presents with constipation (very hard stool) for the last three weeks. Since his mother died two months ago, he and his father have eaten only junk food.
|
|
|
|
30 yo F presents with alternating constipation and diarrhea and abdominal pain that is relieved by defecation. She has no nausea, vomiting, weight loss, or blood in her stool.
|
|
|
|
33 yo M presents with watery diarrhea, vomiting, and diffuse abdominal pain that began yesterday. He also reports feeling hot. Several of his coworkers are also ill.
|
|
|
|
40 yo F presents with watery diarrhea and abdominal cramps. Last week she was on antibiotics for a UTI.
|
|
|
|
25 yo M presents with watery diarrhea and abdominal cramps. He was recently in Mexico.
|
|
|
|
30 yo F presents with watery diarrhea and abdominal cramping and bloating. Her symptoms are aggravated by milk ingestion and are relieved by fasting.
|
|
|
|
33 yo M presents with watery diarrhea, diffuse abdominal pain, and weight loss over the past three weeks. He has not responded to antibiotics.
|
|
|
|
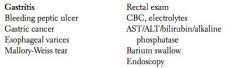
UGI Blee - key elems of
HX PE |
HX
Amount, duration, context (after severe vomiting, alcohol ingestion, nosebleed), associated symptoms (constitutional, nausea, abdominal pain, dyspepsia); medications (especially warfarin, NSAIDs); history of peptic ulcer disease, liver disease, abdominal aortic aneurysm repair, easy bleeding. Key Physical Exam Vital signs, including orthostatics; ENT, heart, lung, abdominal, and rectal exams. |
|
|
45 yo F presents with coffee-ground emesis for the last three days. Her stool is dark and tarry. She has a history of intermittent epigastric pain that is relieved by food and antacids.
|
|
|
|
40 yo F presents with epigastric pain and coffee-ground emesis. She has a history of rheumatoid arthritis that has been treated with aspirin. She is an alcoholic.
|
|
|
|
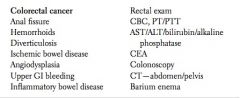
Blood in stool - key elems of
HX PE |
Hx
Melena vs. bright blood; amount, duration, associated symptoms (constitutional, abdominal or rectal pain, tenesmus, constipation/diarrhea); trauma; prior history of similar symptoms; prior colonoscopy; medications (especially warfarin); history of easy bleeding or atherosclerotic vascular disease. Key Physical Exam Vital signs ± orthostatics; abdominal and rectal exams. |
|
|
67 yo M presents with blood in his stool, weight loss, and constipation. He has a family history of colon cancer.
|
|
|
|
33 yo F presents with rectal bleeding and diarrhea for the past week. She has had lower abdominal pain and tenesmus for several months.
|
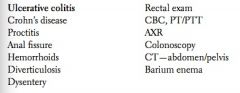
|
|
|
58 yo M presents with bright red blood per rectum and chronic constipation. He consumes a low-fiber diet.
|
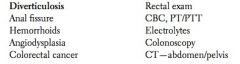
|
|
|
Hematuria - key elems of...
HX PE |
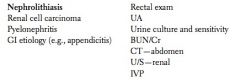
HX
Amount, duration, ± clots, associated symptoms (constitutional, renal colic, dysuria, irritative voiding symptoms); medications; history of vigorous exercise, trauma, smoking, stones, cancer, or easy bleeding. Key Physical Exam Vital signs; lymph nodes; abdominal exam; genitourinary and rectal exams; extremities. |
|
|
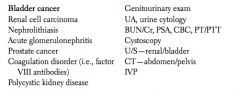
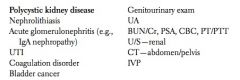
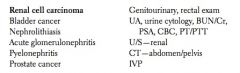
65 yo M presents with painless hematuria. He is a heavy smoker and works as a painter.
|
|
|
|
35 yo M presents with painless hematuria. He has a family history of kidney problems.
|
|
|
|
55 yo M presents with flank pain and blood in his urine without dysuria. He has experienced weight loss and fever over the past two months.
|
|
|
|
other urinary s/s - key elems of...
HX PE |
HX
Duration, obstructive symptoms (hesitancy, diminished stream, sense of incomplete bladder emptying, straining, postvoid dribbling), irritative symptoms (urgency, frequency, nocturia), constitutional symp- toms; bone pain; medications; history of UTIs, urethral stricture, or urinary tract instrumentation; stones, diabetes, alcoholism. Key Physical Exam Vital signs; abdominal exam (including suprapubic percussion to assess for a distended bladder); genital and rectal exams; focused neurologic exam. |
|
|
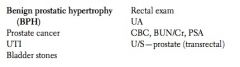
60 yo M presents with nocturia, urgency, weak stream, and terminal dribbling. He denies any weight loss, fatigue, or bone pain. He has had two episodes of urinary retention that required catheterization.
|
|
|
|
71 yo M presents with nocturia, urgency, weak stream, terminal dribbling, hematuria, and lower back pain over the past four months. He has also experienced weight loss and fatigue.
|

|
|
|
18 yo M presents with a burning sensation during urination and urethral discharge. He recently had unprotected sex with a new partner.
|
|
|
|
45 yo diabetic F presents with dysuria, urinary frequency, fever, chills, and nausea over the past three days. There is left CVA tenderness on exam.
|
|
|
|
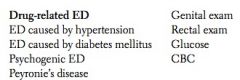
ED (limp noodle) - key elems of....
HX PE |
HX
Duration, severity, ± nocturnal erections, libido, stress or depression, trauma, associated incontinence; medications (and recent changes); past medical history (hypertension, diabetes, high cholesterol, known atherosclerotic vascular disease, prior prostate surgery); smoking, alcohol and drug use. Key Physical Exam Vital signs; cardiovascular exam; genital and rectal exams. |
|
|
47 yo M presents with impotence that started three months ago. He has hypertension and was started on atenolol four months ago. He also has diabetes and is on insulin.
|
|
|
|
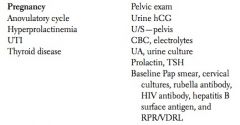
Amenorhea - key elems of ...
HX PE |
HX
Primary vs. secondary, duration, possible pregnancy, associated symptoms (headache, decreased periph- eral vision, galactorrhea, hirsutism, virilization, hot flushes, vaginal dryness, symptoms of thyroid dis- ease); history of anorexia nervosa, excessive dieting, vigorous exercise, pregnancies, D&Cs, uterine infec- tions; drug use; medications. Key Physical Exam Vital signs; breast exam; complete pelvic exam. |
|
|
40 yo F presents with amenorrhea, morning nausea and vomiting, fatigue, and polyuria. Her last menstrual period was six weeks ago, and her breasts are full and tender. She uses the rhythm method for contraception.
|
|
|
|
23 yo obese F presents with amenorrhea for six months, facial hair, and infertility for the past three years.
|
|
|
|
35 yo F presents with amenorrhea, galactorrhea, visual field defects, and headaches for the past six months.
|
|
|
|
48 yo F presents with amenorrhea for the past six months accompanied by hot flushes, night sweats, emotional lability, and dyspareunia.
|
|
|
|
35 yo F presents with amenorrhea, cold intolerance, coarse hair, weight loss, and fatigue. She has a history of abruptio placentae followed by hypovolemic shock and failure of lactation two years ago.
|
|
|
|
18 yo F presents with amenorrhea for the past four months. She has lost 95 pounds and has a history of vigorous exercise and cold intolerance.
|
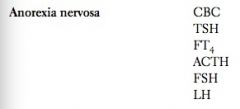
|
|
|
29 yo F presents with amenorrhea for the past six months. She has a history of occasional palpitation and dizziness. She lost her fiancé in a car accident.
|
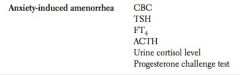
|
|
|
Vaginal bleeding - key elems of ...
HX PE |
HX
Pre- vs. postmenopausal, duration, amount; menstrual history and relation to last menstrual period; asso- ciated discharge, pelvic or abdominal pain, or urinary symptoms; trauma; medications (especially war- farin, contraceptives); history of easy bleeding or bruising; history of abnormal Pap smears. Key Physical Exam Vital signs; abdominal exam; complete pelvic exam. |
|
|
17 yo F presents with prolonged, excessive menstrual bleeding occurring irregularly over the past six months.
|
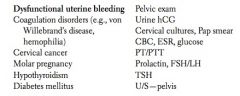
|
|
|
61 yo obese F presents with profuse vaginal bleeding over the past month. Her last menstrual period was 10 years ago. She has a history of hypertension and diabetes mellitus. She is nulliparous.
|
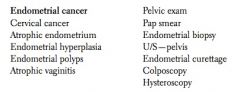
|
|
|
45 yo G5P5 F presents with postcoital bleeding. She is a cigarette smoker and takes OCPs.
|
|
|
|
28 yo F who is eight weeks pregnant presents with lower abdominal pain and vaginal bleeding.
|
|
|
|
32 yo F presents with sudden onset of left lower abdominal pain that radiates to the scapula and back and is associated with vaginal bleeding. Her last menstrual period was five weeks ago. She has a history of PID and unprotected intercourse.
|
|
|
|
Vaginal Discharge - key elems of ...
HX PE |
HX
Amount, color, consistency, odor, duration; associated vaginal burning, pain, or pruritus; recent sexual activity; onset of last menstrual period; use of contraceptives, tampons, and douches; history of similar symptoms; history of STD. Key Physical Exam Vital signs; abdominal exam; complete pelvic exam. |
|
|
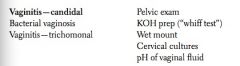
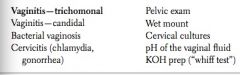
28 yo F presents with a thin, grayish- white, foul-smelling vaginal discharge.
|
|
|
|
30 yo F presents with a thick, white, cottage cheese–like, odorless vaginal discharge and vaginal itching.
|
|
|
|
35 yo F presents with a malodorous, profuse, frothy, greenish vaginal discharge with intense vaginal itching and discomfort.
|
|
|
|
Dyspareunia - key elems of ....
HX PE |
HX
Duration, timing, associated symptoms (vaginal discharge, rash, painful menses, GI symptoms, hot flushes), adequacy of lubrication; libido; sexual history; history of sexual trauma or domestic violence; history of endometriosis, PID, or prior abdominal/pelvic surgeries. Key Physical Exam Vital signs; abdominal exam; complete pelvic exam. |
|
|
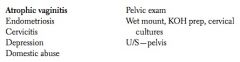
54 yo F c/o painful intercourse. Her last menstrual period was nine months ago. She has hot flushes.
|
|
|
|
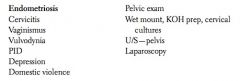
37 yo F presents with dyspareunia, inability to conceive, and dysmenorrhea.
|
|
|
|
Abuse - key elems of...
HX PE |
Hx
Establish confidentiality; directly question about physical, sexual, or emotional abuse and about fear, safety, backup plan; history of frequent accidents/injuries, mental illness, drug use; firearms in the home. Key Physical Exam Vital signs; complete exam ± pelvic. |
|
|
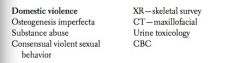
28 yo F c/o multiple facial and bodily injuries. She claims that she fell on the stairs. She was hospitalized for some physical injuries seven months ago. She presents with her husband.
|
|
|
|
30 yo F presents with multiple facial and physical injuries. She was attacked and raped by two men.
|
|
|
|
Jt / Limb pain - key elems of...
HX PE |
HX
Location, quality, intensity, duration, pattern (small vs. large joints, number involved; swelling, redness, warmth), associated symptoms (constitutional, red eye, oral or genital ulceration, diarrhea, dysuria, rash, focal numbness/weakness), exacerbating and alleviating factors; trauma (including vigorous exercise); medications; DVT risk factors; alcohol and drug use; family history of rheumatic disease. Key Physical Exam Vital signs; HEENT and musculoskeletal exams; relevant neurovascular exam. |
|
|
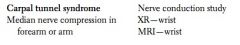
30 yo F presents with wrist pain and a black eye after tripping, falling, and hitting her head on the edge of a table. She looks anxious and gives an inconsistent story.
|

|
|
|
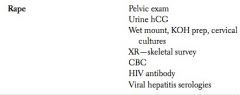
30 yo F secretary presents with wrist pain and a sensation of numbness and burning in her palm and the first, second, and third fingers of her right hand. The pain worsens at night and is relieved by loose shaking of the hand. There is sensory loss in the same fingers. Exam reveals positive Tinel’s sign.
|
|
|
|
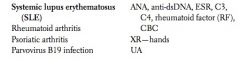
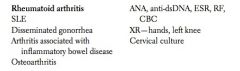
28 yo F presents with pain in the interphalangeal joints of her hands together with hair loss and a butterfly rash on the face.
|
|
|
|
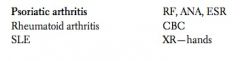
28 yo F presents with pain in the metacarpophalangeal joints of both hands. Her left knee is also painful and red. She has morning joint stiffness that lasts for an hour. Her mother had rheumatoid arthritis.
|
|
|
|
18 yo M presents with pain in the interphalangeal joints of both hands. He also has scaly, salmon-pink lesions on the extensor surface of his elbows and knees.
|
|
|
|
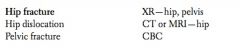
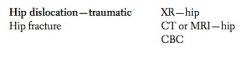
65 yo F presents with inability to use her left leg and bear weight on it after tripping on a carpet. Onset of menopause was 20 years ago, and she did not receive HRT or calcium supplements. Her left leg is externally rotated, shortened, and adducted, and there is tenderness in her left groin.
|
|
|
|
40 yo M presents with pain in the right groin after a motor vehicle accident. His right leg is flexed at the hip, adducted, and internally rotated.
|
|
|
|
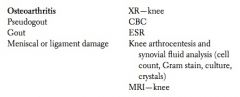
56 yo obese F presents with right knee stiffness and pain that increases with movement. Her symptoms have gradually worsened over the past 10 years. She noticed swelling and deformity of the joint and is having difficulty walking.
|
|
|
|
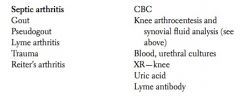
45 yo M presents with right knee pain with swelling and redness.
|
|
|
|
65 yo M presents with right foot pain. He has been training for a marathon.
|

|
|
|
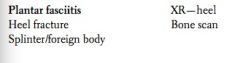
65 yo M presents with pain in the heel of the right foot that is most notable with his first few steps and then improves as he continues walking. He has no known trauma.
|
|
|
|
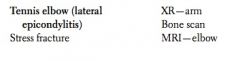
55 yo M presents with pain in the elbow when he plays tennis. His grip is impaired as a result of the pain. There is tenderness over the lateral epicondyle as well as pain on resisted wrist dorsiflexion with the elbow in extension.
|
|
|
|
27 yo F presents with painful wrists and elbows, a swollen and hot knee joint that is painful on flexion, a rash on her limbs, and vaginal discharge. She is sexually active with multiple partners and occasionally uses condoms.
|
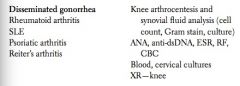
|
|
|
60 yo F presents with pain in both legs that is induced by walking and is relieved by rest. She had cardiac bypass surgery six months ago and continues to smoke heavily.
|
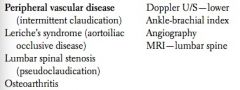
|
|
|
45 yo F presents with right calf pain. Her calf is tender, warm, red, and swollen compared to the left side. She was started on OCPs two months ago for dysfunctional uterine bleeding.
|
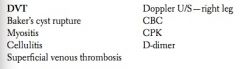
|
|
|
50 yo M presents with right shoulder pain after falling onto his outstretched hand while skiing. He noticed deformity of his shoulder and had to hold his right arm.
|

|
|
|
55 yo M presents with crampy bilateral thigh and calf pain, fatigue, and dark urine. He is on simvastatin and clofibrate for hyperlipidemia.
|
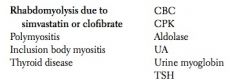
|
|
|
Low back pain - key elems of...
HX PE |
HX
Location, quality, intensity, radiation, context (moving furniture, bending/twisting, trauma), timing (dis- turbs sleep), associated symptoms (especially constitutional, incontinence), exacerbating and alleviating factors; history of cancer, recurrent UTIs, diabetes, renal stones, IV drug use, smoking. Key Physical Exam Vital signs; neurologic exam (especially L4–S1 nerve roots); back palpation and range of motion (al- though rarely of diagnostic utility); hip exam (can refer pain to the back); consider rectal exam. |
|
|
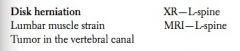
45 yo F presents with low back pain that radiates to the lateral aspect of her left foot. Straight leg raising is positive. The patient is unable to tiptoe.
|
|
|
|
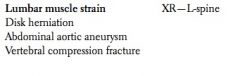
45 yo F presents with low back pain that started after she cleaned her house. The pain does not radiate, and there is no sensory deficit or weakness in her legs. Paraspinal muscle tenderness and spasm are also noted.
|
|
|
|
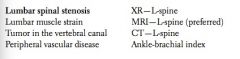
45 yo M presents with pain in the lower back and legs during prolonged standing and walking. The pain is relieved by sitting and leaning forward (e.g., pushing a grocery cart).
|
|
|
|
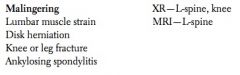
7 yo M presents with low back pain that radiates to the left leg and began after he fell on his knee during gym class. He also describes areas of loss of sensation in his left foot. The pain and sensory loss do not match any known distribution. He insists on requesting a week off from school because of his injury.
|
|
|
|
Child w/ fever ((No child will be present; only the mother will be present to tell the story.)
Key elems of ... HX PE |
Key History
Severity, duration, associated localizing symptoms, appetite, rash, sick contacts, day care, immunizations, past history. Key Physical Exam Vital signs; HEENT, neck, heart, lung, abdominal, and skin exams. |
|
|
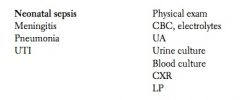
20-day-old M presents with fever, decreased breast-feeding, and lethargy. He was born at 36 weeks as a result of premature rupture of membranes.
|
|
|
|
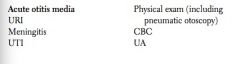
3 yo M presents with a two-day history of fever and pulling on his right ear. He is otherwise healthy, and his immunizations are up to date. His older sister recently had a cold. The child attends a day care center.
|
|
|
|
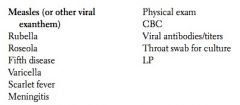
12-month-old M presents with fever for the last two days accompanied by a maculopapular rash on his face and body. He has not yet received the MMR vaccine.
|
|
|
|
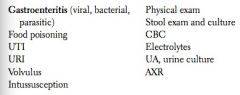
4 yo M presents with diarrhea, vomiting, lethargy, weakness, and fever. The child attends a day care center where several children have had similar symptoms.
|
|

